- klinickafarmakologie.cz - Treatment of tibial ulcer with moist therapy
- solen.cz - Pain in tibial ulcers and their treatment
- dermatologiepropraxi.cz - Tiber Ulcer
- prolekare.cz - Venous tibial ulcer - etiopathogenesis, clinical signs and surgical treatment
- prolekare.cz - Treatment of chronic tibial ulcer of venous etiology
- prolekare.cz - Acute and chronic wounds - etiology, differences in healing and treatment
- remedia.cz - Healing of tibial ulcers
- prolekare.cz - Overview of recommendations in the prevention and treatment of tibial ulcers
- prolekare.cz - Surgical treatment of venous tibial ulcers
Tiber ulcer: what is it, how does it manifest itself and what does it look like?
Many of us are familiar with a tibial ulcer, at least from hearsay. Let's take a closer look at the causes, symptoms and treatment.
Most common symptoms
Characteristics
A tibial ulcer (ulcus cruris) is defined as a chronic wound that extends various depths into the skin and subcutaneous structures.
They affect approximately 3 to 5 % of the population. Women are more likely to suffer from this condition than men.
What is a chronic wound?
A chronic wound is defined as a disruption of the continuity of the skin surface, the integrity of the body, a change in the anatomical structure and associated skin function. The healing time is usually longer than 6 weeks. It can arise from any wound.
Chronic wounds include:
- tibial ulcers
- diabetic ulcerations
- decubitus ulcers
- extensive burns
- amputation stumps
Many of us think it's a disease that only older people suffer from. But it can affect younger patients too.
In the over 70 age group, it occurs in approximately 4 to 5% of the population. In the case of the younger age group, approximately 1% of people suffer from the disease.
Typhoid ulcers significantly reduce the quality of life of the patient. They are not only a health problem, but also significantly affect the social, economic and psychological aspects of life.
In the case of younger age groups, the disease is the cause of long-term incapacity for work. In some cases, patients are unable to perform their original jobs. Sometimes it is the cause of disability.
Treatment of tibial ulcers is lengthy and economically demanding. Determining the cause of the disease is crucial for successful treatment.
Causes
The causes of a tibial ulcer are various. For this reason, it is referred to as a polyetiological disease.
The occurrence of an ulcer depends on many factors. These include obesity, age, congenital disposition, hypertension, diabetes mellitus, thrombosis, hormonal treatment and lifestyle.
Ulcerations of venous origin account for the largest part of the aetiological spectrum (85%). Approximately 10% are ulcerations of arterial origin. The remaining 5% of ulcerations have other causes.
In the following section we will describe the different causes of the disease:
External causes
Ulcerations caused by physical influences
- Post-traumatic ulcerations - occur as a consequence of complicated leg fractures. In most cases they are associated with major tissue loss, tissue necrosis. They are accompanied by signs of infection.
- Ulcerations of thermal origin - they are a manifestation of stage III and IV burns. They arise after the separation of blackish-brown appendages. They replicate the original extent of necrosis.
- Ulcerations of cold origin - poorly healing ulcerations in stage II frostbite mostly affect the peripheral parts of the limbs. They appear only after a certain latency period.
- Pressure ulcerations (decubital) - occur in areas subjected to increased pressure. Local ischaemia of the skin results in necrotic necrotic fascicles on the reddened areas, which gradually transform into ulcerating defects.
Ulceration due to chemical causes
Chemical causes of ulceration include acids, artificial fertilizers, plant extracts, drugs and disinfectants.
At the point of contact with the chemicals, inflammation occurs, which leads to tissue death. For example, coagulative necrosis (tissue death) is caused by concentrated alkalis. Acids cause coagulative necrosis.
Ulceration of infectious origin
Diseases that can result in a tibial ulcer include erysipelas, tuberculosis, mycoses, leprosy, stage III syphilis, herpes zoster, and others.
Arteficial ulceration
The cause of this type can be chemical substances that burn the skin. Also, the provoker of the disease can be a physical cause, for example, a cigarette burn.
Internal causes
Venous ulceration
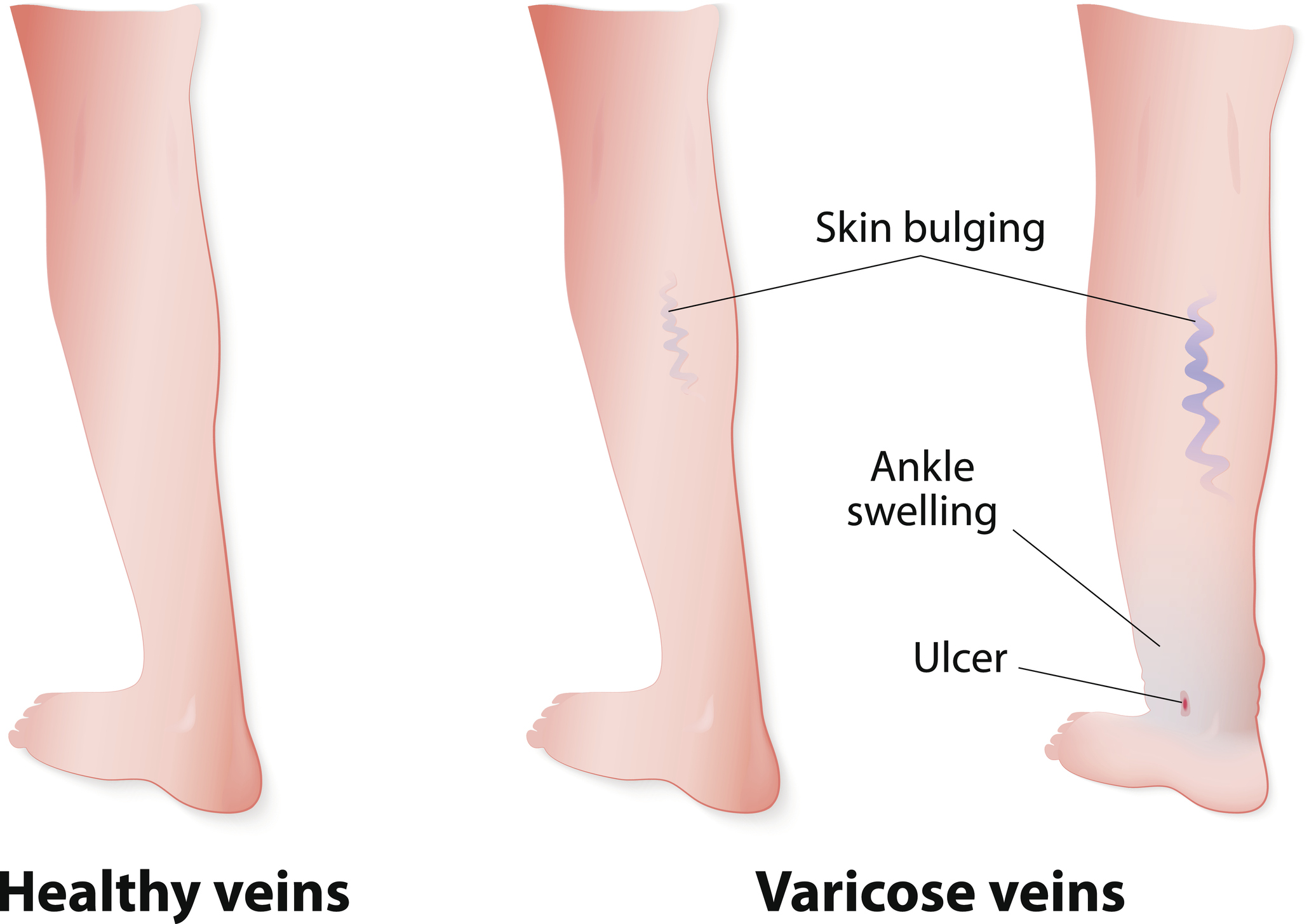
Venous ulcers are the most common (about 85%). They affect about 1% of the population. They are considered the most serious skin complication of chronic venous insufficiency.
Phlebothrombosis is generally considered to be an important risk factor for the development of skin changes and tibial ulceration. These changes are referred to as post-thrombotic syndrome.
What is chronic venous insufficiency, how does it manifest itself, does it have risks?
Arterial ulceration
It is the result of peripheral arterial disease of the lower limbs. The extent of vascular changes determines the size and speed of spread of the ulceration.
Sclerotic plaques, microthromboses, fibrosis and calcification occur on the vessel walls. Subsequently, the arterial lumen narrows, resulting in chronic ischaemia and tissue death.
What is peripheral arterial disease?
The term peripheral arterial disease refers to a group of diseases that ultimately result in reduced blood flow through the extremities. It may be present alone or in combination with other diseases.
Lymphoid ulceration
Primary and secondary lymphoedema of the legs is manifested by extensive swellings. Soft swellings gradually turn into hard ones. These have hyperkeratotic manifestations and verrucous swellings.
As a result of impaired function of the nerve fibres regulating tissue metabolism, large ulcers with strong secretion are formed.
Haematopathogenic ulceration
This type of ulceration is associated with disorders of blood components (erythrocytes, leukocytes, platelets, plasma proteins).
The main causes of ulcerations include:
- anemia
- myeloproliferative diseases - thrombocythaemia (excess platelets in the blood)
- dysproteinemia (macroglobulinemia, microglobulinemia, cryoglobulinemia)
- thrombocytopenic purpura
Ulceration in coagulation disorders
Disruption of the balance between vascular endothelium and internal hemostasis leads to severe changes in the blood clotting system.
It can also cause disturbances in diffusion and metabolism, resulting in changes underlying the development of a tibial ulcer.
Ulceration in metabolic disorders
Metabolic causes that can induce local necrosis include diabetes mellitus, accumulation of substances produced in the body (uric acid) and metabolized foreign substances (drugs).
Neuropathic ulcerations
They occur mainly in diabetic neuropathy, alcoholic neuropathy, leprosy, vitamin B1 deficiency and polyneuropathy.
Vasculitis
Vasculitides are not a common cause of the development of a tibial ulcer. Ulcerative vasculitides are caused by various drugs, infections, food or systemic diseases.
Ulcerating tumours
One of the causes of a tibial ulcer can be the breakdown of a tumor. The most common tumors that result in a tibial ulcer include basalioma, melanoma, Kaposi's sarcoma, angiosarcoma, and spinalioma.
Mixed ulcerations
Mixed tibial ulcers are quite common. They can be caused by two or more causes. The most common combination is mixed tibial ulcers of arterial and venous causes.
Symptoms
Ulcers can vary in shape and depth. The bottom of the ulcer can be black, yellow-grey-green (necrotic tissue), yellow (pus) or bright red (granulation tissue). Sometimes they can be significantly painful.
The following symptoms indicate the likelihood of occurrence:
- swelling
- increased pressure above the ankle
- brown discolouration of the skin
- lipodermatosclerosis - causes the skin, especially in the calf area, to become hard, not flexible and may turn red or brown
- white atrophy
The most common complication of the disease is contact allergy. This arises as a result of over-application of topical medications or secondary infection.
In the following section, we will describe the most commonly occurring tibial ulcers:
- venous ulcers
The typical localization of a venous ulcer is the lower legs. Venous ulcers take years to develop. Patients report that they experience a feeling of tightness and mild pain after prolonged standing. Also, a feeling of heavy legs and night cramps may occur.
Basic characteristics include:
- irregular shape
- brown pigmentation around the ulcer
- normal pulse in the foot
- Arterial ulcers
Arterial ulcers occur mainly in areas of the body that are exposed to minor trauma (for example, distal links of the fingers). In recumbent patients, they may appear in areas that are exposed to pressure (heels, ankles).
The basic characteristics of arterial ulcers include:
- a relatively regular shape
- atrophic, pale skin around the ulcer
- a weak pulse in the foot
Diagnostics
In the following section we will describe the steps of the examination.
In the first step, the physician focuses on a thorough medical history. In the next step, he performs a physical examination.
Aspexia (visual examination) of the extremities is used to detect trophic changes (dry, shiny surface, fissures in the plantar areas, condition of the trophic nails). Palpation is used to detect peripheral pulsations.
Instrumental, laboratory and histopathological examinations help to determine the exact cause of the disease. Histopathological examination is used in practice mainly to exclude a tumour aetiology of the disease.
The examination methods include:
- sonographic examination
- phlebography (venography) - an invasive imaging procedure used to visualise veins
- isotope phlebography
- arteriography - X-ray examination of the arteries
- lymphoscintigraphy - isotope examination of the lymphatic system
Additional examinations include microbiological and mycological examinations.
Course
The disease has a chronic course with recurrences. Recurrences occur in 6 to 15% of cases within one year. 50% of ulcers heal within 4 months. Approximately 20% of ulcers heal within two years.
Healing of a tibial ulcer occurs in three phases:
- Exudative (inflammatory, cleansing) phase
This phase is characterised by a complex defensive reaction of the organism. The aim of the organism is to clean the wound. Inflammation develops, characterised by swelling, redness, pain and increased temperature of the affected area.
The dilation of blood vessels (vasodilatation), increased permeability of blood vessels and the action of chemotactic factors lead to the migration of neutrophils and macrophages to the wound site.
At the same time, mediators of inflammation, cytokines, growth factors and other chemotactic factors are secreted, which activate the cells needed for healing.
What are chemotactic factors?
Chemotactic factors (chemotaxins) are defined as cells that attract neutrophils, macrophages and T-lymphocytes, or other inflammatory cells, to the site where the inflammatory reaction develops.
During the course of the inflammatory reaction, the different chemotactic factors are released at different time intervals. For example, the initial phase of acute inflammation is characterised by the presence of neutrophils. In the later phases, macrophages or T-lymphocytes appear.
- Proliferative (granulation) phase
In this phase, new blood vessels are formed (neoangiogenesis). Granulation tissue gradually fills the wound. A network of collagen fibres is formed. This network forms the basis for the subsequent process of epithelial formation.
- The epithelialisation phase
The epithelialisation phase is also referred to as the final phase of wound healing. The cells of the basal layer migrate to the surface of the skin. At the same time, they move from the edge of the wound to the centre of the wound. The maturation of the cells leads to the definitive rebuilding of the skin with individual layers and functions.
The successful healing process is influenced not only by physiological processes but also by many factors. Factors that directly affect the wound are called local factors. Factors that relate to the overall health are called systemic factors.
For example:
- collagen synthesis - in malnutrition, infection, diabetes, hypoxia
- intensity of the inflammatory response - autoimmune disease, immunodeficiency
- healing environment - hyperglycaemia in diabetes, acidosis in hypoxia, humidity
Many of these factors are interrelated. Systemic factors will have a secondary local effect that can have a negative impact on the healing process.
Conversely, mitigating the effect of local or systemic factors may result in a positive effect on the wound healing process.
For this reason, in the diagnosis and subsequent treatment we must pay attention to all factors that may be related to the wound.
In the case of a tibial ulcer, the healing process is impaired by many local and systemic factors.
The individual factors that influence the healing process are listed in the following table
| Local factors | Systemic factors |
| Localization | Underlying cause of the disease |
| Wound environment | Age |
| Wound size and depth | Nutrition |
| Local infection | Medications |
| Foreign bodies | Immune status |
| Oxygen deficiency | Pain |
| Wound dehydration | Mental state |
| Blood supply disorder | Sleep |
| Fibrin coatings | Systemic diseases |
| Necrotic tissue | Alcohol, drugs, cigarettes |
How it is treated: Tiber ulcer
Treatment of tibial ulcers: what drugs help? And what about antibiotics?
Show moreTiber ulcer is treated by
Other names
Interesting resources
Related










