- Hoare Z, Lim WS (May 2006). "Pneumonia: update on diagnosis and management". BMJ. 332 (7549): 1077–9.
- Ruuskanen O, Lahti E, Jennings LC, Murdoch DR (April 2011). "Viral pneumonia". Lancet. 377 (9773): 1264–75.
- Lodha R, Kabra SK, Pandey RM (June 2013). "Antibiotics for community-acquired pneumonia in children". The Cochrane Database of Systematic Reviews. 6 (6): CD004874.
- Leach RE (2009). Acute and Critical Care Medicine at a Glance (2nd ed.). Wiley-Blackwell. ISBN 978-1-4051-6139-8.
- Lowe JF, Stevens A (2000). Pathology (2nd ed.). St. Louis: Mosby. p. 197. ISBN 978-0-7234-3200-5.
- Bowden RA, Ljungman P, Snydman DR, eds. (2010). Transplant infections. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. ISBN 978-1-58255-820-2.
- George RB (2005). Chest medicine : essentials of pulmonary and critical care medicine (5th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 353. ISBN 978-0-7817-5273-2.
- Eddy, Orin (December 2005). "Community-Acquired Pneumonia: From Common Pathogens To Emerging Resistance". Emergency Medicine Practice. 7 (12).
- Tintinalli JE (2010). Emergency Medicine: A Comprehensive Study Guide (Emergency Medicine (Tintinalli)). New York: McGraw-Hill Companies. p. 480
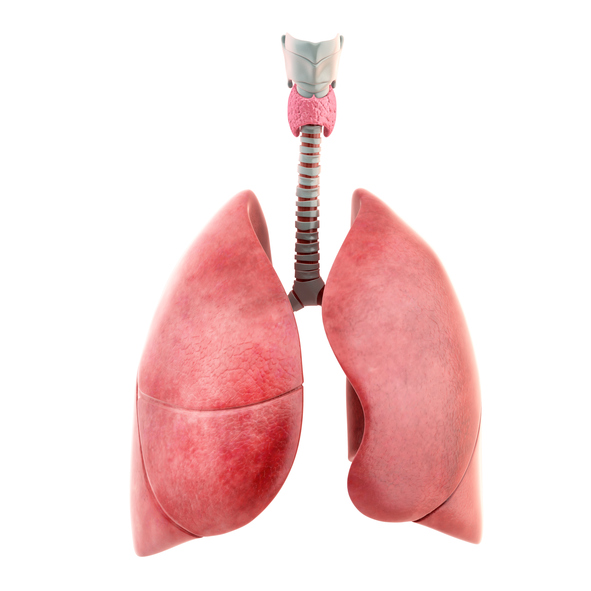
Pneumonia: Symptoms and Classification

Pneumonia is an inflammatory disease characterized by lung tissue damage. Depending on the origin of the disease, this inflammation can take both an infectious and a non-infectious form.
Most common symptoms
- Muscle Pain
- Malaise
- Chest pain
- Right Flank Pain
- Headache
- Sore Throat
- Joint Pain
- Limb pain
- Hoarseness
- Fever
- Spirituality
- Blue leather
- Indigestion
- Nausea
- Lung Island
- Dry cough
- Pressure on the chest
- Tremors
- Fatigue
- Damp cough
- Vomiting
- Coughing up mucus
- Coughing up blood
- Winterreise
- Accelerated heart rate
- Increased body temperature
Characteristics
Pneumonia is an inflammation of the lung parenchyma. Infectious pneumonia is more common.
However, the course as well as the severity of this respiratory disease depends not only on the origin of the inflammation, but also on the general condition of the person and the possible state of immunity, which has a great contribution to the course of treatment.
It is usually acute, i.e. sudden, but can also be chronic. The causative agent of the disease is usually a droplet infection. It spreads mainly from the upper respiratory tract.
Non-infectious pneumonias are also less common and can be caused by allergic reactions and physical or chemical exposure. Pneumonia is one of the most common inflammatory diseases.
Pneumonia is classified by several criteria. It can take different forms, for example, the infectious form can be caused by bacteria, viruses, fungi. However, the most common are bacterial inflammations, which arise from the penetration through the oral cavity and upper respiratory tract. Least common are inflammations caused by infection with fungi or molds.
Non-infectious inflammation is characterised by an inflammatory response even without an infection, for example when chemicals, gases or fluids enter the lungs. However, there is a risk if this type of inflammation is accompanied by infection.
Classification of pneumonia
- by progression
- acute - sudden, lasting up to 3 months
- chronic - prolonged, over 3 months
- recurrent, or relapsing, in one area
- migratory, i.e. the inflammation moves to different sites
- by triggering cause
- infectious - bacterial, viral, fungal, parasitic
- non-infectious - after aspiration, i.e. inhalation, after inhalation of an aggressive substance, allergic
- by epidemiology
- communal - in common public places, easier treatment
- nosocomial - in a hospital setting, worse course of treatment
- by clinical manifestation
- typical - when symptoms indicate pneumonia, such as cough, fever, shortness of breath
- atypical - pneumonia may occur without fever or increased body temperature, or flu-like symptoms such as weakness, fatigue, joint and muscle pain
- by mechanism of origin
- primary - pneumonia only
- secondary - if it is a consequence of another disease
- by pathological picture
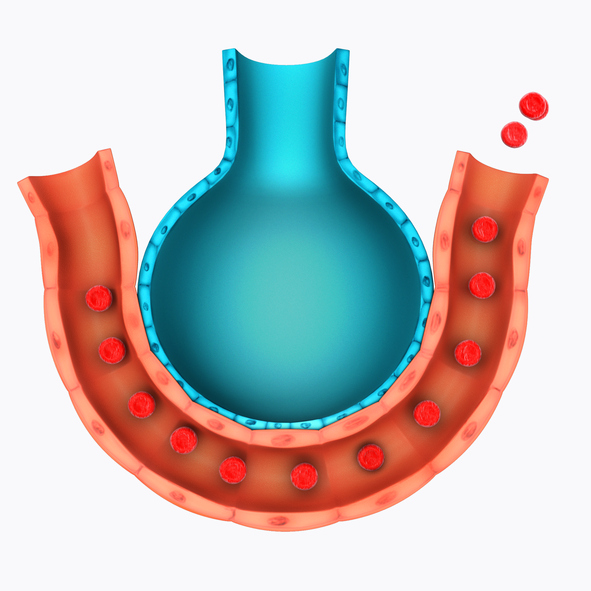
- alveolar - the alveoli of the lungs are affected
- interstitial - tissue between other structures such as the alveoli is affected
- by X-ray findings
- bronchial - if the entire lung wing is affected
- lobar - an inflamed lobe
- interstitial - affecting the interstitium
- bronchopneumonia - inflamed bronchi
Generally, lung inflammation damages the lung tissue. This causes coughing and breathing problems. Due to the often complicated course and long-term treatment of pneumonia, prevention is better, in the form of regular vaccination against respiratory diseases and influenza. And also in the form of a healthy lifestyle.
Causes
Pneumonia occurs when infection or non-infectious irritation causes disruption and damage to lung tissue. Inflammation develops on an infectious basis, whether bacterial, viral, mycotic or parasitic.
Non-infectiously, it can arise from irritation by gaseous or liquid chemicals that enter the respiratory tract. Similarly, it results from aspiration, i.e. inhalation of a foreign body into the lungs. Aspiration of gastric juice is the most risky.
The latter contains aggressive stomach acid or food particles. As a consequence, a complicated inflammation develops. The risk of aspiration of gastric contents occurs when the person is unconscious, severely drunk, or intoxicated with medicines or drugs.
When the person has been lying down for a long time, mucus accumulates in the lower airways and in the lungs. This promotes the multiplication of bacteria, which also provokes an inflammatory reaction. These inflammations are especially common in older non-self-sufficient and immobile people unable to position themselves regularly.
Young children, especially those under 1 year of age, are most at risk of pneumonia. And also people over 60 years of age, people with weakened immunity and people with associated chronic diseases. Pneumonia caused by a resistant infection can be a problem. In that case, it runs more complicated.
The most common forms are bacterial pneumonias. They are caused by bacteria such as Streptococcus pneumoniae, Streptococcus pyogenes or Streptococcus aureus. But also Haemophilus influenzae or Klebsiella pneumoniae, Chlamydia pneumoniae, Legionella pneumophila. These are representatives of the community type of bacterial pneumonia. And they occur commonly in the community, that is, in the public area, outside the hospital setting.
In the case of hospital-acquired infections, i.e. nosocomial infections, it is mainly Pseudomonas aeruginosa, Klebsiella pneumoniae or, for example, E. coli, RS virus, Herpes virus. In this type of pneumonia, there is a risk of more difficult treatment because of resistant strains.

Risk factors for the development of pneumonia:
- age - children and people over 60
- flu
- upper respiratory tract infection
- chronic diseases of the respiratory system - chronic bronchitis, chronic obstructive pulmonary disease (COPD)
- chronic diseases of the cardiovascular system
- stroke
- weakened immune system (after chemotherapy, immunosuppressants, AIDS)
- oncological diseases
- diabetes
- kidney disease - dialysis patients
- pregnancy
- smoking
- drug addiction
- alcoholism
- exposure to chemicals, e.g. working environments in construction or agriculture
Symptoms
Given the variety of causative agents and causes of pneumonia, it is to be expected that the symptoms will also be different. Bacterial pneumonia manifests itself slightly differently than viral or fungal pneumonia.
In general, it could be stated that pneumonia has symptoms such as:
- shortness of breath
- rapid breathing may be present
- cough (either dry or productive, depending on the causative agent)
- chest pain, aggravated by deep breathing, coughing
General manifestations have varying intensities:
- shivering, chills
- increase in body temperature to fever
- lack of appetite
- nausea
- fatigue
- weakness
- headache
- joint and muscle pain
Thus, the typical symptom for pneumonia is difficulty breathing and coughing. Either dry or later moist even with mucus, and usually among the characteristic clinical manifestations is also an elevated temperature, sometimes fever.
However, depending on the provoking cause, inflammation is also accompanied by other symptoms. In more severe forms of pneumonia, there is also shortness of breath and chest pain. The chest pain may be burning, stabbing or of a different nature.
Bacterial pneumonia
Bacterial inflammations present with fever, i.e. body temperature above 38°C, and general exhaustion. Bacterial inflammation is also characterised by a productive cough, i.e. coughing up mucus or pus. The mucus may be of varying consistency, colour (green, yellow, brownish, admixed with blood) and quantity.
Viral pneumonia
In viral inflammation, there is usually only an elevated temperature (body temperature up to 38°C). Viral inflammation progresses with less intensity of symptoms. However, the cough is irritating, dry, and choking. Of course, the person also experiences difficulty breathing. Chest pain is also present.
Bilateral pneumonia (Covid's pneumonia - pneumonia) with a typical image of milk glass on X-ray also has the disease COVID-19,which is caused by a new coronavirus, SARS-CoV-2.
Learn more: Coronavirus - COVID-19
Other types of pneumonia
With a mycotic origin of inflammation, the manifestations are similar to those of viral. Usually in infectious inflammation there are also general symptoms such as an increase in body temperature, joint, muscle and headache.
With non-infectious inflammation, nausea may also occur. Pneumonia may also be atypical, e.g. pneumonia without body temperature to fever, with a mild cough. The person also experiences shortness of breath due to exertion. If examined by auscultation, the finding may be negative. However, an x-ray will show extensive lung involvement.
Diagnostics
The diagnosis of pneumonia is based on the medical history and clinical picture. Changes in breathing are examined by auscultation (listening) using a phonendoscope. Imaging methods include chest X-ray or CT scan.
Chest and lung X-rays and CT scans reveal the extent of invasion and damage to lung tissue and identify the site of inflammation. Based on history taking and symptoms, possible risk factors for complications are identified.

Of course, as with any inflammation, there will be a blood test, mainly to check for blood count and to perform a thorough serological examination. Supplemental tests include sputum examination for microbiological examination and sensitivity to antibiotics.
Alternatively, bronchoscopy is performed in case of chronic problems and an unclear finding on X-ray. The reason for this is to exclude a tumor, that is, oncological disease. During bronchoscopy, it is sometimes necessary to take a sample directly from the airways.
Course
In most cases, pneumonia is acute, even as a complication of inflammation of the upper respiratory tract, complication due to influenza or other inflammation, regardless of whether it is of viral or bacterial origin.
Primary pneumonia with a bacterial causative agent is more severe and is characterised by a rise in body temperature above 38 °C, i.e. fever. The first few hours are characterised by a dry cough that later becomes a productive cough, i.e. with mucus.

The person is coughing up mucus of different consistency, colour (greenish, yellowish, brownish), purulent mucus or with an admixture of blood. The viral agent does not cause a high fever, but usually only an elevated body temperature, i.e. up to 38°C. The cough is dry, irritating and choking.
The person has difficulty breathing, which may be rapid and shallow accompanied by wheezing, whistling or squeaking sounds. Chest pain makes breathing and coughing deeper. Pain when breathing is suggestive of an inflammation of the pleurae, i.e. pleurisy.
So-called flu-like manifestations can also be present because of primary influenza, but also because of pneumonia. Thus, among the general symptoms, there is general weakness, malaise, fatigue, nausea, pain in the muscles, joints, and limbs. There is also headache, lack of appetite, a sensation of heaviness in the stomach, and vomiting.
General symptoms, without the typical course of pneumonia, may be present in atypical pneumonia. Of course, the important thing if more severe difficulties occur is immediate professional examination. In order to avoid complications.
Possible complications of pneumonia include:
- pleurisy, i.e. inflammation of the pleura
- empyema - a purulent deposit in the pleural space
- abscess - encapsulated inflammatory process
- gangrene - tissue necrosis
- septic shock
- in severe pneumonia, death
Inflammation is caused by the body's immune response to disruption and damage to lung tissue. Thus, it is very important to make a rapid diagnosis and start treatment as soon as possible. In the case of insufficient treatment, there is a risk of developing chronic lung disease, possibly resulting in a lung abscess and also a permanent reduction in lung function. In high-risk groups, almost a third of cases even end in death.
How it is treated: Pneumonia
Treatment of pneumonia - drugs, antibiotics, antivirals, inhalation?
Show morePneumonia
Pneumonia is treated by
Pneumonia is examined by
Other names
Interesting resources










