- healthline.com - What Is Oophoritis and How Is It Treated?
- sciencedirect.com - Ovary Inflammation
- mayoclinic.org - Pelvic inflammatory disease
Inflammation of the ovary is a gynecological infection that often occurs simultaneously with inflammation of the fallopian tube, either by extension of the inflammation taking place in the vagina and uterus, or by inflammation of the surrounding organs. Most ovarian infections are caused by bacterial infection. Bacteria enter the ovary through the vagina or through the bloodstream.
Inflammation of the ovaries, also called oophoritis, is a rather serious infectious disease.
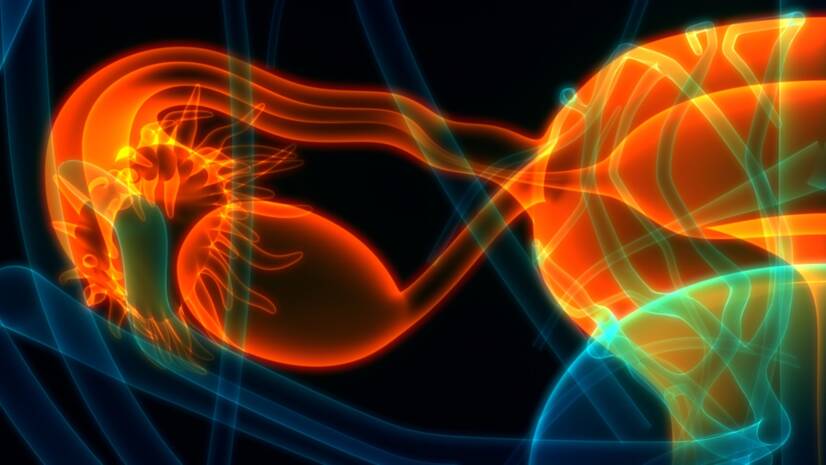
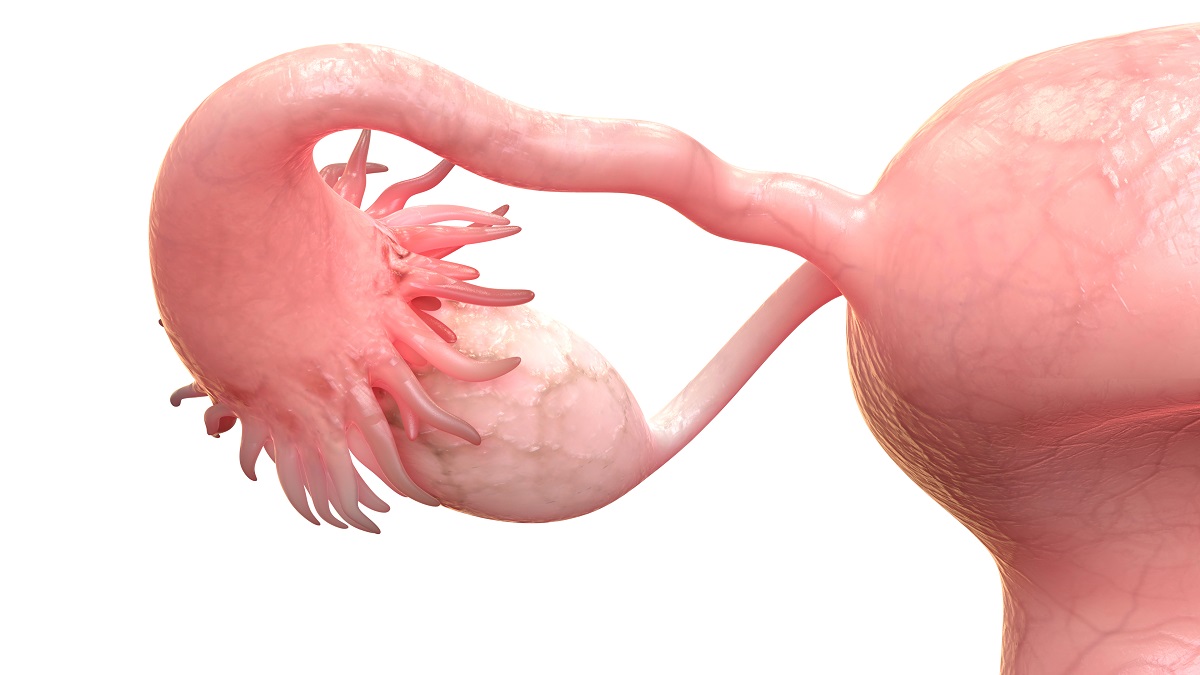
In some cases, the inflammation affects only the ovary, but in most cases, concurrent with the inflammation of the ovary, there is also inflammation of the fallopian tube called Salpingo-oophoritis, or as adnexitis, which is one of the common inflammatory diseases of the female genital organs.
Adnexitis means inflammation of the uterine adnexa, i.e. the uterine appendages that make up the fallopian tube and the ovary.
The ovaries are the paired internal sex organs of a woman that produce the female sex cells eggs and the sex hormone estrogen.
The fallopian tube is a paired organ connecting the uterus to the ovaries. They are tube-shaped, arising from the corners of the uterus and terminating in a funnel-shaped flared end encircling the ovary.
Inflammation of the ovaries is not infrequently accompanied by inflammation in the ovarian region, the entire pelvic area, i.e. also inflammation of the lining of the uterus and surrounding tissues.
It is often caused by a bacterial infection, or a consequence of chronic pelvic inflammatory disease.
The risk of ovarian inflammation increases in the early stages of sexual life, which also depends on sex life and intimate hygiene.
Women of childbearing age between the ages of 20 and 30 are most commonly affected.
Pubertal girls or postmenopausal women are rarely affected.
In most cases, the infection spreads from the cervix to the uterus, then to the fallopian tubes and finally to the ovaries. Eventually, if there are complications, the inflammation can also spread to the peritoneum and abdominal wall. This inflammation cannot arise from a cold, but a cold significantly contributes to the development of the infection.
The disease is caused by bacteria, rarely also by viruses.
The infection enters the ovary and fallopian tubes through different routes called ascending and descending routes.
The ascending route means if the infection is coming from the bottom to the top, i.e. from the vagina, the uterus to the ovary.
The causative agent of inflammation can be present in the vagina and when it overgrows and crosses the barrier, it causes inflammation. The most common transmission of infection is sexual intercourse.
Inflammation can also spread after childbirth, after miscarriage, after menstrual bleeding, or after cervical surgery. However, childbirth, miscarriage, intrauterine device insertion are among the less common reasons for ovarian inflammation.
The descending route means if the inflammation comes from distant foci via the blood or lymphatic route.
For example, from the gastrointestinal tract, from the intestinal tract, most often transferred from the inflammation of the appendix, by infiltration of the effusion formed after its inflammation.
Blood-borne inflammation can develop with an ongoing infection in the body, often with chronic tonsillitis and in immunocompromised women.
Infection-induced inflammation of the ovaries is distinguished from autoimmune oophoritis, which is caused by a malfunction of the immune system.
The immune system attacks the ovaries, treating them as a foreign body, causing inflammation, even atrophy (a decrease in function and its shrinkage).
These inflammatory changes on the ovary damage its function. The main symptoms are irregular to absent menstruation, abdominal cramps, bloating, nausea.
Autoimmune oophoritis can be part of an autoimmune syndrome.
Common causative agents of ovarian inflammation:
Risk factors:
The common cold does not result inovarian inflammation - it is only a risk factor.
Women with weakened immunity are at increased risk.
Typical for inflammation of the ovary is pain in the lower abdomen.
In the early stages of inflammation, the pain may be milder and more of a twinge, but later it turns into a constant pain of a more intense nature, depending on how quickly the inflammation grows.
Most commonly, the pain appears on the right side, or all over the lower abdomen. Very rarely, it can appear on the left side.

Adolescent girls often have recurrent lower abdominal pain, which they notice when they change position or have shocks. The pain shoots into the sacrum, thighs, or the labia majora (i.e. outer lips).
Pain in the lower abdomen has an escalating character. The pain increases and may present with cramps in the lower abdomen.
Elevated body temperature that occurs irregularly and can last up to a week.
High body temperature is less common in young women with ovarian inflammation.
Discharge from the genitals is not the rule and occurs in less than half of women. The discharge may be foul-smelling, greenish, or yellowish in colour.
Menstruation (i.e. period) tends to be more painful even in women who have not previously suffered any pain during menstruation.
Bleeding outside the menstrual cycle may also occur.
Pain during sexual intercourse.
Accelerated pulse.
Severe pain during ovulation.
Fever in severe inflammation is often accompanied by fatigue, chills and lack of appetite.
There may also be a burning sensation or pain during urination.
Frequent urge to urinate.
Diarrhea or constipation.
Ongoing inflammation can lead to tubal ligation leading to infertility. In cases of partial adhesion there is a high risk of ectopic pregnancy.
In some cases, there may be no symptoms, and the diagnosed inflammation of the ovary remains only after a sudden attack of pelvic pain.
Sometimes the symptoms are mild, when they are hardly recognizable.
Inflammation of the ovary is diagnosed by a gynecologist on the basis of a comprehensive examination.
Palpation through the vagina and abdominal cavity may not confirm inflammation, because in the early stages of inflammation, tenderness to palpation is not pronounced.
During inflammation, the ovaries are sensitive, even painful. Later, swelling develops in the fallopian tube, ovary or uterus, which may be markedly swollen and painful on touch.
Blood and urine tests, where the focus is on the number of white blood cells, which are elevated when there is an inflammatory process in the body, as well as CRP values.
To identify the causative agent of the infection, a cervical smear is taken from the cervix, examined and sent to a laboratory for culture.
Cultures taken from the vagina and cervix tend to be 50-70% identical to cultures taken from the ovaries.
Ultrasound of the small pelvis, will show inflammatory changes, swelling of the ovary and fallopian tube.
Another method that belongs to the invasive methods is endoscopic examination, laparoscopy, which makes it possible to take material for examination during the examination and can reveal the cause of pain in the pelvis. This examination is approached in adult women rather than in adolescents and children.
Inflammation of the ovary and fallopian tubes are often affected at the same time.
Inflammation affecting only the ovary occurs in appendicitis or after transmission of inflammation by blood or lymphatics.
More common, however, is the transmission of inflammation from the vagina, uterus, through the fallopian tube to the ovary.
According to the duration of ongoing inflammation and its nature, ovarian inflammation can be acute or chronic.
Acute inflammation is sudden, accompanied by pain in the lower abdomen. In adolescent girls, inflammation does not have as strong a course as in adult women. Typical is swelling of the fallopian tube and marked pain of the ovary on examination by touch.
Chronic inflammation is less pronounced and is usually accompanied by disturbed menstruation, pain during sexual intercourse.
Inflammation from the ovaries can also spread to the surrounding area, up to the peritoneum. With purulent inflammation, an abscess may form, or pus may accumulate in the Douglas space.
Purulent inflammation can cause gradual narrowing of the fallopian tube until it is completely closed.
If the inflammation is left untreated, damage to the ovary can occur, resulting in absence of menstruation, i.e. amenorrhoea.
The passage of inflammation to the peritoneum can lead to intestinal obstruction, called ileus, which requires surgery.
Untreated and progressive inflammation of the ovary can lead to an inflammatory adnexum (an unspecified tumor of the fallopian tube, ovary), or a tubo-ovarian abscess, a pus-filled cavity in the ovarian area. If the abscess ruptures, sepsis, popularly known as blood poisoning, can develop, which is life-threatening.
With inflammation of the ovary, adhesions, abscesses, accumulation of pus in the ovary or in the fallopian tube can occur.
A dangerous consequence of inflammation can be sterility, i.e. infertility.
With ongoing inflammation, the inflammation can spread to the surrounding area and affect surrounding organs, causing further complications.
Learn more:
Ovarian cysts: The dangers of rupture and pregnancy
Ovarian cancer: Causes, identification, and treatment
Ovarian inflammation if not caught and treated in time can affect fertility.
The scarring of the tissue and fusion leads to a blockage of the fallopian tube occurs.
In case of partial fusion or scarring of the fallopian tube, there is an increased risk of ectopic pregnancy.
Sometimes it is possible to remove the blockages surgically, which will help to achieve normal fertilization. If these blockages cannot be removed, in vitro fertilization (IVF), an artificial insemination where the glued fallopian tubes are bypassed, is recommended.
In the case of damage to both ovaries, only egg donation and IVF remain options for pregnancy and foetal delivery.
During pregnancy and confirmation of inflammation, it is necessary to treat the inflammation. Antibiotics are given, which are gentle and do not endanger the fetus, but the treatment itself can be longer and more complicated than in the non-pregnancy period.
Treatment of ovarian inflammation: what to do for pain? Medications and antibiotics?
Show more


