Pulmonary oedema: Why does pulmonary oedema occur? Is it a common cause of death?
Pulmonary oedema is a serious and life-threatening condition if it occurs suddenly (acutely). Its chronic form is milder. It can be caused by chest trauma, pneumonia, drowning or inhalation of a foreign body. It is more common as a consequence of heart failure in the elderly population. It can also develop in pregnancy during eclampsia. Symptoms include breathlessness and other discomforts.
It is also colloquially referred to as water on the lungs.
It can be detected by certain symptoms. One example is shortness of breath, which is a feeling of difficulty breathing or not breathing enough. Breathing may also be faster, accompanied by coughing and expectoration.
In more severe cases, and especially in the acute form, it is also externally manifested by marked shortness of breath, audible gurgling or grunting when breathing, coughing or coughing up pink and foamy fluid.
What are the causes of pulmonary oedema?
Pulmonary oedema can occur due to several causes. It is divided into main groups, according to the mechanism of occurrence. Namely, for impaired permeability (permeability of blood vessels and tissues), for increased hydrostatic pressure in the pulmonary vessels, for decreased oncotic pressure, as well as for other more complex causes.
permeability disorder occurs when:
- Inflammation
- aspiration (inhalation) of a foreign body or vomit
- irritation by toxic gases, chemicals
- inhalation trauma, i.e. burns, inhalation of combustion products
- allergic reaction
- clotting disorders such as disseminated intravascular coagulopathy
- renal failure
- radiation
An increase in hydrostatic pressure occurs in:
- left heart failure
- valvular defect in the left side of the heart
- blockage or obstruction of the pulmonary veins
- high blood flow through the lungs
Reduced oncotic pressure means that there is a low amount of albumin (a protein that holds fluid in the circulating blood) in the blood. This condition occurs, for example, in starvation, anorexia and other eating disorders.
Complex causes also include:
- pulmonary embolism
- eclampsia
- chronic hypoxia (prolonged low oxygen levels)
- neurogenic pulmonary oedema (does not mean psychologically induced pulmonary oedema)
- heroin overdose
Cardiovascular causes of water on the lungs
Very often, pulmonary oedema occurs as a result of problems with the cardiovascular system. Problems can also be caused by long-term untreated hypertension. A typical example is the failure of the left heart. The heart is divided into two halves. Each half is composed of an atrium and a ventricle.
Our tip.
The right ventricle discharges blood into the small, or pulmonary, circulation. There, the blood is oxygenated and then flows through the left atrium into the left ventricle. The left ventricle pumps blood to the aorta and from there to the whole body. If the synergy of the heart's chambers is disrupted, a problem occurs.
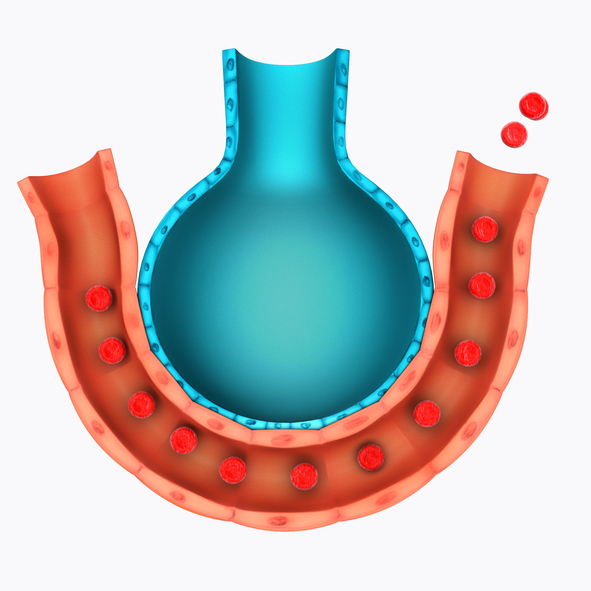
When the left ventricle fails, blood accumulates in the left heart region and subsequently in the pulmonary circulation. This results in an increase in hydrostatic pressure, with preserved right ventricular function, and increased fluid transfer from the vessels to the pulmonary space.

As a consequence, symptoms indicative of pulmonary oedema include:
- shortness of breath
- impaired breathing when lying down, during sleep, propping up several pillows and sleeping in a semi-sitting position
- cough, irritating, dry at the beginning
- in severe oedema, gurgling or hoarseness
- coughing up foamy and pink fluid
- pallor
- restlessness
- facial expression of fear of death
A similar mechanism occurs when there is a malfunction of the valves located in the left side of the heart or between the left ventricle and the aorta. Increased fluid pressure in the lungs can also occur when there is high blood flow through the lungs.
This can be the result of overhydration of the body, especially when infusion of solutions into the veins is increased. The heart cannot pump the increased volume of blood at that time.
Acute heart diseases that can manifest themselves as swelling of the lungs include myocardial infarction (heart muscle infarction). This involves blockage of a blood vessel that supplies oxygen and nutrients to the heart muscle.
The blockage may be due to atherosclerosis, thrombosis or embolism (blockage by a blood clot). Myocardial infarction is an acute ischaemic heart disease. Usually one of the heart (coronary) arteries becomes blocked.
This restricts or stops the blood flow to the heart muscle. The heart muscle tissue subsequently dies due to lack of oxygen.
Our tip: For more information, see the magazine article First Aid for Myocardial Infarction.
Edema also occurs, for example, in hypertrophic cardiomyopathy, which is a primary disease of the heart muscle. The disease consists of a reduced ability to contract or dilate the myocardium and can take various forms, such as hypertrophic, closed or dilated.
Typical symptoms of this disease include:
- thickening or stretching of the musculature of the heart
- insufficient pumping of blood to the body
- excessive blood supply to the pulmonary circulation
- irregular heartbeat
- shortness of breath
- chest pain
Vascular causes include blockage of the pulmonary veins or pulmonary embolism. In pulmonary embolism, blockage of the blood vessels in the pulmonary circulation occurs. Up to 70-90% of cases are caused by disease of the veins of the lower limbs. More precisely, this disease is referred to as deep vein thrombosis of the lower limbs.
One of the symptoms may be swelling of the limb. Similar to heart failure, but in this case there is swelling in both limbs. In pulmonary embolism, the symptoms depend on the extent of the involvement of the pulmonary circulation.
Symptoms in pulmonary embolism depend on the extent of the closure. For example:
- rapid breathing
- shortness of breath (dyspnoea)
- chest pain
- pulmonary oedema in heart failure
- death in severe pulmonary embolism
Problem with the respiratory system
Even with a few problems within the respiratory system, swelling of the lungs can occur. This can occur, for example, with long-term bronchitis. Especially with associated complications.
Very often, problems also arise when chronic bronchitis leads to chronic obstructive pulmonary disease. This is accompanied by a deterioration of the heart, which results in swelling of the lower limbs, but also in swelling of the lungs.
Another acute form of lung involvement is acute respiratory distress syndrome, technically known as ARDS. The disease is inflammatory. It is a diffuse alveolar involvement where pulmonary oedema occurs due to increased permeability of the capillaries.
Very often this disease occurs as a consequence of severe trauma, also as a result of lung infections, but also as a result of water penetration into the lungs, for example after drowning.
Inhalation of toxic fumes or inhalation of vomit or other foreign body is dangerous. Acute reactions cause increased permeability of the fluid. These acute conditions are serious and require immediate treatment. Otherwise, death is also imminent.
Other causes of water on the lungs
Edema also occurs in severe anaphylactic shock, i.e. a widespread allergic reaction. Also in poisoning with certain drugs or in renal and hepatic failure. Another example is severe alcohol intoxication.
It can also develop in chest trauma, pneumothorax, traumatic shock, but also in prolonged compression syndrome (rhabdomyolysis, also known as crush syndrome).
Read also: what the word shock means in medicine.
Other complex causes include eclampsia, which is actually a late form of gestosis. It threatens the life of both the fetus and the mother, and is an indication for early termination of pregnancy.
A particular example is altitude sickness. Altitude sickness is related to lack of oxygen at high altitudes and to air pressure. Acute altitude sickness can occur at altitudes as low as 2500-6000 metres.
It occurs mainly in people who do not follow the rules of ascent and advance too fast. The symptoms of the disease include the appearance of at least one symptom along with a headache.

Symptoms of acute altitude sickness, headache is associated with:
- Fatigue
- weakness
- apathy
- insomnia
- apnoeic pauses during sleep
- nausea
- lack of appetite
- rapid pulse
- shortness of breath
- swelling of the limbs
- reduced urine production, i.e. reduced urination in 24 hours
These symptoms appear 6 to 48 hours after reaching altitude. At what altitude is individual. Symptoms can be mild but also intense. A complication of altitude sickness is altitude cerebral oedema and altitude pulmonary oedema.
In altitude pulmonary edema, symptoms such as:
- dyspnoea at rest.
- rapid breathing rate
- blue discolouration of the skin (cyanosis)
- dry cough
- coughing up foamy pink fluid, mucus
- gurgling, hoarseness of breathing
- inability to lie down due to shortness of breath
- chest pain
- fever
- vomiting
- reduced urination
Treatment for mountain sickness has a sequence. Immediate descent or transport, oxygen administration, medication and pressurisation are required.
How to help with pulmonary oedema?
First aid involves calling for professional help, i.e. emergency medical services. Cooperation with the emergency operator is important.
It's important to remain calm. That means complete physical calm, no exertion and not a single step. It's also important to calm down mentally. The position is very important. It must be sitting or semi-sitting. It's best if the lower limbs are lowered off the bed.
Tight clothing, such as a tie, shirt or belt, should be loosened. Ventilation of the air in the room should ensure a greater supply of oxygen.
Video about pulmonary edema
Diseases with symptom "Lung Island"
- Anaphylactic shock
- Aortic diseases
- Atrial and ventricular septal defect
- Burns
- Cardiac tamponade
- Cardiogenic shock
- Cardiomyopathy
- Congenital Cardiac Defects
- Endocarditis
- Heart failure
- Heart Tumors
- Heart valve disease
- High Blood Pressure
- Hypertensive crisis
- Ischemic heart disease
- Kidney inflammation
- Liver failure
- Myocardial infarction
- Myocarditis
- Pneumonia
- Pulmonary hypertension
- Shock - State of shock
- Mor
Interesting resources










