- Fasano A (April 2005). "Clinical presentation of celiac disease in the pediatric population". Gastroenterology (Review). 128 (4 Suppl 1): S68–73.
- "Symptoms & Causes of Celiac Disease | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases.
- Lebwohl B, Ludvigsson JF, Green PH (October 2015). "Celiac disease and non-celiac gluten sensitivity". BMJ (Review). 351: h4347.
- Lundin KE, Wijmenga C (September 2015). "Coeliac disease and autoimmune disease-genetic overlap and screening". Nature Reviews. Gastroenterology & Hepatology (Review). 12 (9): 507–15.
- "Celiac disease". World Gastroenterology Organisation Global Guidelines.
- Ciccocioppo R, Kruzliak P, Cangemi GC, Pohanka M, Betti E, Lauret E, Rodrigo L (22 October 2015). "The Spectrum of Differences between Childhood and Adulthood Celiac Disease". Nutrients (Review). 7 (10): 8733–51.
- Lionetti E, Francavilla R, Pavone P, Pavone L, Francavilla T, Pulvirenti A, Giugno R, Ruggieri M (August 2010). "The neurology of coeliac disease in childhood: what is the evidence? A systematic review and meta-analysis". Developmental Medicine and Child Neurology. 52 (8): 700–7.
- Husby S, Koletzko S, Korponay-Szabó IR, Mearin ML, Phillips A, Shamir R, Troncone R, Giersiepen K, Branski D, Catassi C, Lelgeman M, Mäki M, Ribes-Koninckx C, Ventura A, Zimmer KP, ESPGHAN Working Group on Coeliac Disease Diagnosis; ESPGHAN Gastroenterology Committee; European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (January 2012). "European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease" (PDF). J Pediatr Gastroenterol Nutr (Practice Guideline). 54 (1): 136–60.
- Tovoli F, Masi C, Guidetti E, Negrini G, Paterini P, Bolondi L (March 2015). "Clinical and diagnostic aspects of gluten related disorders". World Journal of Clinical Cases (Review). 3 (3): 275–84.
- Lindfors, Katri; Ciacci, Carolina; Kurppa, Kalle; Lundin, Knut E. A.; Makharia, Govind K.; Mearin, M. Luisa; Murray, Joseph A.; Verdu, Elena F.; Kaukinen, Katri (December 2019). "Coeliac disease". Nature Reviews Disease Primers. 5 (1): 3.
- Vivas S, Vaquero L, Rodríguez-Martín L, Caminero A (November 2015). "Age-related differences in celiac disease: Specific characteristics of adult presentation". World Journal of Gastrointestinal Pharmacology and Therapeutics (Review). 6 (4): 207–12.
- Ferri, Fred F. (2010). Ferri's differential diagnosis : a practical guide to the differential diagnosis of symptoms, signs, and clinical disorders (2nd ed.). Philadelphia, PA: Elsevier/Mosby. p. Chapter C. ISBN 978-0323076999.
- ee JA, Kaukinen K, Makharia GK, Gibson PR, Murray JA (October 2015). "Practical insights into gluten-free diets". Nature Reviews. Gastroenterology & Hepatology (Review). 12 (10): 580–91. d
- Fasano A, Catassi C (December 2012). "Clinical practice. Celiac disease". The New England Journal of Medicine (Review). 367 (25): 2419–26.
- Newnham, Evan D (2017). "Coeliac disease in the 21st century: Paradigm shifts in the modern age". Journal of Gastroenterology and Hepatology. 32: 82–85.
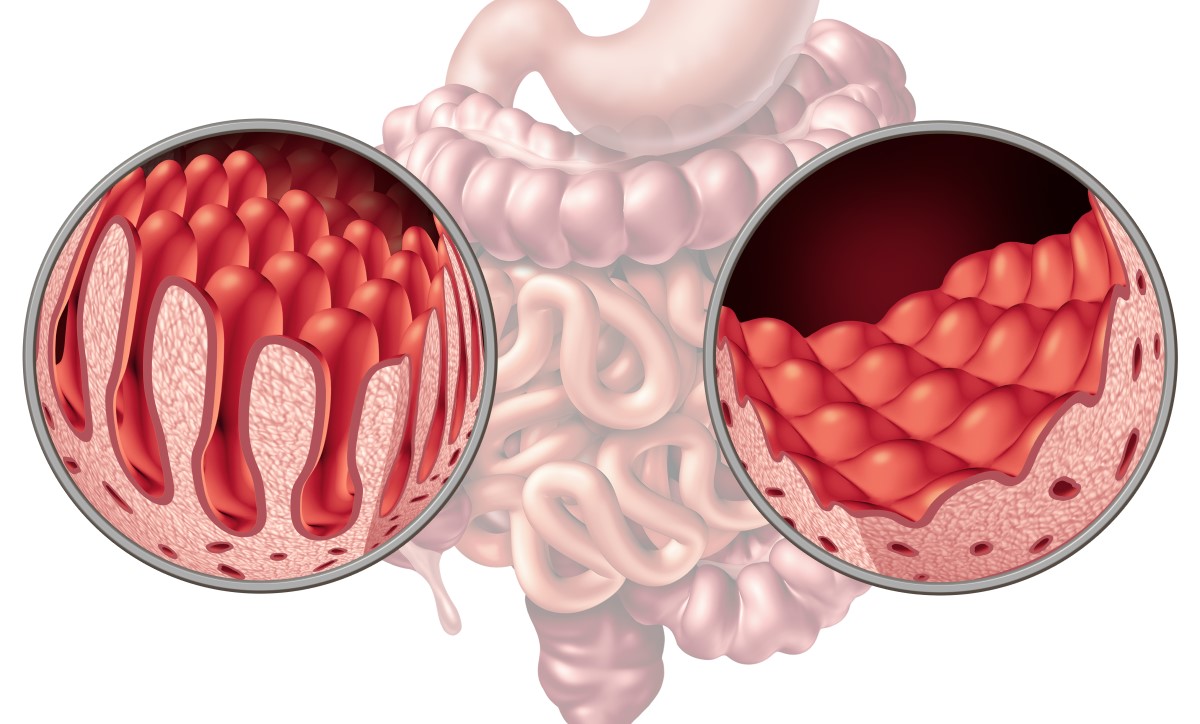
Celiac Disease: Identification, Causes, Symptoms, Treatment

Photo source: Getty images
Most common symptoms
- Aphthae
- Malaise
- Right Flank Pain
- Stomach pain after a meal
- Abdominal Pain
- Joint Pain
- Limb pain
- Anal pain
- Belly button pain
- Lower Abdominal Pain
- Tooth pain
- Spirituality
- Constipation
- Diarrhoea
- Bone Pain
- Rash
- Teeth wiggling
- Brittle nails - onychoschizia
- Brittle hair
- Flatulence - bloating
- Excessive Hair Loss: Causes, Treatment
- Bloating - flatulence
- Indigestion
- Swelling of the limbs
- Tremor
- Dry skin
- Muscle weakness
- Fatigue
- Vomiting after eating and nausea
- Reddened skin
- Yellowish skin
Show more symptoms ᐯ
Treatment, medication, a gluten-free diet
Show moreCeliac Disease is treated by
Other names
Celiac sprue, nontropical sprue, endemic sprue, gluten enteropathy