- Internal medicine: Souček Miroslav, a kolektiv
- Gastroenterology and Hepatology - textbook: Aleš Žák
- medlicker.com - Indigestion (dyspepsia): everything you need to know
- npz.sk - Digestive problems often start in the head
- clevelandclinic.org - Functional Dyspepsia
- pubmed.ncbi.nlm.nih.gov - Dyspepsia: organic versus functional
- nhs.uk - Indigestion
- mayoclinic.org - Indigestion
- webmd.com - Indigestion
What is dyspepsia: What are the symptoms and course of the digestive disorder?

Dyspepsia refers to a digestive disorder. It can be part of a variety of gastrointestinal diseases. Examples of problems include abdominal discomfort, abdominal pain and gas.
Most common symptoms
- Malaise
- Chest pain
- Stomach pain after a meal
- Abdominal Pain
- Anal pain
- Belly button pain
- Painful bowel movements
- Lower Abdominal Pain
- Nausea
- Constipation
- Thinning
- Diarrhoea
- Black stool
- Rash
- Flatulence - bloating
- Bloating - flatulence
- Indigestion
- Heartburn
- Swallowing disorders
- Buds
- Cold extremities
- Head spinning
- Fatigue
- Anxiety
- Vomiting after eating and nausea
- Vomiting
- Reddened skin
- Increased appetite
Characteristics
The word dyspepsia comes from the Greek dys (disorder), pepsis (digestion).
It is a set of various digestive disorders, a manifestation of gastrointestinal diseases, but also an accompanying phenomenon of diseases of other body systems.
Dyspepsia manifests itself many times with variable symptoms. Often the trouble recurs.
The human digestive system in brief
Digestion is the part of metabolism by which the body obtains energy.
Digestion consists of:
- taking in food
- processing food
- absorption of nutrients
- excretion of undigested residues
The digestive tract consists of:
- the oral cavity
- pharynx
- oesophagus
- stomach
- small intestine
- large intestine
- rectum
- anal opening
The glands of the digestive system are:
- liver
- pancreas
- salivary glands
Epidemiology - what is the incidence?
Approximately ¼ of the world's population suffers from dyspepsia. Of these, only ¼ seek medical attention.
After visiting a doctor with a digestive disorder, only about 10% of patients are referred for endoscopic examination immediately and 20-30% of people within 1 year.
Indigestion is more common in young people under the age of 40. It is more likely to affect women and people exposed to stressful situations.
Dyspepsia is divided into...
- Primary (organic), which is caused by an organic disease e.g. inflammation, ulcer
- Secondary, which is caused by extra-intestinal disease, e.g. cardiovascular, metabolic, endocrine, or the effects of drugs and toxins
- Functional - functional dyspeptic syndrome is defined as those not associated with previous diseases
- Unresolved types of dyspepsia based on psychofunctional disorders. These include inappetence and constipation in depression, vomiting in aversion, abdominal pain in anxiety, urge to defecate in stage fright, diarrhea in fear
Classification of dyspepsia by localisation
1. Upper dyspepsia - problematic digestion in the stomach area.
2. Lower dyspepsia - indigestion affecting the intestines.
Functional dyspepsia of the upper type
Upper gastric dyspepsia (functional gastropathy) is manifested by dyspeptic symptoms due to a disturbance in the function of the stomach. The most common cause is a disturbance in digestive movements. It is one of the most common gastric diseases.
Dyspepsia of the upper digestive tract often has a chronic or recurrent course.
Symptoms may be varied. However, pain and abdominal discomfort in the form of an unpleasant sensation in the abdomen, which may not be accompanied by pain, are dominant. It may be in the form of pressure, premature satiety after eating, with inappetence, nausea (feeling of vomiting).
Symptoms in all patients are not the same. According to the types of problems are distinguished into different functional dyspepsia.
Division of dyspepsia by type
In reflux type, also called as GERD (gastroesophageal reflux disease), gastric juice gets back into the esophagus and causes heartburn.
The dysmotility type results from limited or impaired gastrointestinal motility, as may be the case with a flabby stomach.
In ulcer dyspepsia (irritable stomach), there is increased gastrointestinal motility and secretion with painful pressure in the epigastrium (the area below the sword-shaped process of the sternum, the part between the chest and the midline of the abdomen). It resembles ulcer problems, such as pain at fasting with relief after eating.
Idiopathic dyspepsia arises from unknown causes, separate and independent of any other disease.
Aerophagia is increased swallowing of air that accumulates in the stomach and causes digestive problems.
Functional dyspepsia of the lower type
Diseases of the lower digestive tract include intestinal dyspepsia, which is very unpleasant and impairs quality of life.
It is more common in women than in men.
Functional dyspeptic syndrome is a manifestation of various factors, such as the influence of the external environment, stress, psychosocial influences, a person's personality, abnormal motility, visceral sensitivity (sensitivity of internal organs and skin), food allergies and others.
Causes
The cause of dyspepsia can be (table)
| Dyspepsia organic | caused by tumour, ulcer, gastroesophageal reflux disease |
| Dyspepsia secondary | secondary, in general disease or disease of other organs, pancreatic disorder, biliary disorder |
| Dyspepsia functional | as a separate disease |
Read also articles that may be related to indigestion:
- Pancreatitis: acute, chronic or necrotizing pancreatitis?
- Cholecystitis.
- Gastritis.
- What is Celiac Disease: briefly about the cause, symptoms and treatment?
What causes functional dyspepsia?
- Impaired gastric emptying. In some people, the function of the stomach is disturbed, leading to slower gastric emptying and subsequent food accumulation. Prolonged lying of food in the stomach causes gas accumulation and bacterial growth.
- Food allergies can cause an inflammatory reaction in the intestine.
- Helicobacter pylori, which is one of the common gastric infections, can cause chronic inflammation of the stomach.
- Psychological factors, especially in people with a sensitive nervous system. Stress and tension can physically affect digestion.
Risk factors
- Age over 65 years
- combination of NSAIDs (non-steroidal anti-inflammatory drugs) with ASA (acetylsalicylic acid), anticoagulants, antidepressants, corticosteroids
- smoking
- alcohol
- ulcer disease
- anxiety, depression
- Helicobacter pylori
Symptoms
Usually the symptoms increase during the day and usually subside at night.
The most common symptoms of dyspepsia are:
- Pain in various places in the abdomen
- Pressure pain in the abdominal area
- Feeling of fullness
- Feeling of inadequate digestion, food remains in the stomach for a long time
- Urge to vomit, feeling of stomach on water
- Heartburn - pyrosis
- Belching and passage of gas from the stomach through the oral cavity - ructus, eructation
- Flatulence - flatulence
- Increased passage of gases - flatulence
- Feeling of incomplete emptying
- Constipation - obstipation
- Diarrhoea - diarrhoea
- Vomiting - emesis
- Change in stool frequency
- Frequent and compulsive defecation
- Irregular stools with variable consistency
- Chest pain
Frequent symptoms of upper dyspeptic syndrome:
- Unappetite
- Feeling of fullness
- Nausea - urge to vomit
- Vomiting
- Anorexia
- Salivation - salivation
- Pain in the epigastrium when swallowing
Common symptoms of lower dyspeptic syndrome:
- Diarrhea
- Constipation
- Bloating
- Flatulence
- Painful urge to pass stool
Classification of functional dyspepsia by symptoms
Functional esophageal disorders
- Functional pyrosis (heartburn) is a burning sensation behind the rib cage, pain without the presence of esophageal reflux disease, without histological signs of gastric motility disorders
- Chest pain probably of oesophageal origin, pain and discomfort in the midline of the chest that is not burning in nature
- Functional dysphagia(difficult swallowing) is the sensation of abnormal passage of food through the oesophagus
- Globus is the sensation of a foreign body in the throat that is not painful. It occurs between meals
Functional disorders of the gastroduodenum - stomach and duodenum
- Functional dyspepsia is an unpleasant feeling of food persisting in the stomach, an unpleasant feeling of an early overcrowded stomach independent of the amount of food, pain in the epigastrium and burning in the epigastrium
- Disorders associated with eructations (belching): aerophagia is the morbid swallowing of air that accumulates in the stomach, but also non-specific excessive belching without evidence of air swallowing
- Nausea and vomiting
- Chronic idiopathic nausea - straining to vomit, not always associated with vomiting and occurring several times a week
- Functional vomiting - vomiting one or more times per week, without the presence of an eating disorder
- Cyclic vomiting syndrome - in the acute onset, recurrent episodes of vomiting lasting less than a week and occurring more than once a year. In between periods, the person is free of nausea and vomiting
- Adult rumination syndrome (easy regurgitation), return of recently ingested food from the stomach to the mouth, without vomiting. Episodes last 1-2 hours and are without previous nausea. Often this symptom is confused with anorexia, bulimia, as weight loss often occurs
A simpler classification is to divide it into two forms
Irritable stomach - hypersthenic dyspepsia
An irritable stomach is characterized by an increased reaction, in the form of cramps, pain, heartburn, acid regurgitation (re-entry of food into the oral cavity), vomiting.
An irritable stomach is often accompanied by intolerance to alcohol, coffee and irritating foods.
Pain in the epigastrium occurs after eating with relief after digestion. Fasting pain may occur, which disappears after eating.
Appetite is usually good.
This type is also referred to as pseudoulcerosis syndrome.
Vomiting may be irritative with a small amount of vomit or vomiting of a larger amount with stomach acid. There is relief after vomiting.
Weak stomach - hyposthenic dyspepsia
A weak stomach is manifested by decreased appetite, premature satiety, a feeling of pressure and fullness after eating, nausea and a feeling of slow digestion.
The appetite is weaker.
This type belongs to the dysmotility types.
The whole function of the digestive tract is reduced.
Neurodigestive asthenia is characterized by gastrointestinal disturbance and reduced performance, prolonged and variable problems, intolerance to certain foods.
The overall problems manifest themselves as a general illness.
They are manifestations of nervous system disorders such as:
- insomnia
- nervousness
- fatigue
- Anxiety - a state of distress in many psychoneuroses
- depression
- hypochondria - fear and fabrication of illness
- obsessions - intrusive thoughts
- obsession
- tics
- neurotic speech
- concentration disorders
- sweating
- acrohyperhidrosis - increased sweating on the hands and feet
- cold acre - extremities, limbs, nose, chin
- dermographism - skin reactions such as paleness or redness
- erythema pudendi
- pulse instability - rapid changes in heart rate
- tachycardia - rapid heart rate
- palpitations - heart palpitations
Manifestations fluctuate throughout the year with irregular intervals.
Intestinal dyspeptic syndrome
It is characterized by
- discomfort throughout the abdomen, sometimes only around the navel
- feeling of pressure and fullness
- cramping and spilling of intestinal contents
- flatulence
- increased bowel sounds, increased bowel movements manifested by impaired motility (bowel movements)
- disorders of faecal excretion
- impaired secretion of mucus in the stool
- disturbances of intestinal chemistry affected by the intestinal microflora, with a predominance of fermentative and putrefactive processes
Distribution
Irritable bowel - abdominal pain, irregular stools, feeling of urge to defecate, feeling of inadequate defecation + also referred to as irritable bowel syndrome.
Functional diarrhoea - painless thin stools, no other symptoms.
Spastic constipation is accompanied by unpleasant abdominal pain of varying intensity. The urge to defecate is absent and the stool passes after several days. The stool is bay or ribbon-shaped.
Yeasty, putrefactive dyspepsia is associated with intestinal hypermobility (excessive bowel movement) associated with yeast or putrefactive organisms.
Right iliac fossa syndrome. Typically characterized by pain in the right iliac fossa accompanied by flatulence, excessive passage of gas through the rectum, and irregular diarrheal stools.
Diagnostics
Diagnosis focuses mainly on symptoms and the exclusion of a primary or secondary cause.
It focuses on the characteristic manifestations and the time course in relation to psychological and physical stress.
Current treatment and drug interactions that could cause digestive problems, the degree of risk of malignancy, information on previous illnesses are ascertained.
The patient's age, unexplained weight loss, changes in bowel movements, slight increase in temperature, vague malabsorption (disorders of digestion and nutrient absorption) are taken into account.
Objective examination
The patient is observed for cold and sweaty acral areas, trembling of the fingers and eyelids, skin redness, itchy eczema on the skin, red dermographism (skin reaction to mechanical irritation, circumscribed redness after scratching), neurotic behaviour, pulse lability (rapid changes in heart rate), tendon hyperreflexia, which could be related to other diseases.
Physical examination
- Per rectum examination
- Examination of the abdomen by palpation, with tenderness in the epigastrium in the midline
Laboratory examination:
- Examination of blood, urine, and stool will tell a lot about the person's health and rule out other diseases (biochemical blood tests, sedimentation rate, blood count, liver function tests, blood glucose and amylase levels, CRP stool examination for occult bleeding, for parasites, blood and urine amylase tests, or food intolerance testing)
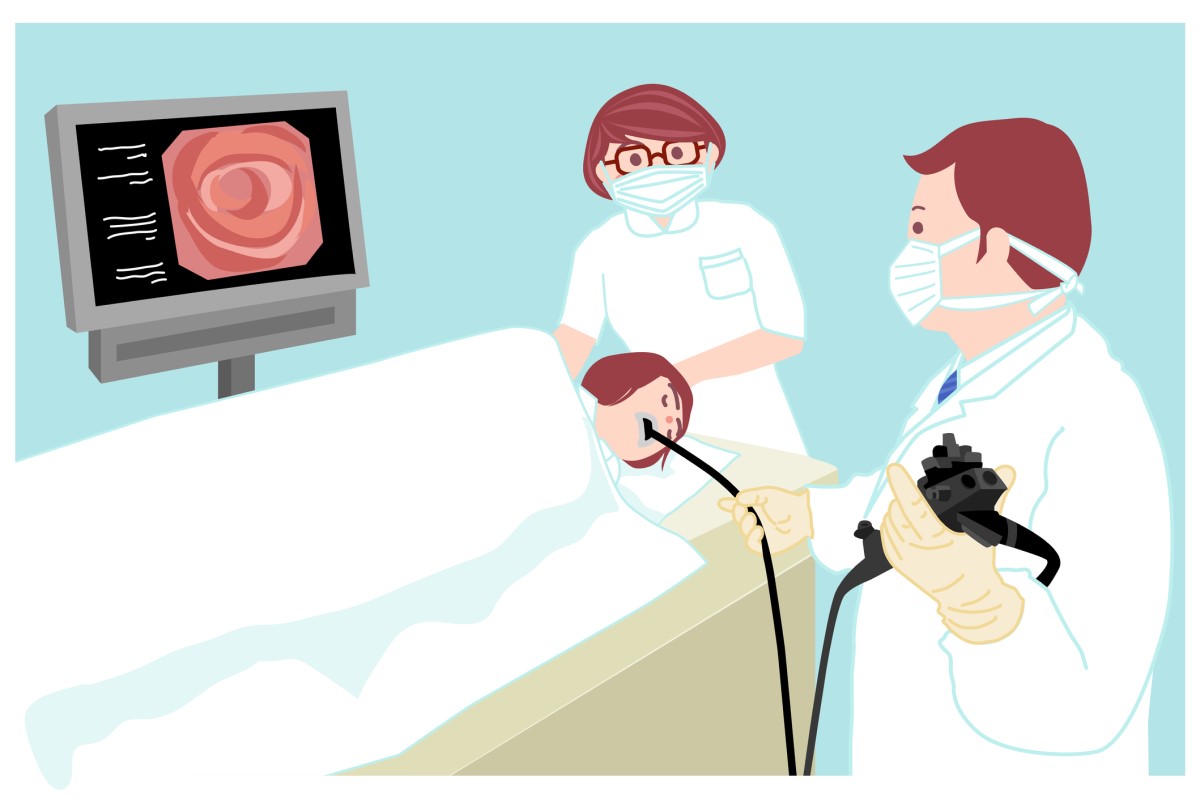
Endoscopic examination
Endoscopy is the safest method to rule out the disease and should be done for any type of dyspepsia. It is a diagnostic imaging method to optically examine the body cavities using an endoscope device.
- Gastroscopy - examination of the stomach and duodenum
- Colonoscopy - examination of the small and large intestine
- Fibroscopy - examination of the small intestine
For women, a gynaecological examination is also recommended.
Other imaging methods are sonography, X-ray of the stomach, CT scan and MRI scan.
A therapeutic or diagnostic-therapeutic test is common, where drugs are given for two weeks to relieve symptoms, such as proton pump inhibitors, prokinetics, spasmolytics, eubiotics.
Course
Dyspepsia also has variable periods. A person feels well, has no problems, and suddenly problems arise in various forms. These may recur during the year, with varying durations.
Dyspepsia can be divided into
The acute form, which lasts 7-10 days and is usually of infectious origin or due to the ingestion of spoiled food.
The chronic form, the duration of which is 12 weeks or more in the last year, even intermittently.
Dyspepsia and pregnancy
Pregnancy is often associated with digestive difficulties that appear from the beginning of pregnancy, and especially from the 27th week of pregnancy.
Dyspepsia occurs in many women during pregnancy, most commonly in the form of heartburn caused by reflux of stomach acid from the stomach into the oesophagus, nausea, indigestion, bloating and constipation.
They can be caused by the baby's growth and the enlarging uterus pressing on the stomach, but also by hormonal changes. Increased levels of certain hormones during pregnancy cause the muscles and musculature of the esophageal sphincter to relax.
Dyspepsia does not threaten the woman during pregnancy or the developing baby. It is one of the unpleasant difficulties that accompany pregnancy.
An appropriate diet and a healthy lifestyle help to alleviate the symptoms.
If dyspeptic symptoms persist and are uncomfortable, consult your gynaecologist or pharmacist about the appropriate form of medicine to relieve the symptoms.
It should be borne in mind that not all medicines for digestive problems are appropriate to take during pregnancy.
What diet to avoid for indigestion?
Inappropriate foods that increase acidity in the stomach are tomatoes, chocolate, fatty and spicy foods, all fruit juices, hot drinks, coffee, alcoholic beverages.
Read also the article:
Reflux: treatment and diet for heartburn, which foods are unsuitable?
How it is treated: Dyspepsia
What is the treatment for dyspepsia? Medication, regimen and diet + Alternative
Show moreDyspepsia is treated by
Other names
Interesting resources










