Treatment of tibial ulcers: what drugs help? And what about antibiotics?
The treatment of tibial ulcer can be divided into several groups:
Local treatment
In local treatment, classical therapies and modern covering materials are used in practice. In classical therapies, moist compresses, pastes and ointments are applied.
In the form of compresses, various disinfectants (3% pine water, hypermanganese solution, superoxidized rinse solution) are applied.
Of the ointments, the ointment with iodized povidone is mainly used. The classical treatment procedure is used especially in the case of infected and significantly bacterially colonized ulcers.
Classical treatment procedures have several disadvantageous features:
- precise indications for the application of individual drugs are not established.
- the effectiveness of individual drugs is not verified by research
- most topically applied drugs contain allergens
- frequent changes of cover are necessary
- they fail to reduce wound odour
A very important part of the treatment of an ulcer is the care of the surrounding area. In the treatment of venous ulcers, eczema often forms on the surrounding skin. In this case, a poultice and topical application of a corticosteroid are applied.
Corticosteroid can also be added to a protective paste around the wound.
A more modern treatment approach is moist therapy. It is now the standard approach to treating chronic wounds. The choice of a particular type is guided by the characteristics of the particular ulcer.
Moist therapy has several advantageous features:
- it creates and/or maintains an optimal wound environment
- maintains the necessary pH and moisture
- drains and/or locks wound exudate in its structure
- stimulates autolytic wound cleansing
- protects the wound from infection
- painless wound dressing
The following table shows the different groups of moist therapy products
| Alginates |
|
| Hydrocolloids |
|
| Amorphous and compact hydrogels |
|
| Foams |
|
| Polyacrylate woven fabric cushions |
|
Have you heard that honey is used in the treatment of chronic wounds?
Medical honey is a blend of two types of honey from Australia and New Zealand. These contain glucose oxidase and bioactive ingredients from the manuka bush.
Clinical studies have shown that medicated honey reduces healing time, eliminates infections, reduces antibiotic use and ultimately reduces hospitalisation time.
Effects of medicated honey:
- Antibacterial
- anti-inflammatory
- stimulates immune function and anti-cancer activity
- reduces wound odour
In practice, medical honey is applied in the form of a plaster. Medical honey is usually applied to a calcium-alginate matrix (waterproof carrier).
The honey patch should be applied for at least 12 hours, but preferably for 24 hours. Replacing the patch in the wound depends on the stage of healing itself.
What role does silver play?
Preparations containing silver significantly improve and promote the healing process of chronic wounds. Silver particles have antimicrobial effects in a spectrum of gram-positive and gram-negative bacteria.
In practice, patches containing colloidal silver are used. They are characterised by faster and better wound healing. They create better protection against bacteria and reduce the risk of infection.
Another option is a foam patch containing ionic silver. The foam covering has a rapid antimicrobial effect.
Compressive treatment
Compression treatment is used in the case of venous ulcers. Venous ulcers heal faster when patients use compression bandages.
Elastic bandages are more effective than using a simple non-elastic bandage. Here the rule is that any compression is better than none. After the ulcer has healed, lifelong use of compression stockings is advisable.
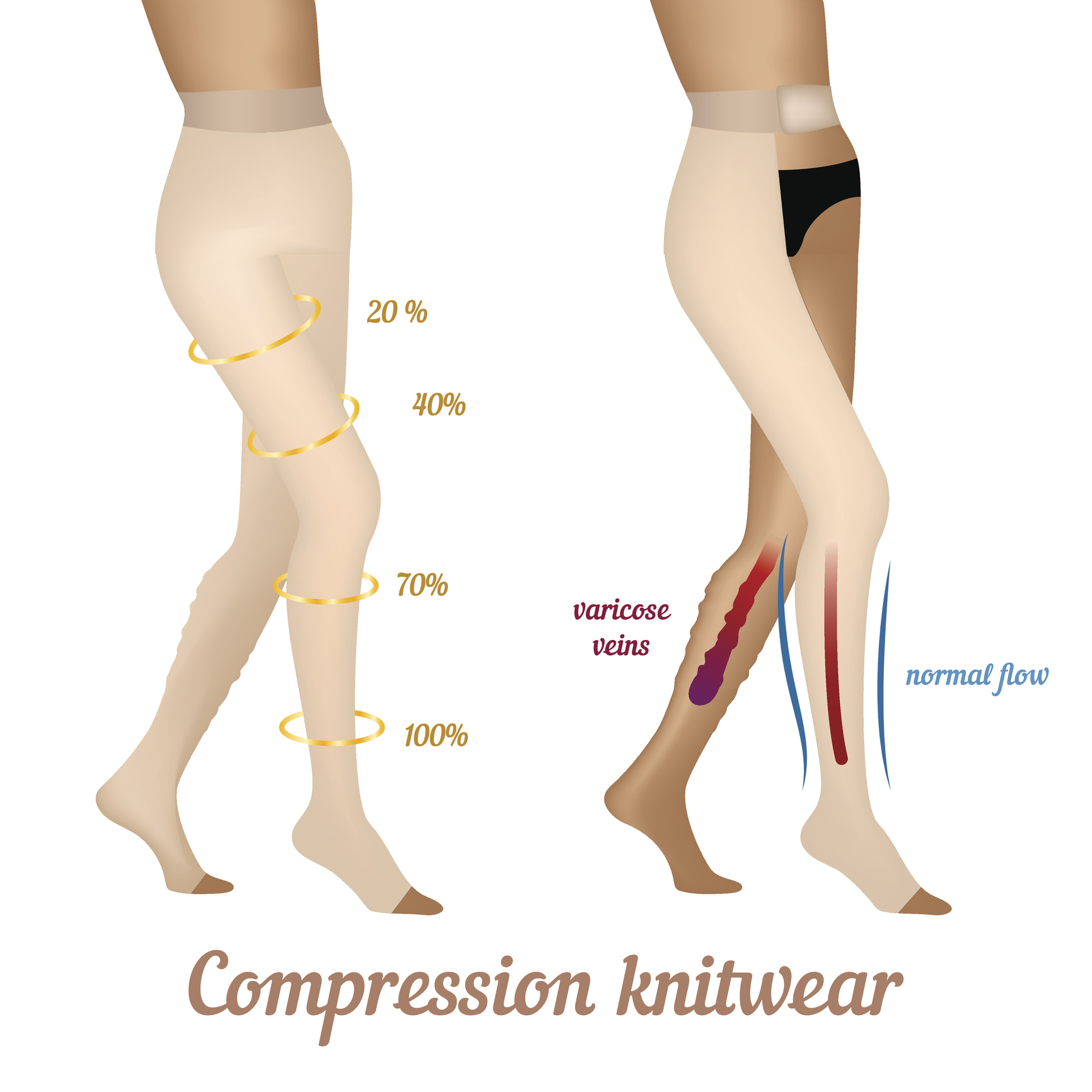
What kind of compression stockings are we familiar with?
- Calf
- thigh
- semi-femoral
- tights
Why is compression therapy used in practice?
- Replaces insufficiency of the calf muscle pump
- reduces congestion in the superficial venous system of the limbs
- accelerates blood flow
- alleviates the symptoms of disease by transporting metabolites
How should we apply the compression bandage correctly?
A short-drawn type of dressing, 8-10 cm wide, is best. Apply the dressing in a tight rotation. The pressure exerted by the dressing should be strongest at the ankle. It should ease towards the knee.
The bandage should be applied from the toes, upwards over the heel. Finally, a proper bandage should not hurt.
Surgical treatment
Surgical treatment of an ulcer includes skin graft transplantation, cleaning the base of the ulcer with a sharp spoon and other surgical methods.
Vascular surgery is one of the options. These treatments shorten the long-term course of the disease. These treatments include endoscopic subfascial resection of perforators or sclerotherapy.
Systemic treatment
Systemic treatment is aimed at the cause of the disease. It consists mainly in the treatment of circulatory and other associated diseases.
Systemic treatment includes veno-pharmaceuticals, vasodilators, analgesics and enzyme preparations. Systemic antibiotic treatment is indicated only when there are signs of skin infection.
One of the symptoms of a tibial ulcer is pain. Often patients complain that they cannot sleep because of the pain. Treatment of chronic pain improves quality of life. It also affects the rate of healing.
The intensity of pain is individual:
- it can be continuous
- aggravated by dressings
- can be triggered by a change in the position of the limb
Analgesics (painkillers) are chosen by the doctor according to the intensity of the pain, its nature (burning, deep, sharp, dull) and its duration (continuous, intermittent, during dressings).
If the patient has mild and moderate pain, non-steroidal antiphlogistic drugs are used. If the patient has moderate and severe pain, weak opioids (tramadol) are indicated. For patients suffering from severe pain, strong opioids (buprenorphine) are indicated.
Regimen measures
Regimen measures include exercise, nutrition and positioning of the limbs. Exercise helps to improve haemodynamics in the muscles. In this way, it helps in preventing recurrence of ulcers.
Patients should avoid prolonged standing and sitting, inappropriate footwear, wearing too tight clothing, exposure to high temperatures (sauna) and injuries to the feet.
In most cases, patients suffering from tibial ulcers are overweight. Nutritional deficiencies (deficiencies in vitamin A, C, protein and zinc) result in impaired ulcer healing.
Lack of exercise impairs the function of the muscle pump, thus leading to venous insufficiency.
Other auxiliary methods
We can support the healing of tibial ulcers (venous and lymphatic) with manual and instrumental lymphatic drainage. We can also use biostimulation laser, exercise and hyperbaric oxygen therapy.
Manual lymphatic drainage with a comprehensive approach by a physiotherapist significantly reduces leg swelling and associated pain. Lymphatic drainage enhances blood flow through the veins. This prevents the development of swelling.










