- Vela, M. et al., Reflux Disease of the Esophagus - GERD, Grada, Prague 2015
- solen.sk - GASTROEZOFÁGOVÁ REFLUXNÍ DOROBA, Ladislav Kužela, Marian Oltman
- webmd.com - GERD
- emedicine.medscape.com - Gastroesophageal Reflux Disease Treatment & Management
- healthline.com - Everything You Need to Know About Acid Reflux and GERD
- webmd.com - Complications of Heartburn and GERD
- ncbi.nlm.nih.gov - Diagnosis and treatment of gastroesophageal reflux disease
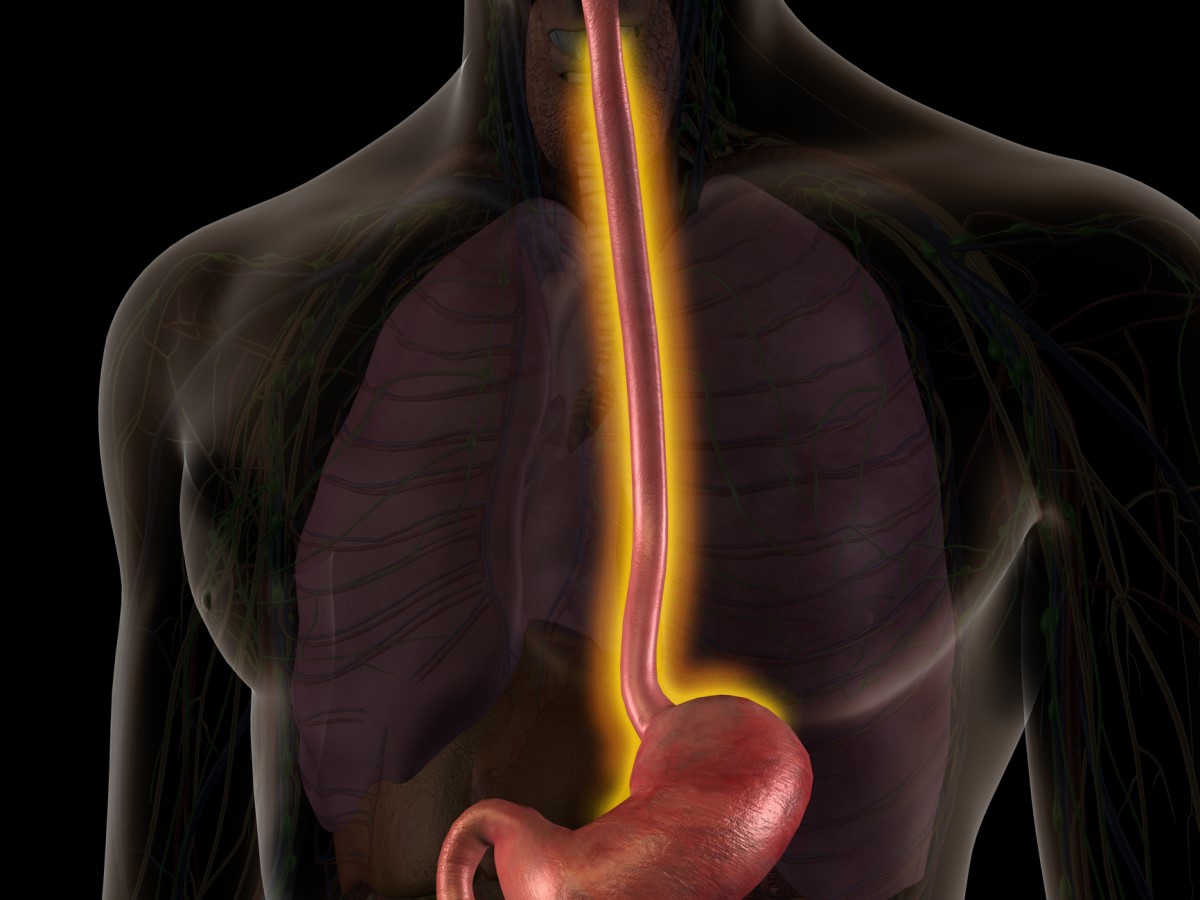
GERD: Gastroesophageal reflux disease. Classic heartburn and gastroesophageal reflux disease

Gastroesophageal reflux is a disease manifested mainly by heartburn. It seriously reduces the quality of life of the patient.
Most common symptoms
- Chest pain
- Stomach pain after a meal
- Abdominal Pain
- Sore Throat
- Pain when swallowing
- Hoarseness
- Spirituality
- Nausea
- Black stool
- Heartburn
- Dry cough
- Vomiting
- Vomiting blood
Characteristics
Gastroesophageal reflux is a normal physiological phenomenon that most people experience occasionally, especially after eating.
Gastroesophageal reflux disease (GERD) occurs when the amount of gastric juice that enters the esophagus through the reflux tract exceeds the normal limit. This causes symptoms with or without associated damage to the lining of the esophagus (i.e. esophagitis - inflammation of the esophagus).
GERD = GastroEsophageal Reflux Disease
Causes
Schematically, the esophagus, lower esophageal sphincter (LES) and stomach can be imagined as a simple water circuit.
The oesophagus acts as an antegrade pump (pump driving food towards the stomach), the lower oesophageal sphincter as a valve and the stomach as a reservoir.
Abnormalities that contribute to GERD can originate from any component of the system. The cause may be poor esophageal motility, a dysfunctional lower esophageal sphincter, or delayed gastric emptying.
Transient relaxations of the lower esophageal sphincter represent the most significant pathophysiological factor.
From a medical or surgical point of view, it is extremely important to identify which of these components is defective so that effective therapy can be applied.
When discussing the mechanisms of GERD, the issue of hiatal hernia or hernia (protrusion of part of the stomach above the diaphragm toward the esophagus) should be mentioned.
A hiatal hernia is often encountered in patients with reflux disease. However, it has been shown that not all patients with hiatal hernia have symptomatic reflux.
Risk factors for the development of esophageal reflux disease include:
- hiatal hernia - Often hiatal hernia is accompanied by reflux.
- Overweight or obesity - Several studies have shown that GERD occurs at a high rate in morbidly obese patients and that high body mass index (BMI) is a risk factor for the development of this condition. The hypothesis that obesity increases esophageal acid exposure is supported by the documented relationship between increased BMI and increased prevalence of GERD. The mechanism by which high BMI increases esophageal acid exposure is not fully understood. Increased gastric pressure, lower esophageal sphincter (LES) incompetence, and increased frequency of transient lower esophageal sphincter relaxations may play a role in the pathophysiology of GERD in patients who are morbidly obese
- Pregnancy - Most pregnant women experience symptoms of gastroesophageal reflux disease (GERD) during pregnancy, especially heartburn. These symptoms can occur at any time during pregnancy and often worsen during pregnancy. Hormones actually cause the digestive system to slow down. The muscles that move food up the esophagus also move more slowly during pregnancy. As the uterus grows, it pushes on the stomach. This can sometimes push stomach acid into the esophagus. GERD in pregnancy can rarely cause complications such as esophagitis. Most often, symptoms subside after the baby is born. Treatment for pregnant women is no different from that of the general population
- Delayed gastric emptying (gastroparesis)
- Connective tissue diseases such as rheumatoid arthritis, scleroderma or lupus
Diet and lifestyle choices can worsen acid reflux if you already have it:
- Smoking - Smoking causes increased relaxation of the lower esophageal sphincter, decreased salivation, increased acid secretion in the stomach, and destruction of the protective layer of the esophagus. All of these factors contribute to the development of GERD in smokers. Research has also shown a link between smoking and some of the worst complications of GERD, including Barrett's esophagus and throat cancer.
- Certain foods and drinks, including chocolate and fatty or fried foods, coffee and alcohol
- Large portions of food - They increase pressure in the stomach
- Eating food just before bedtime
- Certain medications - calcium channel blockers, nitrates, beta blockers, hormones - progesterone, aspirin

Symptoms
The most common symptom of GERD is heartburn - pyrosis (acid indigestion). It is usually described as a burning pain in the chest that starts behind the breastbone and moves upwards towards the neck and throat.
Many people say they feel that food is going back into their mouths, leaving a sour or bitter taste.

Other symptoms of GERD include:
- Nausea (feeling like vomiting)
- vomiting
- difficulty swallowing
GERD can also have so-called extra-intestinal symptomatology, which includes pulmonary manifestations (cough, asthma, aspiration pneumonia - pneumonia from inhaled food). It is often one of the causes of extra-thoracic chest pain, halitosis (bad breath), tooth enamel wear, laryngitis (inflammation of the larynx). It can also cause 'globus' (feeling of a foreign body in the throat) or sleep problems.
GERD can be classified as non-erosive reflux disease (NERD) or erosive reflux disease (ERD). This is differentiated based on the presence or absence of damage to the lining of the esophagus observed during endoscopy (gastroscopy).
3x complications of esophageal reflux disease
- Damage to the oesophagus
- Increased risk of oesophageal cancer
- Dental caries
1. Esophageal damage
If acid from the stomach enters the esophagus and damages the esophageal lining there, it can cause:
- Esophagitis (inflammation of the esophagus) - Stomach acid irritates the lining of the esophagus and causes it to swell. This inflammation is called esophagitis. It can lead to painful swallowing
- Esophageal ulcers - GERD is the leading cause of esophageal ulcers. Symptoms include painful swallowing, nausea and chest pain
- Esophageal strictures (narrowing of the esophagus) - Over time, damage caused by stomach acid can scar the esophageal epithelium. When there is a lot of this scar tissue, the esophagus narrows. These narrow spots, called strictures, make it difficult to swallow food and drink. This can lead to weight loss and dehydration. Strictures are treated with a procedure that gently dilates the esophagus (called balloon dilation)
- Barrett's oesophagus - About 5% to 10% of people with GERD develop this condition. Stomach acid causes precancerous changes in cells (precancer - a condition that precedes the development of a malignant tumour).
The good news is that only 1% of people with Barrett's esophagus get esophageal cancer. With early diagnosis, removal of the abnormal cells in the esophagus is possible.
Barrett's esophagus does not cause any more severe symptoms than GERD itself. Therefore, a patient with GERD should be examined endoscopically (gastroscopy).
2. Increased risk of oesophageal cancer
A diagnosis of GERD slightly increases the risk of developing this type of cancer.
Symptoms of this type of cancer, such as difficulty swallowing and chest pain, do not appear until later in the disease. This is when it is more difficult to treat the condition.
3. Dental caries
Heartburn can also take a toll on your smile. Stomach acid can damage the enamel, the hard outer layer of your teeth, and this can weaken your teeth and lead to tooth decay.
Diagnostics
The diagnosis of GERD is made by symptoms, objective testing including endoscopy, outpatient monitoring of reflux and response to antisecretory therapy.
Symptoms of heartburn and regurgitation (the return of food from the stomach sometimes to the mouth) are the most reliable for making a presumptive diagnosis.
Esophagogastroduodenoscopy (EGD, gastroscopy)
Endoscopy of the upper gastrointestinal tract demonstrates the anatomy and identifies the possible presence and severity of complications of reflux disease (esophagitis, Barrett's esophagus, strictures).
Using the patient's history and pathological analysis of biopsy specimens obtained during endoscopy, a diagnosis of GERD can be made.
Esophagogastroduodenoscopy also excludes the presence of other diseases (e.g. peptic ulcer) that may present similarly to GERD.
Although oesophagogastroduodenoscopy is often performed for the diagnosis of GERD, it is not the most cost-effective diagnostic method. In fact, oesophagitis is present in only 50% of patients with GERD.
Oesophageal manometry
Oesophageal manometry records the function of the lower oesophageal sphincter and oesophagus (peristalsis). Oesophageal manometry is essential for correct placement of the probe for 24-hour pH monitoring.
Indications for esophageal manometry and prolonged pH monitoring include the following:
- Persistence of symptoms while taking adequate antisecretory therapy, such as PPI therapy.
- recurrence of symptoms after discontinuation of acid-reducing drugs
- investigation of atypical symptoms, such as chest pain or asthma, in patients without oesophagitis
- confirmation of the diagnosis in preparation for antireflux surgery
24-hour outpatient pH monitoring
Ambulatory 24-hour pH monitoring is the standard criterion for the diagnosis of GERD with a sensitivity of 96% and specificity of 95%. It quantifies gastroesophageal reflux and allows correlation between reflux symptoms and reflux episodes.
Patients with endoscopically confirmed esophagitis do not require pH monitoring to establish a diagnosis of GERD.
Imaging in gastroesophageal reflux disease
Simple radiographic findings are not useful in the evaluation of patients suspected of having a diagnosis of GERD, but are useful in the evaluation of lung status and basic anatomy.
Chest images may demonstrate a large hiatal hernia, but small hernias can be easily missed. Studies with contrast in the upper gastrointestinal tract are the initial radiologic procedure of choice when investigating a patient who is suggested to have GERD.
Inflammatory and neoplastic esophageal diseases are better detected with double-contrast techniques. Conversely, single-contrast techniques are more sensitive for structural defects such as hiatal hernias and strictures or esophageal rings.
Although delayed gastric emptying is present in up to 60% of patients with GERD, this emptying defect is usually a secondary factor in the pathogenesis of the disease in most patients (except in patients with advanced diabetes mellitus or connective tissue disorders).
Patients with delayed gastric emptying usually experience bloating and fullness after eating, among other symptoms.
Gastric emptying investigations may be useful in the evaluation of patients in whom delayed gastric emptying is thought to contribute to the symptoms of GERD.
Nuclear methods
Gastroesophageal reflux scintigraphy can be performed with acidic orange juice labeled with technetium-99.
However, gastroesophageal reflux scintigraphy plays a minor role in the adult patient because of the limited sensitivity and availability of other methods.
Gastroesophageal reflux scintigraphy is much more commonly used in infants and children because of the non-invasive nature of the study and the relatively low radiation dose. In infants and children, it is often performed with labelled milk.
Intraluminal oesophageal electrical impedance
Intraluminal esophageal electrical impedance is a newer investigative method. It is useful for detecting both acid reflux and non-acid reflux by measuring backflow in the esophagus.
How it is treated: Gastroesophageal reflux disease - GERD, reflux, heartburn
Treating GERD: Can medication, lifestyle changes or surgery help?
Show moreGastroesophageal reflux disease is treated by
Other names
Interesting resources










