- Moore, Jonathan (September 1, 2008). "Creating the Ideal Microcosm for Rapid Incorporation of Bioengineered Alternative Tissues Using An Advanced Hydrogel Impregnated Gauze Dressing: A Case Series". The Foot & Ankle Journal. doi:10.3827/faoj.2008.0109.0002.
- Violi, F; Basili, S; Berger, JS; Hiatt, WR (2012). Antiplatelet therapy in peripheral artery disease. Handbook of Experimental Pharmacology. 210. pp. 547–63. doi:10.1007/978-3-642-29423-5_22. ISBN 978-3-642-29422-8. PMID 22918746.
- "What Are the Signs and Symptoms of Peripheral Arterial Disease?". nhlbi.nih.gov. August 2, 2011. Archived from the original on February 25, 2015. Retrieved February 26, 2015.
- "What Is Peripheral Arterial Disease?". nhlbi.nih.gov. August 2, 2011. Archived from the original on February 25, 2015. Retrieved February 25, 2015.
- "What Is Peripheral Vascular Disease?" (PDF). American Heart Association (heart.org). 2012. Archived (PDF) from the original on April 12, 2015. Retrieved February 26, 2015.
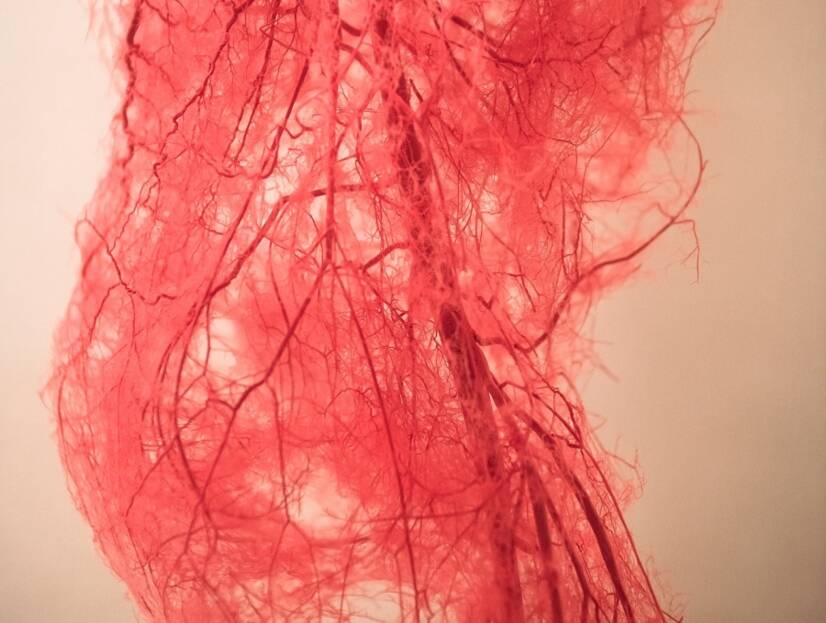
Peripheral artery disease (PAD) is the narrowing of the arteries to the legs, stomach, arms and head.
- "What Causes Peripheral Arterial Disease?". nhlbi.nih.gov. August 2, 2011. Archived from the original on February 25, 2015. Retrieved February 26, 2015.
- Fowkes, FG; Rudan, D; Rudan, I; Aboyans, V; Denenberg, JO; McDermott, MM; Norman, PE; Sampson, UK; Williams, LJ; Mensah, GA; Criqui, MH (October 19, 2013). "Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis". Lancet. 382 (9901): 1329–40. doi:10.1016/s0140-6736(13)61249-0. PMID 23915883. S2CID 38652734.
- "How Is Peripheral Arterial Disease Diagnosed?". August 2, 2011. Archived from the original on April 7, 2015. Retrieved March 27, 2015.
- Ruiz-Canela, M; Martínez-González, MA (2014). "Lifestyle and dietary risk factors for peripheral artery disease". Circulation Journal. 78 (3): 553–9. doi:10.1253/circj.cj-14-0062. PMID 24492064.
- "How Is Peripheral Arterial Disease Treated?". nhlbi.nih.gov. August 2, 2011. Archived from the original on February 25, 2015. Retrieved February 26, 2015.
Peripheral Artery Disease: Causes, Symptoms, Prevention and Treatment
Peripheral artery disease is a term for diseases of the arteries that supply various parts of the body. Blood vessels are usually damaged due to atherosclerosis, but it is not the only cause.
Most common symptoms
- Malaise
- Feeling of heavy legs
- Loss of pubic hair
- Abdominal Pain
- Limb pain
- Leg Pain
- Muscle Pain
- Ulcer
- Blue leather
- Muscle stiffness
- Defence
- Swelling of the limbs
- The Island
- Tingling
- Slow wound healing
- Cold extremities
- Muscle weakness
- Muscle cramps
- Itchy skin
- Fatigue
- Reddened skin
Characteristics
More specifically, PAD is about diseases of peripheral blood vessels, i.e. all arteries other than those that supply the heart or brain.
FAQ:What kind of disease is it and why does it occur?How does it manifest itself and what are the risks of arterial involvement and insufficient blood supply?Why is it also called "obliterative"?How is it treated?
The peripheral artery system supplies oxygen to parts of the body such as the neck, head, upper limbs, abdomen, kidneys and lower limbs.
One of the names of the disease found in medical literature is peripheral obliterative arteriopathy. What does the expression even mean?
Peripheral = away from the centre: in the vascular system, it is arteries other than those that supply the heart or brain.
Arterio = relating to an artery or arteries. It refers to those vessels that carry blood from the heart and usually carry oxygen-saturated blood.
Obliterative = causing or accompanied by closure or collapse of a lumen obliterative arterial disease. In this case, it indicates the process of narrowing of the vessels, more precisely their internal lumen.
A progressive disease,
which can result in vascular obstruction
and
insufficient blood supply to an organ or a tissue.
Over time, the blood vessels become impassable, causing a disruption of the blood supply and oxygenation of the affected part, tissue, organ or limb.
Restriction in blood supply = ischemia, with consequent tissue or organ damage.
Peripheral vascular disease is reported to be mainly caused by an atherosclerotic process, i.e. by hardening of the arteries.
Atherosclerosis is a disease in which certain substances are deposited in the walls of blood vessels. They do not normally belong there.
So, as a result...
The space inside the artery thus gradually narrows. In addition, the vessel wall hardens, thus losing elasticity. The common result is partial or complete occlusion of the vessel.
However, this is not the only cause behind peripheral vascular disease.
Bleeding has a number of different symptoms. Their severity and overall course depends on several factors. This is, for example, the extent of insufficient blood flow, the rate at which the occlusion of a vessel or the area of blood supply occurred.
Well-known examples are ischemic heart disease, heart attack or stroke.
The above examples do not belong to the group of peripheral vascular diseases.
Peripheral Arteries Are...
The heart pumps blood to the aorta, from which it progresses to the whole organism. The peripheral vascular system includes other parts of the body outside the heart and aorta itself.
This includes all blood vessels, such as the arteries of the subclaves, the upper limbs, the blood supplying the head through the neck, the blood leading to the abdominal organs, the kidneys and those leading to the lower limbs.
Arteries are blood vessels that carry blood from the heart to tissues and organs.
They are usually filled with blood, which is oxygenated, i.e. rich in oxygen.
Except the lung artery.
The lungs are an artery that protrudes from the right ventricle and leads deoxygenated blood to the lungs, where it is reoxygenated.
Pulmonary veins are similar.
They move from the lungs and carry the oxygenated blood back to the left side of the heart. The veins are therefore the vessels that flow towards the heart.
The arteries have a different vascular wall composition than the veins.
The artery wall consists of three layers. The thickest is the middle muscle layer. It is both strong and flexible.
Its composition is also important because of the pressure created by the heart during its contraction and the distribution of blood throughout the human body.
Large arteries branch into smaller arteries that run into tissues, organs, and parts of the body. The final vascular sections are the small arteries.
The arteries transition into the capillary system, which are the smallest vascular bodies. They supply nutrients.
Oxygen + nutrients are transferred here and back as they also receive the products of metabolism.
Next, the blood continues into the venous system. In this way, deoxygenated blood returns to the right part of the heart so that it can pass to the lungs. It is subsequently oxidized in the lungs.
And so it goes indefinitely.
Want to know more?
What is peripheral artery disease?
What causes it?
How does it manifest?
What is the treatment and how can it be prevented?
Peripheral Artery Disease Affects the Arteries
It is a disease that affects all arteries, except the coronary vessels, i.e. the vessels that supply the heart.
The abbreviation PAD is sometimes used.
PAD is one of the most common diseases affecting the world's population.
When the arteries are damaged, there is a disturbance of the blood supply, ie the supply of oxygen and nutrients.
There is a disparity between:
Tissue needs : supply of oxygen and nutrients.
This results in a disorder in the tissue, organ or part of the body.
The disease is chronic and progressive, meaning that it takes place over a long period of time and progresses over time - it worsens.
Acute forms of arterial occlusion do not fall into the category of peripheral arterial disease.
Moreover, PAD is a systemic disease.
What does that mean?
Several arteries of the human body are damaged = global impact. However, the disability can vary in degree and extent.
The presence of PAD is said to indicate a possible involvement of the arteries of the heart or brain. And it is also a marker of the development of a heart attack, stroke or sudden death.
According to expert research, people over the age of 62 are affected by two or three vascular streams at the same time. These are mostly coronary arteries and arteries of the lower extremities. To a lesser extent along with damage to the blood vessels of the brain.
Lower limb PAD + coronary heart disease.
Lower limb PAD + cerebrovascular disease.
Lower extremity PAD + coronary heart disease + cerebrovascular disease.
Atherosclerosis is identified as the most common problem behind peripheral arterial disease. However, other disease states also cause the disease.
An example is the comparison of PAO between two parts of the body.
90% of PAD of the lower limbs (DK) is caused by atherosclerosis.
Compare...
Upper limb PAD causes atherosclerosis only rarely.
Lower extremity PAD is one of the most common forms of the disease.
That is why it draws so much attention.
Causes
Atherosclerosis is a long-term progressive process. It runs systemically, which means a total disability of several, not just one, arteries.
Deposits of fat and other substances are deposited in the walls of the arteries. So-called atherosclerotic plaques are formed.
This process causes an inflammatory reaction, or a plaque thrombosis, or blood clot.
Gradual hardening, narrowing of blood vessels and loss of their elasticity is the basis for a disease state of insufficient blood supply.
Current need and inability to ensure the desired supply of oxygen and nutrients = problematic.
This results in various difficulties. These are manifested according to the specific place, extent or time in which the blood flow disorder occurred.
There are also acute forms, i.e. sudden states insufficient blood supply.
However, the term peripheral arterial disease also includes chronic forms that are chronically progressive and ongoing.
The disease significantly negatively affects the quality of life.
If the lower limbs are affected, a part of it may be amputate.
The most common causes of PAD are:
- atherosclerosis of the arteries, especially the lower extremities
- artery inflammation
- primary and secondary vasculitis of the upper and lower limbs
- in rheumatic systemic inflammation
- in infectious diseases
- in a tumourous process
- after taking medication
- after radiation
- after a transplantation
- primary and secondary vasculitis of the upper and lower limbs
- cystic adventitial disease
- rare disease of the outer layer of the vessel
- one or more cysts arch into the lumen of the vessel, thereby impairing blood flow
- fibromuscular dysplasia
- congenital (inborn) disease
- vascular lining disease
- mainly in women
- It mainly affects the blood vessels in the abdomen and kidneys
- compression syndromes - cause compression of the artery
- injury
- vascular dissection - cracking of the vascular wall
- mechanical effects
- cold and humidity long-lasting effect of cold in connection with humidity, wind
- vibration - when using vibration tools
- iatrogenic arterial damage - caused by medical treatment
- thrombosis and embolism are less common causes, more often causing an acute problem
- Trombangitis obliterans or Buerger disease
- especially in young smokers
- unclear cause
- inflammatory artery disease
In peripheral arterial disease is concerned, there are certain risk factors associated with the most common causes. As such, there are modifiable and non-modifiable risk factors.
Non-modifiable risk factors include:
- age - the risk of developing the disease increases with age
- in men over 45 years and in women over 55 years
- approximately 20% of the population over the age of 70
- PAD of lower limbs 5-10 % of the population above 60
- sex - men are more at risk of atherosclerosis
- the risk is also higher in postmenopausal women
- heredity - family occurrence increases the risk
Modifiable factors:
- smoking - the most serious risk factor
- the risk of vascular occlusion is 3 times higher in smokers than in non-smokers
- quitting smoking is very important in diseases of the cardiovascular system
- increased fat levels and impaired fat metabolism
- high-fat diet
- HLP or hyperlipoproteinaemia with cholesterol levels greater than 5.18 is an increasing risk
- LDL or Low Density Lipoprotein Cholesterol Level above 3,37 mmol/l
- obesity
- high blood pressure - hypertension - increases the risk
- diabetes - poorly or insufficiently treated diabetes, or neglect of treatment
- vitamin B6 and folic acid deficiency, B9 - reduced level = decreased vitamin levels increased plasma homocysteine concentration - hyperhomocysteinemia = risk of vascular endothelial damage
- lack of physical activity
- stress
- Hyperfibrinogenemia - increased fibrinogen levels in the blood
- hyperuricaemia - gout
Learn more in the article on the effects of the Mediterranean diet on human health.
Table: percentage of risk factors by sex
| Men | % | Women | % |
| Smoking | 97 | Hypertension | 77 |
| High cholesterol | 37 | Smoking | 53 |
| Hypertension | 20 | High cholesterol | 45 |
| Diabetes | 12 | Diabetes | 17 |
Symptoms
They depend on the site where the vessel narrowed critically, on the extent and part that is supplied with blood, and last but not least on the time period in which the vessel occluded.
Ischemia can be an acute condition caused by thrombosis or embolism.
In thrombosis, platelets and other components of hemocoagulation accumulate on the atherosclerotic plaque. The vessel can thus become partially or completely clogged.
An embolism ioccurs due to a blood clot, or other foreign object, in the bloodstream that goes into another part of the body, for example when a blood clot formed in the heart is carried into the brain, abdominal organs, kidneys or the lower limbs.
Chronic conditions, such as progressive PAD over time.
Table: example of vascular disease by area
| Site | Description |
| Cervical, vertebral and cerebral vessels |
|
| Upper limb |
|
| Mesenteric artery |
|
| Renal artery |
|
| Lower limb |
|
Interestingly, diseases of the vascular system affect millions of people, and three-quarters of them have had no problems. They occur at a higher age.
Peripheral Arterial Disease of the Lower Extremities
One of the most common forms of PAD is a disorder in the lower limbs.
Thus, ischemic limb disease can be acute or chronic. And long-term disease falls into the group of PAD diseases.
Vessel involvement arises for a variety of reasons, mainly due to atherosclerosis.
In the past, the term for the chronic form of lower extremity bleeding and the term "lower limb ischaemia" was used. However, this term applies to a disease with a clinical picture.
PAD covers a wide range of diseases, for a variety of causes, even in the early stages of the disease, which can be completely asymptomatic.
The progression of the disease leads to a characteristic condition.
Manifestations of PAD of the lower extremities are characteristic ...
The sufferer experiences difficulties when walking and limb pain.
When the upper limb is affected, its mobility will also be limited.
Claudication
A question:
What is claudication?
The word means "a limp".
Claudication = limping.
This type is typically manifested during exertion. When walking, the need for oxygen and nutrients increases with the muscles of the lower limb.
There is pain in the leg that forces the affected person to stop. Before that happens, the suffere may have slowed down walking or started limping.
After a period of rest, the difficulties subside, usually within 4 minutes.
This type of pain resembles angina pectoris - exertional chest pain in a cardiovascular disease.
After some rest, one is able to cross a certain section again. This is done due to lower blood supply.
Claudicatio intermittens = might be translated as "intermittent vascular (or arterial) claudication".
Intermittent bleeding was described in horses by vets in 1831.
In 1858, the French physician Jean-Martin Charcot described the condition in people.
These are mostly the same distances.
In the event that a given section shortens or the intensity and onset of difficulties worsen, the progression of the condition must be considered.
The onset of claudication in the lower limb will be affected by:
- walking speed
- ambient temperature - cold that narrows blood vessels
- smoking
- terrain, the more complicated, the more muscle effort
- walking up and down the stairs
- level of physical exertion
The long-term development of the disease also affects the formation of the so-called collateral circulation. These are the newly formed vascular vessels that partially supply the bloodless area.
In this case, claudication pain occurs, but the person is able to continue walking despite the pain. He slows down his walk and the pain subsides over time.
Rest Pain
Another example is typical rest pain.
For example, limb pain occurs at rest, in a horizontal position and at night.
The cause is a reduction in blood flow as the hydrostatic pressure in the lower limb decreases in the horizontal position.
The relief of this type of pain occurs after standing up or dangling the limbs off the mat, which will increase the hydrostatic pressure and improve blood flow to the muscles of the lower limb.
Deterioration of Issues and the Onset of Rest Pain
Rest pain usually indicates a worsening of the arterial system. The end portions of the vessels are so damaged that circulation is disturbed in the target tissue, such as the lower limb muscle.
This is when pain gets intense and unbearable.
In this case, the pain is reported in the leg:
- toes
- upper part of the foot
- on the sole
- knuckles
If there is intense pain in the lower leg or the thigh, it may be an acute artery occlusion.
Rest pain in PAD of the lower extremities occurs in stages 3 and 4.
The Fontaine Classification of Peripheral Arterial Disease
Several methods are used to classify the disease and its stage. However, the most recommended classification is Fontaine.
Table: Fontaine classification of the disease
| Stadium | Description |
| Stage I - asymptomatic |
|
| Stage II - claudication |
|
| Stage II - rest pain |
|
| Stage II - trophic defects |
|
Diabetes + PAD
Be careful in case of diabetes.
Another condition is damaged blood vessels with concomitant diabetes.
Diabetes develops a condition called polyneuropathy, which is nerve damage.
In this case, the affected person does not have to feel any pain, even in the case of severe vascular damage.
And, in turn...
Neuropathy itself can cause problems resembling peripheral arterial disease. At the same time, the blood vessels are undamaged.
However, more often, both diseases are combined into a condition referred to as:
neuroischemic limb.
Critical Limb Ischemia
A condition in which there is a risk of limb amputation due to a reduced blood supply.
The disease is abbreviated as CLI - Critical Limb Ischemia.
It is also known as:
Chronic limb threatening ischemia (CLTI).
Chronic limb ischemia progresses in approximately 15 to 30% to critical limb ischemia.
Mortality in CLI is reported to be 12% within year 1, 42% within 5 years, and 65% within 10 years. Another reason is the participation of other diseases of the cardiovascular system.
Symptoms of critical limb ischemia:
- resting limb pain - lasting for 2 weeks
- wound formation that does not heal
- ulcerations - ulcer formation
- or gangrene - dead tissue
- absence of pulsation on the arteries of the legs or pulse weakening
- or the presence of murmurs on the arteries and. femoralis or a. poplitea
- sudden onset of CLI
- skin changes
- pale, blue to purple discolouration
- cold skin
- skin changes
In acute limb ischemia (ALI) there is a risk of limb amputation. It occurs in conditions such as embolization, thrombosis of the artery wall or injury.
It is a sudden deterioration of the condition or an acute condition.
The extent of the wound, tissue loss and the presence of infection also affect the outcome.
All Possible Symptoms Summarised
A summary of symptoms in peripheral arterial disease, which may occur in various combinations.
Table: Symptoms
|
|
Swelling of the limb may not be present.
Diagnostics
So, medical history is important + subjective difficulties include claudication and other already mentioned manifestations.
This is followed by a physical check-up, skin condition, color, skin quality and the presence of a defect. It also includes the detection of arterial pulsations and the presence of murmurs. Tactile, positional tests and functional tests (treadmill examination) are added.
The ankle-brachial index test (ABI) is performed. Ankle pressure is measured using Doppler ultrasonography.
The following groups of people should be tested for ABI:
- smokers over 50 years of age
- people over 70 years of age
- people with atherosclerosis and other cardiovascular disease
- people with diabetes
- people with hypertension - that is, people with high blood pressure
- people with high cholesterol
- people with claudication (pain)
- people with limb pain with no apparent cause
It is also necessary to determine the total pressure conditions in lower limbs.
Doppler examination is especially important - duplex or triplex USG.
Imaging methods include:
- colour duplex sonography
- CT and MRI angiography
- termography
- invasive methods such as intravascular ultrasound and angioscopy, angiography
It is also necessary to perform a laboratory blood test, such as blood count, blood clotting and biochemical properties.
Differential diagnosis is performed in order to distinguishing a particular disease or condition from others that present with similar clinical features, e.g. venous diseases, post-thrombotic syndrome, neurogenic pain, osteoarthritis or muscle pain and others.
Learn more in articles on venous diseases:
Course
The early stages of the disease do no always present with signs and symptoms. This stage is called asymptomatic, i.e. showing no symptoms.
Subjective difficulties in the onset of the disease are not always present.
Mild symptoms, such as feeling cold in the limbs or tingling in the limb, may occur during this period.
The disease imay be detected accidentally by detecting a murmur above the arteries during the examination.
The clinical picture develops later on, which includes claudication (pain) and difficulty walking.
The extent and intensity depends on several factors as well as on the overall physical activity.
Oxygen and nutrients needed for muscle work are not sufficiently supplied to the target tissues. This is manifested by ischemic pain, i.e pain due to a restriction in blood supply.
If the exertion or walking stop, the pain is relieved within a few minutes.
The person is able to walk again.
The pain causes the creasing, which is why this symptom was named.
Vascular claudication (pain) = claudicatio intermittens.
The progression of the disease or the worsening of the condition in a shorter period of time means rest pain. It starts regardless of the exertion.
It may be painful when the lower limbs are positioned horizontally.
Horizontal positioning at night is also problematic. The person wakes up from sleep and is able to g oback to sleep in a sitting position to somewhat relieve the pain.
This is because the position increases the hydrostatic pressure in the limb. This partially improves blood flow to the tissues.
In the long run, non-blood supply to the lower limbs is a problem that will also cause damage to the skin, subcutaneous tissue and other structures.
Therefore, over time, skin changes may occur. These are manifested by a change in skin colour. The skin may be colder, paler or darker, blue to purple.
Sudden paleness and coldness of the skin indicate an acute form of limb bleeding.
The most difficult stage is the formation of deep defects. Wounds heal very in a complicated manner or do not heal at all.
The complication is a wound infection.
The final stage, i.e. necrosis or gangrene, which is a risk for limb amputation. The necessity and degree of amputation is assessed according to the extent of the affected tissue and the damage to the arteries of the lower limbs.
Another form is an acute condition. However, it does not fall under PAD.
The acute form has an abrupt onset, even without previous difficulties. The cause may be embolism or sudden thrombosis. Embolism can occur after a blood clot has left the heart, for example.
How it is treated: Peripheral Artery Disease
Treatment and medication of peripheral artery disease
Show morePeripheral Artery Disease is treated by
Peripheral Artery Disease is examined by
Other names
Interesting resources
Related










