- emedicine.medscape.com - Acute Pancreatitis. Jeffrey C F Tang, MD
- webmd.com - Pancreatitis. Neha Pathak, MD
- uptodate.com - Clinical manifestations and diagnosis of acute pancreatitis. Santhi Swaroop Vege, MD
- ncbi.nlm.nih.gov - Acute Pancreatitis. Jonathan Gapp; Subhash Chandra
- researchgate.net - (PDF) Risk factors for increased intra-abdominal pressure in severe acute pancreatitis
Acute pancreatitis: can be mild or fatal. Symptoms of pancreatitis

Acute pancreatitis (inflammation of the pancreas) is usually characterised by high intensity pain. What other problems does this serious condition bring with it? Why does it arise?
Most common symptoms
- Stomach pain after a meal
- Abdominal Pain
- Belly button pain
- Back Pain
- Fever
- Increased body temperature
- Nausea
- Diarrhoea
- The Island
- Vomiting
- Yellow whites of the eyes
- Yellowish skin
- Accelerated heart rate
Characteristics
Acute pancreatitis is an inflammation of the pancreas, which is usually very painful and can be fatal in severe cases.
Acute pancreatitis is the leading cause of gastrointestinal-related hospital admissions. Its frequency is steadily increasing worldwide.
The severity of the disease varies widely, from mild disease requiring conservative treatment to severe and complicated disease with high morbidity and mortality.
Pancreas
The pancreas is an organ located in the abdomen. It plays a vital role in digesting the food we eat.
The pancreas has two main parts. The exocrine part is made up of acinar cells that produce digestive enzymes to aid in digestion (mainly amylase, lipase, trypsin) and makes up 80% of the pancreas.
The endocrine part regulates blood sugar levels with the hormones insulin and glucagon and makes up 20% of the pancreas.
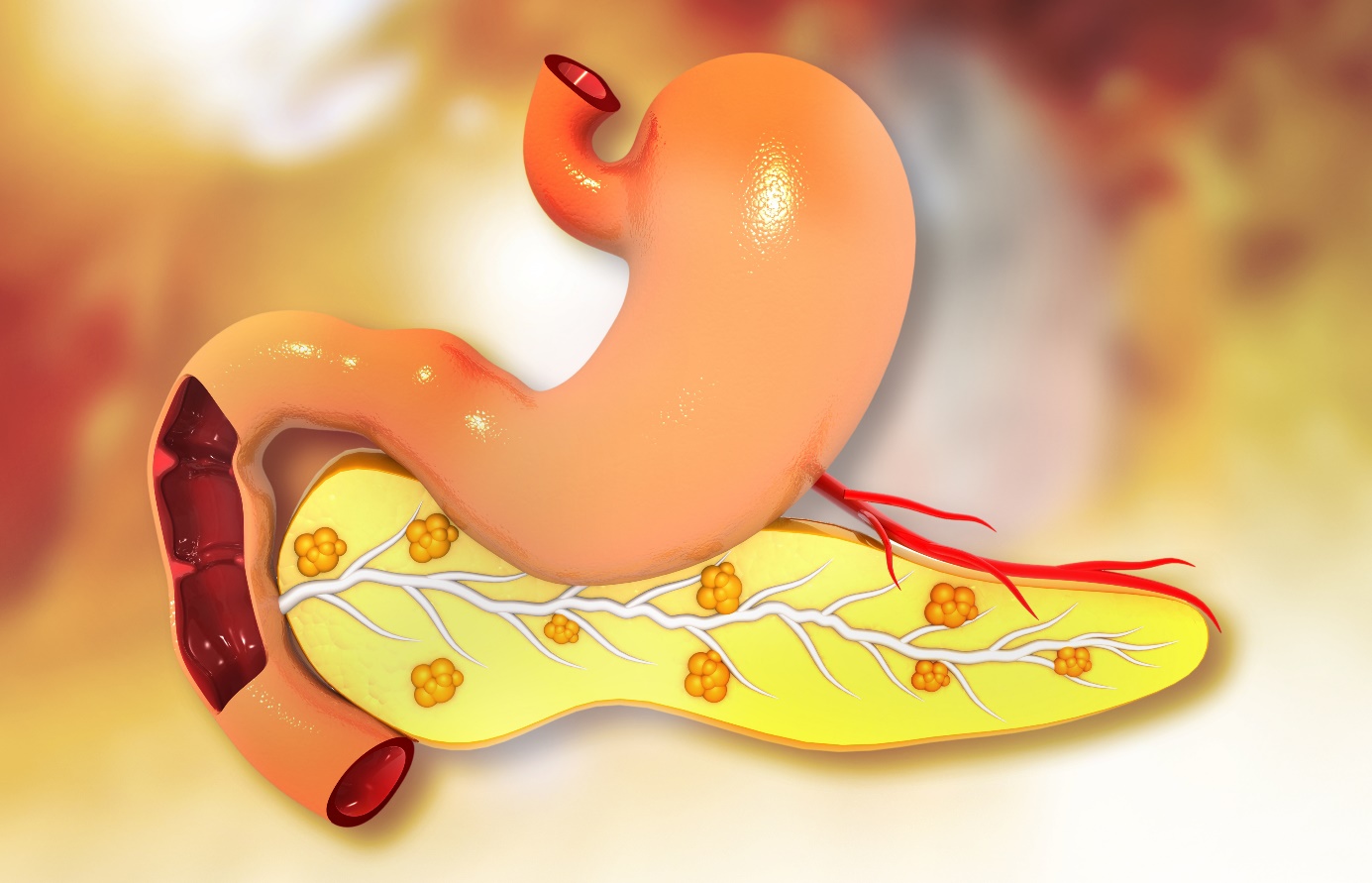
Location of the pancreas
The pancreas is located behind the stomach in the upper left part of the abdomen. It is surrounded by other organs including the small intestine, liver and spleen.
It is a spongy gland, about 16-22 cm long and shaped like a flat pear.
The broad part, called the head of the pancreas, is located towards the middle of the abdomen.
The head of the pancreas is located where the stomach meets the first part of the small intestine, the duodenum. Here the stomach empties partially digested food into the intestine and the pancreas releases digestive enzymes into these contents.
The central part of the pancreas is called the body. Its thin end is called the tail and extends to the left side of the abdomen.
How does pancreatitis occur?
Acute pancreatitis can arise when factors involved in maintaining cellular balance are disturbed. The initiating event can be anything that damages the acinar cell and disrupts enzyme secretion.
This can include alcohol use, gallstones and certain drugs.
Once cellular damage is triggered, the damaging effects on the pancreas begin. The cellular damage causes an inflammatory reaction in the pancreatic tissue. The pancreas swells and its tissue is destroyed.
When the mediators are secreted into the bloodstream, systemic complications such as bacteraemia (the spread of bacteria in the blood), acute respiratory distress syndrome (ARDS), fluid build-up in the lungs, gastrointestinal bleeding and kidney failure can occur.
A systemic inflammatory response syndrome (SIRS) can also develop, leading to the development of systemic shock. Eventually, the mediators of inflammation can be so overwhelming that circulatory instability and death follow.
In acute pancreatitis, parenchymal edema and necrosis (death) of fat around the pancreas occurs first. This is known as acute edematous pancreatitis.
When necrosis progresses to the pancreas itself, bleeding and loss of gland function occurs. Inflammation develops into hemorrhagic or necrotizing pancreatitis.
Causes
Long-term alcohol consumption and gallstone disease cause most cases of acute pancreatitis (see chart below), but many other etiological factors are known.
In 10-30% of cases, the cause is unknown. However, studies suggest that up to 70% of cases of idiopathic pancreatitis (pancreatitis of unknown cause) arise from bile duct microlithiasis.
Bile duct disease
Gallstones are one of the most common causes of acute pancreatitis in most developed countries (accounting for approximately 40% of cases). They pass into the bile duct and settle temporarily in the outlet of the bile duct into the small intestine.
The risk of a stone causing pancreatitis is inversely proportional to its size.
It is thought that injury to the acinar cells occurs secondary to increasing pressure in the pancreatic duct to the intestine (it is common with the biliary duct) caused by blockage by gallstones. However, this has not been definitively proven in humans.
Occult microlithiasis is probably responsible for most cases of idiopathic acute pancreatitis.
Alcohol
Alcohol use is a major cause of acute pancreatitis (accounting for at least 35% of cases). At the cellular level, ethanol leads to intracellular accumulation of digestive enzymes and their premature activation and release, with subsequent destruction of the cell.
The disease most often develops in patients whose alcohol use has been habitual for 5-15 years. Alcoholics are usually admitted with an acute flare of chronic pancreatitis.
Occasionally, however, pancreatitis may develop in a patient with a weekend habit. A few cases have also arisen because of a single large amount of alcohol ingested on one occasion that triggered the first attack.
Yet the alcoholic who drinks habitually remains the rule rather than the exception for the development of pancreatitis.
There is currently no generally accepted explanation for why some alcoholics are more prone to develop acute pancreatitis than other alcoholics who drink similar amounts.

Endoscopic retrograde cholangiopancreatography
Pancreatitis occurring after endoscopic retrograde cholangiopancreatography (ERCP) is probably the third most common type. It accounts for approximately 4% of cases.
The risk of pancreatitis after ERCP is around 5%.
The risk of acute pancreatitis after ERCP increases if the endoscopist is inexperienced. Massive intravenous hydration before the procedure has consistently been shown in studies to prevent pancreatitis after ERCP.
Recently, the rectal suppository indomethacin has been used. It has been shown to reduce the incidence of pancreatitis after ERCP, and is now widely accepted in most institutions.
Trauma
Abdominal trauma causes elevated levels of the pancreatic enzymes amylase and lipase in 17% of cases and clinical pancreatitis in 5% of cases.
Pancreatic trauma occurs more frequently with open abdominal injuries (e.g., knives, bullets) than with blunt abdominal trauma (e.g., from steering wheels, horses, bicycles).
Blunt trauma to the abdomen or back can crush the gland through the spine, resulting in injury to the pancreas.
Medication
Drug-induced pancreatitis has a relatively rare occurrence (approximately 2% of cases), probably related to an unknown predisposition. Fortunately, drug-induced pancreatitis is usually mild.

Drugs 100% associated with acute pancreatitis include:
- azathioprine
- sulfonamides
- tetracycline
- valproic acid
- methyldopa
- estrogens
- furosemide
- 6-mercaptopurine
- 5-aminosalicylic acid compounds
- corticosteroids
- octreotide
Drugs possibly associated with acute pancreatitis include:
- chlorthiazide and hydrochlorothiazide
- metronidazole
- nitrofurantoin
- piroxicam
- procainamide
- chlorthalidone
- combination drugs for cancer chemotherapy
- cimetidine
- cisplatin
- diphenoxylate
In addition, there are many drugs that are reported to cause acute pancreatitis in isolated or sporadic cases.
Less common causes
The following causes account for less than 1% of cases of pancreatitis:
Infection
Pancreatitis, especially in children, can be caused by several infectious diseases. These cases of acute pancreatitis tend to be milder than cases of acute biliary or alcohol-induced pancreatitis.
Viral causes include mumps virus, coxsackievirus, cytomegalovirus, hepatitis virus, Epstein-Barr virus, echovirus, varicella-zoster virus, measles virus and rubella virus.
Bacterial causes include mycoplasma, salmonella, campylobacter and tuberculosis.
Globally, childhood roundworm is also a recognised cause of pancreatitis.
Pancreatitis is associated with AIDS. However, it can result from associated infections, tumors, disorders of fat metabolism, or drugs.
hereditary pancreatitis
Hereditary pancreatitis is a genetic disorder in which a mutation in a gene causes premature activation of trypsinogen to trypsin. There are other mutations that can cause acute pancreatitis. These include cystic fibrosis.
Hypercalcemia - elevated calcium levels
Hypercalcemia from any cause can lead to acute pancreatitis. Causes of hypercalcemia include increased parathyroid function, excessive doses of vitamin D, congenital hypercalcemia.
Hypertriglyceridaemia - increased levels of fats in the blood
Clinically significant pancreatitis usually does not occur until a person's serum triglyceride level reaches 30 mmol/L.
Most authors believe that it is an inborn error of lipid metabolism rather than pancreatitis that causes hyperlipidemia. This type of pancreatitis tends to be more severe than disease caused by alcohol or gallstones.
Tumors
Obstruction of the pancreatic drainage system by a pancreatic tumour can cause acute pancreatitis. The probability of pancreatitis occurring when a tumour is present is approximately 14%.
Toxins
Exposure to organophosphate insecticide can cause acute pancreatitis. Scorpion and snake bites can also be a cause. In Trinidad, the scorpion bite Tityus trinitatis is the most common cause of acute pancreatitis.
Surgical interventions
Acute pancreatitis can occur in the postoperative period of various surgical procedures. An example is abdominal or heart bypass surgery, which can damage the gland by causing pancreatic insufficiency.
Postoperative acute pancreatitis is often difficult to confirm. It has a higher complication rate than pancreatitis associated with other aetiologies. The mechanism is unclear.
Vascular abnormalities
Vascular factors such as anemia or inflammation of the vascular system may play a role in the development of acute pancreatitis.
Inflammation of the vascular system may predispose patients to pancreatic anaemia, particularly in patients with polyarteritis nodosa and systemic lupus erythematosus.
Autoimmune pancreatitis
Autoimmune pancreatitis, a relatively newly described entity, is an extremely rare cause of acute pancreatitis. When it does cause acute pancreatitis, it is usually in young people (approximately 40 years of age) who may also suffer from other autoimmune diseases.
The pathogenesis is unclear but potentially related to immunoglobulin (Ig) G4 autoimmune disease.
Risk factors
Factors that increase the risk of pancreatitis include:
- Excessive alcohol consumption - Research shows that heavy alcohol drinkers are at increased risk of pancreatitis. This includes people who consume four to five alcoholic drinks a day.
- Cigarette smoking - Smokers are on average three times more likely to develop chronic pancreatitis compared to non-smokers, but also have a higher risk of acute pancreatitis. The good news is that if you quit smoking, your risk is reduced by about half.
- Obesity - You are more likely to get pancreatitis if you are obese.
- Diabetes - If you have diabetes, your risk of pancreatitis increases.
Symptoms
The main symptom of acute pancreatitis is severe pain that suddenly appears in the middle of your abdomen.
This severe pain often worsens over time and can spread towards your back.
Do you have pain in your upper abdomen and under your left ribs?
Read article Pain under your left rib: Is it a sign of a disease?

Other symptoms of acute pancreatitis include:
- feeling sick or nauseous - vomiting
- diarrhea
- indigestion
- high temperature - 38 °C or more
- yellowing of the skin and eyes (jaundice)
- abdominal tenderness or swelling
- fast heartbeat (tachycardia)
Practical advice:
Eating or drinking can make you feel worse very quickly, especially if you eat fatty foods. Leaning forward or curling up in a ball can help ease the pain, but lying on your back often makes it worse.
Acute pancreatitis caused by gallstones usually develops after eating a large meal. If the condition is caused by alcohol, the pain often develops 6 to 12 hours after consuming excessive amounts of alcohol.
Acute pancreatitis is divided into:
- Mild acute pancreatitis, which is characterized by the absence of organ failure and local or systemic complications.
- Moderate acute pancreatitis, which is characterised by transient organ failure (resolves within 48 hours) and/or local or systemic complications without persistent organ failure (>48 hours).
Diagnostics
Acute pancreatitis is confirmed by history, physical examination and usually a blood test (amylase and lipase). Blood levels of amylase or lipase are typically elevated to 3 times normal levels during acute pancreatitis.
In some cases, blood tests are not elevated and the diagnosis is still questionable. In such cases, abdominal imaging such as computed tomography (CT) may be performed.
Testing
Once the diagnosis is confirmed, certain imaging tests may be performed during or after the patient's hospitalization to help identify the cause of acute pancreatitis. Such tests include:
Transabdominal ultrasound
This is commonly performed during hospitalization to specifically evaluate whether the gallbladder contains stones. Gallstones are the most common cause of acute pancreatitis.

Endoscopic ultrasound
This examination is not commonly required during acute pancreatitis. Compared to transabdominal ultrasound, it is relatively more invasive in that the physician inserts a flexible thin tube into the stomach.
A camera and ultrasound probe are attached to the end of the tube. This allows the doctor to look at images of the gallbladder, pancreas and liver.
The images are more sensitive than transabdominal ultrasound images in detecting small stones in the gallbladder and bile ducts that may have been missed. It can also visualize the pancreas for abnormalities.
Magnetic resonance cholangiopancreatography
Magnetic resonance cholangiopancreatography uses magnetic resonance imaging (MRI). It is a non-invasive procedure that produces cross-sectional images of parts of the body. The technician injects dye into the patient's veins, which helps to image the pancreas, gallbladder, and bile ducts.
This is another sensitive test to evaluate the gallbladder, bile ducts and pancreas for causes of acute pancreatitis.
Computed tomography (CT)
A CT scan is a non-invasive X-ray examination that takes 3-dimensional images of parts of the body.
It is not usually performed initially during an episode of acute pancreatitis. It may be performed when the diagnosis is uncertain or several days after hospitalization. It helps to evaluate the extent of pancreatic damage when the patient is not recovering as quickly as expected.
Tento článok vznikol vďaka podpore spoločnosti Hemp Point CBD Slovensko.
How it is treated: Acute pancreatitis - inflammation of the pancreas
Treatment of acute pancreatitis: drugs, diet, antibiotics, ERCP to surgery
Show moreAcute pancreatitis is treated by
Other names
Interesting resources










