- solen.sk - Diagnostics of osteoporosis, Zdenko Killinger et al.
- solen.sk - Secondary osteoporosis, Soňa Tomková and Danica Telepková
- solen.sk - Osteoporosis and quality of life, Lucia Masaryková et al.
- solen.sk - Pharmacological treatment of osteoporosis, Daniel Čierny et al.
- casopisvnitrnilekarstvi.cz - Osteoporosis in premenopausal women, Juraj Payer et al.
- prolekare.cz - Influence of vitamin K on musculoskeletal health in postmenopausal women, Jan Rosa and Mária Stančíková.
- nia.nih.gov - Osteoporosis
- medicalnewstoday.com - What to know about osteoporosis, Brenda B. Spriggs
- accessmedicine.mhmedical.com - Osteopenia, Paul A. Fitzgerald
- ncbi.nlm.nih.gov - Osteopenia, Matthew Varacallo et al.
- pubmed.ncbi.nlm.nih.gov - Postmenopausal osteoporosis: the latest guidelines, Rod Marianne Arceo-Mendoza.
- josr-online.biomedcentral.com - The global prevalence of osteoporosis in the world: a comprehensive systematic review and meta-analysis, Nader Salari et al.
- science.org - Bone metabolism and evolutionary origin of osteocytes: Novel application of FIB-SEM tomography, Yara Haridy et al.
- ncbi.nlm.nih.gov - Osteoblast-Osteoclast communication and Bone Homeostasis, Jung-Min Kim et al.
- medicalnewstoday.com - Does caffeine contribute to osteoporosis?, Jessica Caporuscio
OSTEOPOROSIS: When bones weaken and treatment is difficult. What are the causes, symptoms and consequences + tips for prevention?

Osteoporosis causes weakening and fragility of the bones. It is a silent and gradually developing disease. Who is at risk? What are the symptoms and treatment?
Most common symptoms
- Malaise
- Chest pain
- Joint Pain
- Limb pain
- Nerve pain
- The Hump
- Bone Pain
- Muscle stiffness
- Pathological fracture
- Back Pain
- Bone thinning
- Fatigue
Characteristics
Osteoporosis is one of the most widespread disorders of the support system. It causes weakening and fragility of the bones to the extent that even normal movement or exertion can cause a fracture.
It is a silent and progressive disease that significantly reduces quality of life.
Because the treatment of osteoporosis is complex, it is important to be careful about prevention and early detection.
Who is at risk of osteoporosis, what are the symptoms and what (not) to do if you develop the disease?
The basic building blocks of bone are bone cells and an intercellular substance - bone matrix.
The bone matrix consists of a collagen network, non-collagenous proteins and mineral matter represented mainly by calcium. To a lesser extent, the mineral matter also consists of phosphorus and magnesium.
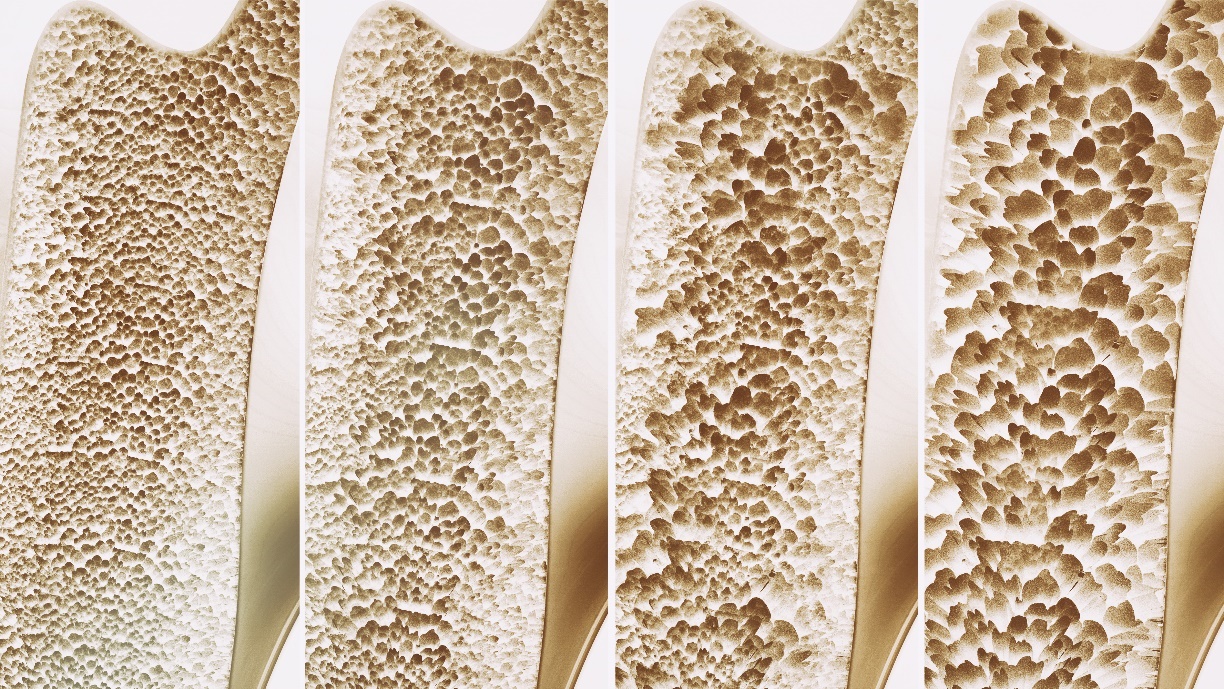
Osteoporosis is a disease characterised by significant loss of bone matrix, increased bone fragility and consequent high risk of fracture.
In 1830, the French pathologist Jean Lobstein discovered that every bone has pores. He also observed marked differences in the size of these pores, especially in older women. He called bones that had larger pores porous. He named the disease osteoporosis (osteo = bone, porosis = porous).
Does it really only affect women?
No.
Although osteoporosis is slightly more common in women, men are no exception.
A distinction can be made based on what caused the osteoporosis:
- Primary osteoporosis
- secondary osteoporosis
1. Primary osteoporosis
Primary osteoporosis is much more common than secondary osteoporosis. It is associated with changes in bone metabolism due to the natural ageing of the body.
We are familiar with primary osteoporosis:
- a type called postmenopausal, which occurs only in women after menopause
- the senile type, which can also affect men, most commonly after the age of 70
People who are short and thin are at higher risk of developing osteoporosis because they naturally have less bone mass. Bone loss can occur more rapidly as a result of ageing.
2. Secondary osteoporosis
Secondary osteoporosis is not related to natural ageing and can therefore occur in young people regardless of gender.
It is caused by various factors that indirectly (secondarily) affect bone metabolism.
The following table lists the main factors influencing the development of secondary osteoporosis
| Genetically determined factors | Mutations in genes for collagen, vitamin D, estrogen receptors, etc. |
| Environmental factors | Ionizing radiation, environmental influences |
| Long-term use of selected types of drugs | Corticosteroids, antacids (proton pump inhibitors), cytostatics, heparin, high-dose thyroid hormones, methotrexate, medroxyprogesterone acetate, thiazolidinediones, lithium, selective serotonin reuptake inhibitors (SSRIs), antiepileptics, etc. |
| Chronic diseases | Hypogonadism, hyperparathyroidism, hyperthyroidism, type I and II diabetes mellitus, hypercorticalism, acromegaly, hemochromatosis, rheumatic diseases, nephropathy, homocystinuria, chronic intestinal diseases (ulcerative colitis, Crohn's disease, celiac disease, lactose intolerance), hematopoietic disorders, cystic fibrosis, hepatic cirrhosis, chronic kidney disease, cancer, etc. |
| Prolonged excessive stress on the body | Peak sports, undue stress |
| Lifestyle, nutritional deficiencies | Alcohol, nicotine, excessive caffeine consumption, poor quality diet, eating disorders, sedentary lifestyle |
A less common type of osteoporosis is juvenile osteoporosis. It occurs in children and adolescents without a known causative factor. In young adults, so-called idiopathic osteoporosis is rare, and the causative factor is also unknown.
Causes
What is bone metabolism?
In addition to movement, bones have many other important functions in our bodies. They provide mechanical support for the body, protect vital organs and act as a reservoir of calcium and phosphate.
In order for bones to perform these functions throughout our lives, they must be able to adapt to changes in mechanical load and maintain their integrity and strength.
The constant metabolic activity of bone cells serves this purpose:
- Osteoblasts - Their main function is bone formation and mineralization.
- Osteoclasts - Their primary function is the destruction of bone by proteolytic enzymes.
Bone metabolism is the process of remodeling in which the old or damaged part of the bone is removed and replaced with new bone.
The entire bone remodeling cycle is stimulated primarily by physical activity.
It lasts approximately 4 months and has 4 phases:
- Activation phase - Immature osteoclasts come to the surface of the damaged bone.
- Destruction phase - Mature osteoclasts destroy (resorb) the damaged bone
- reversal phase - Osteoclasts die, immature osteoblasts move in to replace the damaged bone
- New bone formation phase - Mature osteoblasts produce new bone, and osteoblasts gradually mineralize and transform into new bone cells, which gradually transform into bone cells.
For the bone remodeling process to work properly, osteoblast-mediated bone formation must be in balance with osteoclast-mediated bone destruction.
This balance is strictly regulated by:
- parathyroid hormone
- calcitonin
- calcitriol
- estrogens
- growth hormone
- insulin
- glucocorticoids
- thyroid hormones
- inflammatory cytokines
- calcium levels
- vitamin K2 levels
- phosphorus levels
An imbalance in bone metabolism occurs when any of these regulators is deficient or in excess for various reasons.
The table shows the influence of the basic regulators of bone metabolism on the activity of bone cells
| Regulator | Osteoclast activity | Osteoblast activity |
Parathyroid hormone
| ↑ | ↓ |
Calcitriol (1,25-dihydroxycholecalciferol)
| ↑ | ↓ |
Calcitonin
| ↓ | no effect |
Tyronines (thyrotropic hormone, thyroxine and triiodothyronine)
| ↑ | ↓ |
Estrogens (estradiol, estrone and estriol)
| ↓ | ↑ |
Growth hormone (somatotropin)
| without influence | ↑ |
Insulin
| without effect | ↑ |
Glucocorticoids (cortisol, cortisone)
| ↑ | ↓ |
Inflammatory cytokines (IL-1, IL-2, IL-6, IL-12, TNF-αand others).
| ↑ | ↓ |
How are calcium, vitamin D and vitamin K2 related?
Bones are the largest reservoir of calcium in the body. Calcium is found in them in the form of hydroxyapatite, calcium hydrogen phosphate and calcium carbonate.
In order for calcium from the diet to reach the bones, the presence of:
- the active form of vitamin D (calcitriol)
- vitamin K2
- osteocalcin
- the other regulators of bone metabolism mentioned above, in particular parathyroid hormone and calcitonin
Calcitriol is formed in the kidneys from vitamin D3 (cholecalciferol) by the action of parathyroid hormone.
Calcitriol has several indispensable roles in the body, one of which is to increase calcium absorption from the intestines and reduce its excretion in the urine.
After calcium is absorbed by intestinal cells (enterocytes), the role of vitamin K2 comes into play.
Vitamin K2 is part of an enzyme in our body called gammaglutamyl carboxylase. This allows it to ensure that osteocalcin is activated by a process called carboxylation.
This carboxylated osteocalcin then works with calcitonin to help build calcium directly into the bones.
This means that calcium taken into the body will not be deposited where it shouldn't (e.g. in the walls of blood vessels). It will be used as efficiently as possible to build bone mass.
Osteocalcin is a protein produced by mature osteoblasts, which is part of the bone matrix. Osteocalcin formation is promoted by calcitriol. According to recent findings, vitamin A also promotes osteocalcin formation.
For more information on vitamin A and its effect on bone, see here:
VITAMINA for good eyesight? Where is it needed?
Symptoms
Does osteoporosis hurt?
Not at first.
In the initial stages of the disease, no symptoms appear.
Later on, non-specific back pain may occur, which worsens with movement, e.g. back pain when changing body position from lying to sitting.
There may also be bone pain that has no obvious cause, e.g. unrelated to a previous bone injury.
Very often the very first sign of osteoporosis is a fracture when the disease is already fully developed.
Fractures of bones affected by osteoporosis occur even with very little pressure and in situations where a healthy bone would not break.
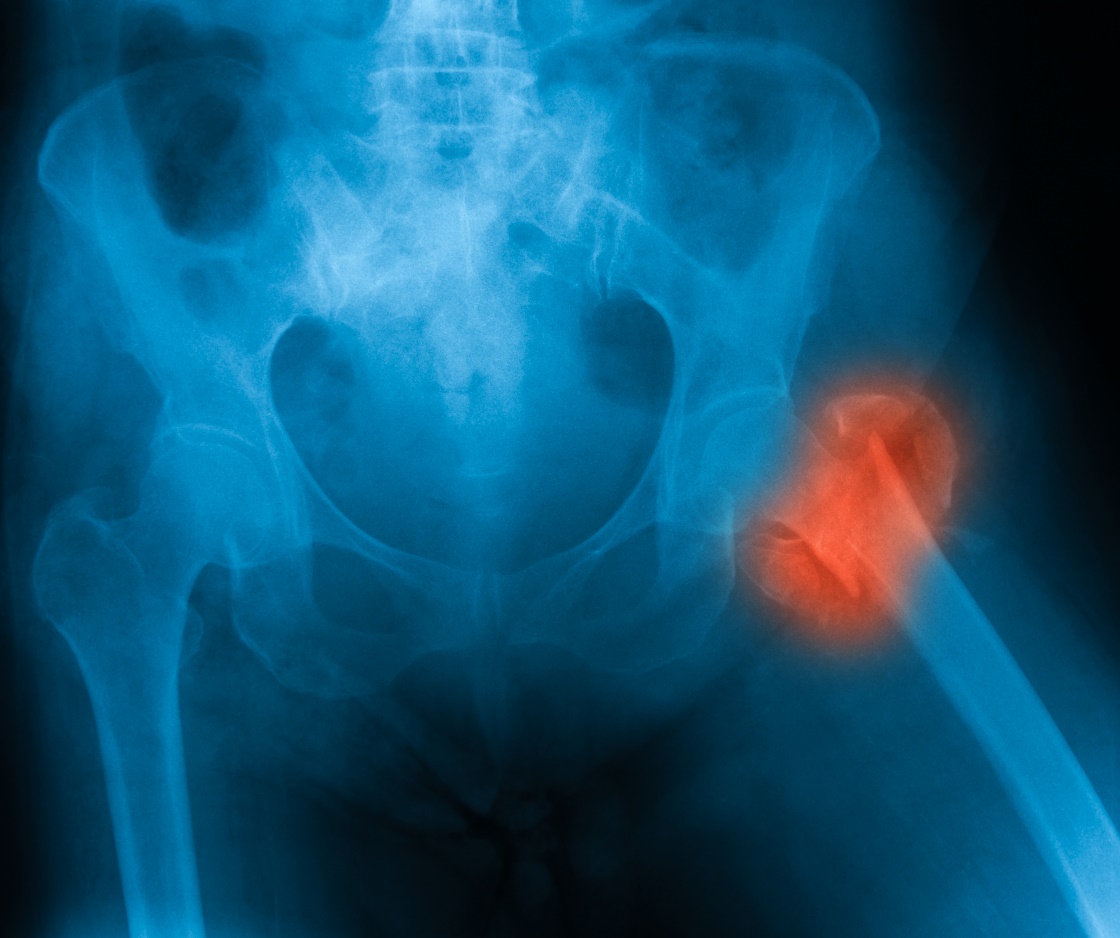
The most common fracture sites are the forearm, vertebrae and femur.
Other symptoms of osteoporosis that have already developed include:
- loss of body height
- hunched posture
- general physical weakness
Diagnostics
- visual examination, during which the patient's physical parameters are evaluated
- measurement of bone mineral density - densitometry
- laboratory blood tests
- conventional radiological examination (e.g. X-rays of the vertebrae)
What is densitometry?
Densitometry is a painless test that determines bone mineral density, called bone mineral density (BMD).

It is performed in a radiology outpatient clinic. Currently, any doctor can send a referral for this test.
You must meet at least one of the indication criteria, which include:
- Long-term estrogen deficiency
- long-term treatment with corticosteroids, anticoagulants, antiepileptics, immunosuppressants, cytostatics, thyroid hormones or other drugs affecting bone metabolism
- BMI < 19
- Women over 65 years and men over 70 years
- parental history of femoral neck fracture
- presence of other chronic diseases affecting the development of osteoporosis
- suspicion of osteoporosis from vertebral radiographs
- fractures due to inadequate trauma and other symptoms characteristic of osteoporosis
The principle of densitometry is the measurement of X-ray absorption by bone tissue.
The result is a bone density value expressed in grams of mineral matter per cm2 of bone (g/cm2). Using densitometry, the doctor determines the amount of calcium present in a particular bone.
In densitometry, only those bones that are most likely to fracture are irradiated with X-rays. The most commonly used method in densitometry is dual energy X-ray absorptiometry (DXA).
The most accurate view of bone density is provided by central densitometry, which examines the femoral spine and the upper part of the femur (proximal femur).
Densitometry results - how to understand them?
The bone density value obtained from the densitometric examination must be converted to a T-score or Z-score before a diagnosis can be made.
The T-score represents the difference between the patient's bone density value and the average bone density value measured in healthy young individuals of the same sex.
The table shows the degree of osteoporosis defined by the T-score.
| Degree of osteoporosis | T-score |
| 1. Incipient osteoporosis (osteopenia) | -1 to -2.5 SD |
| 2. Osteoporosis | less than -2,5 SD |
| 3. Manifest osteoporosis | less than -2,5 SD + at least 1 inadequate fracture |
If the T-score decreases by even 1 unit, the risk of fracture increases up to twofold.
The T-score is determined in all patients with suspected primary osteoporosis, i.e. in persons over 65 years of age and in postmenopausal women regardless of age.
The Z-score is a comparison of the patient's T-score and the average T-score of healthy persons of the same sex and age.
A Z-score of less than -2 is considered a warning sign of reduced bone density.
The Z-score is determined especially in children and young patients with suspected secondary osteoporosis.
If osteopenia results in...
A T-score between -1 and -2.5 or a Z-score below -2 represents reduced bone density. It is referred to as osteopenia.
Osteopenia does not yet lead to inadequate fractures or other problems that occur in full-blown osteoporosis. Therefore, osteopenia is considered a precursor to osteoporosis or incipient osteoporosis that does not yet have any symptoms.
If you have been diagnosed with osteopenia, you will need to have regular densitometric check-ups. At the same time, you will need to take appropriate preventive measures. Prevention can often prevent osteopenia from developing into osteoporosis.
Trabecular bone score (TBS)
The DXA method used in densitometric examination can also be used to calculate the so-called trabecular bone score, which assesses the quality of bone mass independently of bone density.
It focuses on the microarchitecture of the bone, i.e. the distribution of minerals in specific sections of the bone, most commonly in the lumbar spine.
Based on the TBS value, the risk of fracture can be determined. A TBS value below 1.32 defines reduced bone quality and deterioration of bone microarchitecture.
FRAX Fracture Risk Calculator
FRAX (Fracture Risk Assessment Tool) is a computerised calculator developed by WHO. It assesses the 10-year risk of fracture in a patient with suspected osteoporosis.
It is a questionnaire in which the patient answers 11 basic diagnostic questions about risk factors for osteoporosis. If the patient has densitometric results, there are 12 questions.
The patient can complete this questionnaire free of charge via the sheffield.ac.uk website. However, it is up to the doctor to interpret the results.
Laboratory blood tests
Osteoporosis is characterised by loss of bone matrix caused by an imbalance in bone metabolism. It is therefore possible to assess various biochemical parameters in the blood to reflect any changes in the metabolic activity of bone cells.
Blood tests can also help to exclude other diseases that might be responsible for the development of secondary osteoporosis.
At the time of diagnosis, the markers listed in the table below are the main ones to be determined in a patient with suspected osteoporosis. The reference values given are for people over 50 years of age.
The markers listed in the table
| Marker | Abbreviation | Sample material | Reference values |
| Blood count | KO | whole blood | Miscellaneous |
| Glucose | GLU | whole blood | 3.3-5.5 mmol/l |
| Creatinine | KREA | Serum | Men: 60-100 µmol/l Women: 50-90 µmol/l |
| Albumin | ALB | Serum, plasma | 36-45 g/l |
| Alkaline phosphatase | ALP | Serum, plasma | Men: 0.88-2.13 μkat/l Women: 0,88-2,35 μkat/l |
| Alanine aminotransferase | ALT | serum, plasma | Men: 0.23-0.68 Women: 0.12-0.52 |
| Gammaglutamyltransferase | GMT, GGT | Serum, plasma | Men: 0.25-1.90 μkat/l Women: 0.18-1.28 μkat/l |
| C-reactive protein | CRP | Serum, plasma | < 5 mg/l |
| Rheumatoid factor | RF | serum, plasma | < 30 kIU/ml |
| Antistreptolysin O | ASLO | serum | < 200 IU/ml |
| Glomerular filtration rate | GF | Serum | > 1.5 ml/s/1.73m2 |
| Protein electrophoresis | ELFO | serum | various |
| C-terminal telopeptide fragment of collagen 1 | CTx-1 | Serum | Men: 204.0-504.0 ng/l Women: 330.0-782.0 ng/l |
| Osteocalcin | OC | Serum | Men: 14.0-46.0 µg/l Women: 13.0-43.0 µg/l |
| Propeptides of procollagen 1 | P1NP | Serum | 25.9-43.0 µg/l |
| Bone alkaline phosphatase fractions | bALP | Serum | Men: 23.0-75.0 % Women: 20,0-74,0 %. |
| Vitamin D (total) | D | Serum, plasma | 60.0-200.0 nmol/l |
| Calcium | Ca | serum | 2.15-2.51 mmol/l |
| Phosphorus | P | serum, plasma | Men: 0.75-1.35 mmol/l Women: 0.85-1.50 mmol/l |
| Parathyroid hormone | PTH | Serum | 15.0-65.0 ng/l |
| Prolactin | PRL | Serum | Men: 2.1-17.7 µg/l Women: 2.0-29.2 µg/l |
| Thyrotropic hormone | TSH | Serum | 0.50-5.40 µIU/ml |
| Free thyroxine | fT4 | Serum | 11.6-22.7 pmol/l |
| Estradiol (in women) | E2 | Serum | Miscellaneous |
World Osteoporosis Day falls on 20 October. During this day, many health care facilities and organisations provide free lectures or screenings aimed at the prevention and early detection of osteoporosis.
Consequences, prognosis
The most serious consequence of osteoporosis is painful fractures. In terms of prognosis, fractures of the femoral neck are the most dangerous.
After a femoral neck fracture, approximately 20% of patients die within one year due to complications.
Other consequences of osteoporosis include chronic musculoskeletal pain and the associated inability to carry out some normal activities. This can lead to social withdrawal and psychological difficulties.
It is estimated that approximately one in three women and one in five men over the age of 50 will suffer a fracture as a result of osteoporosis. Due to environmental and nutritional factors (e.g. lack of sunlight, vitamins, etc.), the risk of these fractures in Europe is highest in the Scandinavian countries.
Prevention
What you eat when you're young is waiting for you when you're old...
For any disease, the basis of prevention is lifestyle, which includes a healthy diet and exercise.
In terms of osteoporosis, it is very important not to neglect building bone mass from a young age.
During adolescence, the formation of new bone outweighs the destruction of bone. This leads to growth. Around the age of 25, we reach what is known as peak bone mass. This means that at this age our bones are at their best. Around the age of 35, bone mass begins to naturally decline. The percentage of bone loss can vary from one healthy individual to another, depending on genetics, lifestyle or the quality of bone mass built up at a young age.
What is good for building bone mass?
First and foremost, a varied and high quality diet that ensures adequate intake of calcium, magnesium, B vitamins and vitamin K2 from natural sources.
It is also necessary to ensure a sufficient intake of vitamin D, which often needs to be supported by appropriate dietary supplements. When taking them, it is necessary to follow the recommendations of the doctor or pharmacist.
Read also:
Bone density: what are healthy values when tested and how to increase them?
Regular exercise is also important for building bone mass. The intensity of exercise should be adapted to age and current physical condition. In particular, strength sports such as weight training are the most effective.

What to watch out for?
In order to keep bone mass in the best possible condition, the following activities in particular must be avoided:
- sedentary lifestyle
- excessive sugar consumption, which reduces calcium absorption
- excessive consumption of animal protein, red meat and sausages, the metabolism of which increases the release of calcium from the bones
- excessive salt consumption, which increases calcium excretion
- alcohol, which reduces calcium absorption
- smoking, as nicotine negatively affects parathyroid hormone production and the balance of bone cell activity through various mechanisms
Coffee and osteoporosis - how is it really?
Not only coffee, but also other popular caffeinated beverages have been blacklisted for many years in terms of their impact on bone health.
The adverse effect of caffeine on bone metabolism is mainly related to its diuretic effect, but also to its effect on vitamin D receptors.
Increased diuresis (urine output) after consuming a caffeinated beverage increases urinary calcium excretion. The effect on vitamin D receptors in turn has a negative impact on calcium absorption.
This can be particularly problematic in people who consume high doses of caffeine and who do not replace calcium losses with diet, i.e. do not have a balanced diet.
Therefore, the consumption of high doses of caffeine is not recommended for the prevention and treatment of osteoporosis.
However, drinking coffee in reasonable quantities (e.g. 2 cups per day containing 8 g of coffee) does not have a significant effect on osteoporosis.
How it is treated: Osteoporosis
Osteoporosis treatment: drugs, vitamins and minerals. What else will help?
Show moreOsteoporosis is treated by
Other names
Interesting resources










