- Saguil A (November 2017). "Herpes Zoster and Postherpetic Neuralgia: Prevention and Management". American Family Physician. 96 (10): 656–63.
- Lopez A, Harrington T, Marin M (2015). "Chapter 22: Varicella". In Hamborsky J, Kroger A, Wolfe S (eds.). Epidemiology and Prevention of Vaccine-Preventable Diseases (13th ed.). Washington D.C.: U.S. Centers for Disease Control and Prevention (CDC). ISBN 978-0990449119. This article incorporates text from this source, which is in the public domain.
- "Shingles (Herpes Zoster) Signs & Symptoms". Centers for Disease Control and Prevention (CDC). 1 May 2014. Archived from the original on 26 May 2015. Retrieved 26 May 2015.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Cohen JI (18 July 2013). "Clinical practice: Herpes zoster". The New England Journal of Medicine. 369 (3): 255–63. doi:10.1056/NEJMcp1302674. PMC 4789101. PMID 23863052.
- Kahan S (2003). In a Page Medicine. Lippincott Williams & Wilkins. p. 215. ISBN 9781405103251.
- GBD 2015 Mortality and Causes of Death Collaborators (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- Rajendran A, Sivapathasundharam B (2014). Shafer's textbook of oral pathology (Seventh ed.). p. 351. ISBN 9788131238004.
- Gagliardi, Anna Mz; Andriolo, Brenda Ng; Torloni, Maria Regina; Soares, Bernardo Go; de Oliveira Gomes, Juliana; Andriolo, Regis B.; Canteiro Cruz, Eduardo (7 November 2019). "Vaccines for preventing herpes zoster in older adults". The Cochrane Database of Systematic Reviews. 2019 (11). doi:10.1002/14651858.CD008858.pub4. ISSN 1469-493X. PMC 6836378. PMID 31696946.
- Dworkin RH, Johnson RW, Breuer J, Gnann JW, Levin MJ, Backonja M, et al. (2007). "Recommendations for the management of herpes zoster". Clin. Infect. Dis. 44 Suppl 1: S1–26. doi:10.1086/510206. PMID 17143845
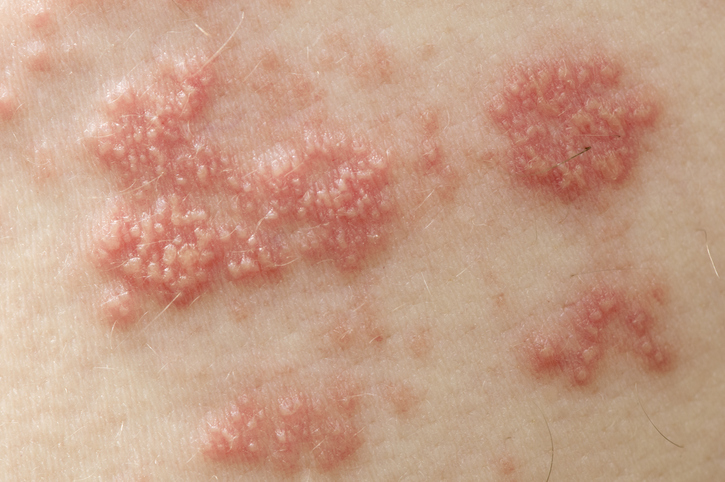
Shingles: Herpes Zoster Transmission, Symptoms, Treatment and Complications

Photo source: Getty images
Most common symptoms
- Malaise
- Skin pain
- Nerve pain
- Eye Pain
- Painful Lymph Nodes
- Fever
- Increased body temperature
- Nausea
- Depression - depressed mood
- Hyperpigmentation
- Rash
- Indigestion
- Concentration disorders
- Blisters
- Buds
- Muscle weakness
- Itchy skin
- Fatigue
- Anxiety
- Vomiting
- Reddened skin
- Deterioration of vision
- Enlarged lymph nodes
Show more symptoms ᐯ
Treatment of shingles: Pain medication and antivirals
Show moreShingles is treated by
Other names
Herpes zoster