How to detect prostate cancer as early as possible and what are the treatment options?

It is the second most common cancer in Europe and worldwide and the most common cancer in men. About 95% of patients survive for 5 years and about half of them die.
Article content
Prostate cancer is an insidious disease but has a favourable prognosis if the tumour is localised and diagnosed early. The prognosis worsens in direct proportion to the growth of the tumour and the progression of the disease.
The disadvantage is that it can be asymptomatic or non-specific for a long time and then grow very rapidly.
When to increase attention and seek medical advice, read on.
When diagnosed early, it is a well treatable disease.
However, when diagnosed late, it leads to the death of the patient.
Noting the first symptoms and seeking early help is important.
Only then can treatment be successful.
What is prostate cancer?
Prostate (foreskin) cancer is a malignant disease. As it is an organ of the male reproductive tract, it affects only men.
It is one of the three most common diseases of this glandular organ in general. Its other two very common diseases are inflammatory processes and benign prostatic hyperplasia, also known as BPH.
In malignant prostate disease, there is an abnormal division of cells in the prostate that are not needed. They have no function and are not subject to apoptosis - natural cell death.
The mortality rate from prostate cancer decreases in direct proportion with patient awareness of the disease, early diagnosis and patient cooperation during treatment.
Men over 50 years of age should be especially alert.
Why is this so, you ask?
Anatomical and physiological conditions
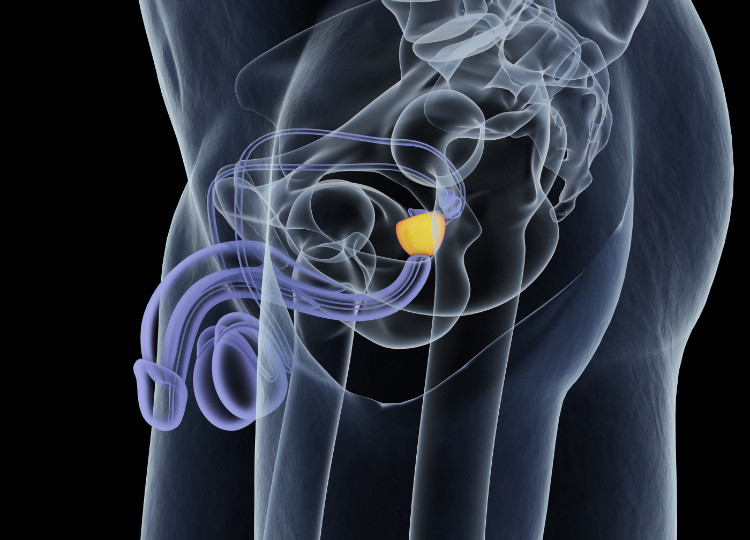
The prostate gland is part of the male reproductive system - more specifically the genital tract.
It is located on the musculature of the pelvic floor, behind the lower edge of the pubic symphysis, below the bladder (below its base). It could be said to surround the beginning of the male urethra, which passes through its center.
It is a rigid organ that resembles a chestnut in shape and size.
It has an oval shape measuring 4.5 cm x 2 cm x 3 cm.
It is partly made up of muscle, or smooth muscle cells, and connective tissue cells which surround its glands. The surface of the prostate is made up of a connective tissue sheath. This enters the prostate gland in some places and divides it into several lobes.
Anatomically, it has two parts and three lobes.
The basis prastatae or also the base of the prostate gland points upwards towards the bladder.
The apex of the prostate is located towards the pelvis. The middle lobe (lobus medius) is located in the middle and surrounds the urethra passing through the prostate. The right and left lobes (lobus dexter et sinister) are located on the side.
The function of the prostatic glands is to produce a thin secretion of cloudy milk-coloured secretion. This content, together with spermatozoa and mucous secretion formed in the epididymis, is discharged into the urethra.
These secretions along with the sperms form the ejaculate.
Factors in the development of prostate cancer
Age - as mentioned once before, prostate cancer occurs in middle-aged men.
Before the age of 50, only around 1% of cases have been reported. The cut-off age when it starts to occur is 50 years. However, most patients are still over the age of 60.
The basic prerequisite for the onset of this disease is increasing longevity, which results in prolonged exposure of the prostate to the hormone testosterone. Therefore, this disease is not present in childhood, nor in patients who have had their testicles removed for some reason.
Genetic factors - as with most cancers, prostate cancer is thought to have a genetic predisposition. Having the disease in the family increases the risk of the disease in the offspring up to threefold.
However, other factors that contribute to the development of the disease in a family are not excluded.
Chemical and physical influences - confirmed carcinogens are involved in the development of cancer itself and prostate cancer is not avoidable.
These include cigarette smoke, tobacco smoking, alcohol, aromatic hydrocarbons, UV radiation and other ionizing and radiant types of radiation.
In addition to the above, a large number of other confirmed and suspected carcinogens belong to this group.
Symptoms of prostate cancer
Prostate cancer may not show any symptoms in its early stages.
If preventive checkups are not on your list of responsibilities, it can very easily happen that your next visit to the doctor will be at a late (or terminal) stage because of coercion.
Pain
Pain is typical of cancer diagnoses. Pain occurs at the site affected by the cancer or in neighbouring organs by tumour overgrowth or in distant organs and parts of the body by metastasis.
Pain when the tumour is located in the prostate is usually intra-abdominal. The patient feels pressure or pain in the pelvic area, in the lower abdomen, sometimes when urinating. Nonspecifically, pain in the sacral spine may occur, which is often incorrectly confused with dorsalgia (neurological back pain).
Difficulty urinating
The growth of the tumour leads to non-specific symptoms related to its localisation on the pelvic floor muscles near the urinary tract below the lower bladder.
Therefore, the first warning signs include difficulty urinating.
- Frequent to urgent urination (polakisuria) with partial or even complete leakage of urine (incontinence) is typical. The same is true at night (nycturia), when the patient is often awakened by the need to urinate.
- The urine flow is weak. Sometimes it takes a while for the urine to start - so-called delayed urination.
- With further growth and pressure of the tumour, urination becomes difficult. For this reason, painful urination (dysuria) often occurs.
- Sometimes with the presence of blood in the urine, visible to the naked eye.
- When the tumour is already very large, it presses on the urethra so much that the patient has difficulty urinating. He feels like urinating, but only urinates a small amount of urine (oliguria) or eventually only drops to nothing at all (anuria).
- The accumulation of urine results in urinary retention with the need for a permanent catheter to be inserted through the urethra and into the bladder (urine drainage tube with collection bag).
Sexual difficulties
During intercourse, the muscles of the fallopian tube contract rhythmically and sperm are expelled from the epididymis. The smooth muscles of the seminal vesicles and prostate also contract.
If the prostate is affected by a cancerous process, we may observe difficulties with erection and changes in the ejaculate itself.
- Erectile dysfunction is the inability of the penis to swell or erect (fill the corpora lutea with blood) during intercourse and then to enlarge and lengthen, or to maintain this state. In this case, forget about erection enhancement products.
- If there is no problem with the erection, the sex organ will swell and ejaculation will occur. The ejaculate is normally physiologically made up of sperm and mucus-like secretion from the epididymis. In the case of a pathological process - and the same is true for prostate cancer - blood is usually present in the ejaculate. This is called haemospermia.
General discomfort
General symptoms include those that are typical and common to most cancers. The patient experiences increased fatigue, general weakness, malaise, dizziness.
Physical performance decreases compared to the previous condition. These symptoms are in the foreground.
The patient with prostate cancer is anaemic (anaemia), which only exacerbates the weakness of the body. In later stages, or when the tumour has metastasised, he or she cannot maintain balance due to weakness in the lower limbs, which become weak.
The terminal stage even leaves the patient bedridden, becoming immobile.
Sometimes there is a fever, a general weakening of the immune system with the subsequent development of secondary infections that make adequate treatment impossible.
Night sweats are present - either in combination with or without fever.
There is appetite, thirst, nausea or vomiting. Patients experience a gradual loss of weight, leading to a condition called cachexia - malnutrition, where the person's weight is very low, there are hardly any fat stores in the body and the bones are, as it were, covered with skin.
When should we increase our attention?
Due to the prevalence in the male sex and the high risk of developing it at the age of over 50 years, every man should have a urological examination of the prostate after this age. Subsequently, these examinations should be regular at least once a year.
You may not have known:
Men who are diagnosed with prostatic hyperplasia have the same risk of developing cancer as healthy men.
BHP has not yet been linked to a higher risk of cancer.
A higher incidence of the disease in African Americans is noted.
Probably due to the lower standard of living in these countries, mortality is higher and diagnosis tends to be made relatively late, which makes treatment options more difficult and significantly worsens prognosis.
When should increased attention be paid?
- Family history - If a direct blood relative in your family has had prostate cancer or another type of cancer, the risk of getting it can double or triple.
- Pain - The most common types of pain are abdominal and lower abdominal pain. Pelvic floor pain - non-specific, abdominal or low back pain, which is often incorrectly attributed to neuralgia (pain of a neurological nature) may also occur.
- Urinary problems - These are one of the most common indicators for prostate cancer. Of course, they are also present in many other diseases of the urinary tract, prostate or infections. Urinary problems vary from urgency to urinary leakage, frequent urination, later weak urination, weak urine stream to anuria (inability to urinate) with urinary retention (retention of urine in the bladder). Blood is usually present in the urine. In later stages, urination is painful.
- Sexual problems - Sometimes erection problems to erectile dysfunction occur. Blood may be present in the ejaculate.
- Other disorders - Cancers present with local discomforts depending on the site of origin, but also with general discomforts that are non-specific. They tend to be present in more than one disease. These include fatigue, malaise, excessive sleepiness, muscle weakness, apathy, decreased physical performance, lack of appetite, nausea, vomiting, excessive sweating, pallor, weight loss, and later cachexia, decreased immune system, frequent infections, febrile states, anemia, and others.
Treatment options
Treatment varies depending on the stage of the cancerous process at the time of diagnosis, the histological characteristics of the tumour tissue, the patient's general current condition, his/her age, life expectancy and associated diseases from which the patient suffered before the diagnosis of prostate cancer (diabetes, cardiovascular diseases, respiratory diseases, acute or chronic renal failure, blood diseases, etc.).
All of these factors and diseases can negatively affect the development of further treatment. Before starting the actual therapy, the patient must be thoroughly examined by his/her physician with regard to the above-mentioned factors. There are several options for prostate cancer therapy that can be combined with each other.

Surgical treatment
By surgical treatment we mean the surgical (operative) removal of the tumor. Sometimes it is with the necessity of removing the entire organ that is affected by the cancerous process.
If the tumour has spread to an adjacent organ, partial resection of the adjacent organ is also necessary. Sometimes castration is also recommended to improve the patient's overall prognosis.
- Surgical removal of the prostate is called prostatectomy. In some cases, if the tumour is caught at an early stage and is smaller in size, a subtotal prostatectomy is performed. This is the partial removal of the prostate along with the cancer. It is only recommended in the case of a circumscribed prostate tumour where the borders and margins are clearly visible.
- If the disease has been caught at later stages or its margins are not clearly visible, total prostatectomy - complete surgical removal of the entire prostate - is indicated. The prostate is removed in its entirety, including its capsule and seminal vesicles. In some worse cases, removal of lymph nodes from the pelvis is also necessary.
- In the case of total removal of the prostate, a subsequent connection of the bladder to the urethra, which was severed after the prostate was removed because it passed directly through the centre of the prostate, is necessary.
Hormonal treatment
The very essence of hormone therapy is the long-known fact that androgens (testosterone in men) are responsible for the growth of both normal and cancerous cells. Physiologically, they are responsible for the development of male sexual characteristics.
If the production of androgens is interrupted, the growth of cancerous cells is also stopped and they start to undergo apoptosis (natural cell death). Several ways are known to prevent their action. The different hormone therapy options can be combined.
- The source of the androgens is the testicles. This means that their total surgical removal prevents the action of androgens directly from the source. Their removal is called orchiectomy (castration) and is performed through the inguinal canal (groin). Since the testicles are the site of sperm production, this procedure results in complete sterility (infertility) of the patient.
- Another option is to reduce the effect (inhibition) of gonadotropins in the pituitary gland (hypothalamus) by means of luteinizing hormone (LHRH analogues). Gonadotropins are hormones produced by the pituitary gland. Their function is to induce and stimulate the activity of the gonads. The pituitary gland has a coordinating function and controls the endocrine glands. Among other things, it directly influences the formation of androgens in the testicles. It follows logically that inhibition of gonadotropic hormone also leads to inhibition of androgens. We speak of so-called medical castration.
- One of the options is to block the androgen receptors directly in the testicles. For this, we use steroidal or even non-steroidal anti-androgens. These interfere with testosterone production by directly blocking the androgen action in the receptors. They are thus directly involved in the cell death of the tumour tissue.
Radiotherapy
Radiotherapy uses ionising radiation (layman's term for irradiation) to treat prostate cancer. It is used for patients at a moderately advanced stage.
Prostate cancer cells are known to be more sensitive to the effects of ionising radiation than healthy cells in surrounding tissues. It is also used in patients who wish to avoid surgery. It is also used in combination with other prostate cancer treatment options.
- The radiation can be produced from a device called a linear accelerator. The point of entry into the patient is through the patient's skin. This therapy is also called external beam radiation therapy (EXRT). The treatment lasts approximately two months. The patient is irradiated 5 times a week. These time periods are called fractions. The disadvantages of this method are that the healthy tissues are also irradiated and the patient becomes weaker overall. Ionizing radiation and its effect on healthy cells and the patient in general has its negatives. After radiation, the patient tends to be generally weak, malaise, and suffers from lack of appetite or vomiting.
- Radiotherapy, in which a source of ionising radiation is placed directly into the prostate near the tumour cells and radiation is given locally at close range, is called brachytherapy. This therapy is carried out while being monitored by ultrasound. The advantage of this method of radiation is that higher doses of radiation can be used, which ultimately means a more invasive therapy against the tumour with a higher chance of stopping the division of the tumour cells. The unwanted radiation exposure to healthy tissues in the vicinity is also reduced.










