- clevelandclinic.org - Female Infertility
- womenshealth.gov - Infertility
- webmd.com - Your Guide to Female Infertility
- mayoclinic.org - Female infertility
Female Infertility: Causes, Diagnosis

Female infertility means that it is not possible for a woman to become pregnant.
Most common symptoms
- Period pain
- Lower Abdominal Pain
- Depression - depressed mood
- Bleeding after sexual intercourse
- Malnutrition
- Menstrual cycle disorders
- Mood disorders
- Smelly discharge from the vagina
- Long menstrual bleeding
Characteristics
Female infertility is a disease in which a woman is unable to conceive and successfully bear a child.
Approximately 10% of women suffer from some form of infertility.
Infertility affects 60-80 million people worldwide, and half of them remain childless their entire lives.
Worldwide, 35% of cases are male, 50% are female, 5% involve couple compatibility, and 10% are of unknown origin.
Infertility is a topic that concerns more than one couple longing for a child. This topic brings with it a lot of negative emotions affecting the psyche and health of the individual. Recently, infertility has been on the rise. Infertility is considered to be a condition where conception has not occurred even after a year of unprotected sexual intercourse.
Infertility in women is multifactorial, with the first problems of declining fertility usually occurring over the age of 35. After the age of 40, fertility already decreases quite significantly.
Infertility can take several forms.
Primary infertility is characterised by the condition of failing to conceive a child even after a year if the couple has had unprotected intercourse at least twice a week.
Secondary infertility is the same condition, but the couple has already conceived a child in the past.
Fertilisation takes place properly if the reproductive system is functioning properly.
How does fertilization occur?
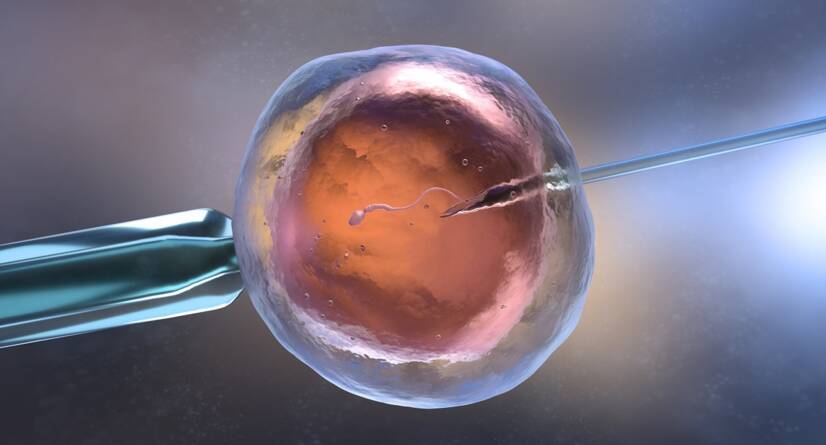
- Fertilisation occurs during sexual intercourse, by the fusion of male and female sex cells.
- A healthy ovary releases a mature egg during ovulation.
- The released ovum is drawn through a funnel-shaped opening into the fallopian tube.
- Sperm pass through the lining of the uterus into the ovary, where they meet the egg waiting to be fertilised.
- After fertilization, the egg travels further through the fallopian tube into the uterus.
- The fertilized egg attaches to the lining of the uterus, where it implants and grows.
You can read more in the article:
How does fertilization of the egg occur and how long does it take to nest?Fertility depends on the regular formation of a mature egg, on its journey from the ovary to the uterus and on the readiness of the lining of the uterus.
Infertility is defined as a couple who have not conceived an offspring by unprotected sexual intercourse within one year, or women above 35 or more after 6 months.
Infertility represents a great psychological burden and is one of life's most painful experiences.

Many women experience infertility full of sadness and depression, and see motherhood as the goal of their lives. For men, infertility is more associated with feelings of disappointment. It is a stressful situation for both partners.
The discovery of infertility brings with it feelings of guilt, self-blame for past sexual behaviours such as abortion and venereal disease. After repeated and unsuccessful treatment, there is often denial, anger, depression. Later, couples begin to think about alternatives, such as artificial insemination, adoption, or living a life without a child.
Causes
There are many causes of female infertility. Sometimes it is difficult to pinpoint the exact cause and some couples even have unexplained infertility.
Common causes of infertility include:
- Ovulation disorders – 25 %
- Endometriosis - 15%
- Pelvic adhesions – 12 %
- Blockage of the fallopian tubes – 11 %
- Other fallopian tube/uterine abnormalities – 11 %
- Hyperprolactinemia - 7%
Ovulation disorder
An ovulation problem occurs when an egg is not released from the ovary.
It occurs with hormonal imbalance, after an eating disorder, substance abuse, thyroid disease, stress, or pituitary tumors.
Normal ovulation depends on the precise timing and interaction of the hypothalamus, pituitary and ovary. If the hypothalamus or pituitary gland does not stimulate the ovary sufficiently, the release of the egg will not occur.
With a violated ovary, the stimulation of hormones may be correct, but the ovary does not respond. The normal course of ovulation is prevented by chemotherapy, alcoholism and smoking. Sometimes the problem is the premature onset of menopause.
There may also be a problem with the number and quality of eggs.
Women are already born with all the eggs that have developed while still in intrauterine development. Some women's egg supply becomes depleted, which often occurs before menopause.
Affected eggs have the wrong number of chromosomes, such eggs are not able to fertilise or there is no possibility for them to develop into a healthy foetus. Such affected eggs tend to be accidental, but are more common as a woman ages.
Polycystic ovary syndrome -PCOS.
It causes hormonal imbalances. It is often associated with obesity, abnormal facial hair, acne, and is one of the common causes of female infertility.
Primary ovarian insufficiency is usually due to premature loss of eggs, or an autoimmune response due to genetics, but also after overcoming cancer with subsequent chemotherapy.
Problems with the uterus
This group includes the occurrence of polyps (growths on the lining of the uterus), myoma (benign tumors), adhesions located inside the uterus, cysts, which are common in the uterus, these pathologies by their growth can block the fallopian tubes or cause disorders of implantation of the fertilized egg.
A uterine disorder can be congenital (inborn) such as a septum, where there is an obstruction in the uterus, the cause of which is often a split uterus and other uterine shape disorders.
A disorder of the cervix caused by a hereditary malformation or damage to the cervix.
In some cases, the mucus of the uterine cervix does not produce the type of mucus that allows sperm to move through the cervix, thus preventing sperm from moving into the uterus and to the released egg, and its subsequent fertilization.
Disorder of the fallopian tubes
Infections taking place in the pelvic area can cause scarring, even adhesion of the fallopian tubes, in which case their patency is impaired. Fallopian tube problems often occur after pelvic inflammatory diseases caused by sexually transmitted diseases such as chlamydia and gonorrhea.
The ovary can be adhered partially or completely. When partially glued, the ovary is passable for sperm but not for the size of the egg. In this case, ectopic fertilization often occurs.
Disorders of the hypothalamus
Hypothalamic dysfunction. The hypothalamus produces hormones called FSH - Follicle Stimulating Hormone and LH - Luteinizing Hormone, which are responsible for promoting ovulation. When there is a lot of stress, obesity, or conversely being underweight can interfere with the production of these hormones and thus interfere with ovulation.
A common symptom is cycle disruption to absence of menstruation.
Hyperprolactinemia
Excessive amounts of prolactin in a woman's body can be caused by the pituitary gland. Excessive production of prolactin decreases the production of the hormone estrogen and this cause infertility.
Congenital infertility, where there is no possibility of becoming pregnant because of a congenital disorder, such as Turner syndrome, where a woman is missing one X chromosome, thus limiting the activity of the gonads.
Causes that increase and cause infertility
- A woman's state of health, her lifestyle and age.
- As a woman ages, the possibility of becoming pregnant decreases and becomes a common factor in infertility. Women over 35 become at risk. Their egg count decreases, more eggs are laid. Have an abnormal number of chromosomes and are at increased risk of health problems.
- Hormonal disorders that prevent ovulation (endocrine gland disease).
- Abnormal menstrual cycle
- Obesity
- Being underweight
- Extreme exercise and from it a limited amount of subcutaneous fat.
- Endometriosiscan prevent the implantation of an egg or block the fallopian tubes with its growth.
- Autoimmune diseases of a woman when antibodies are formed against, for example, sperm, eggs or embryos.
- Sexually transmitted diseases
- Substance use
- Smoking
- Women after overcoming tubal ectopic pregnancy.
Prevention
Preventing the onset of disease, of any health problem, should come first. And it is lifestyle/lifestyle that has the exclusive place.
Measures that have some degree of impact are:
- Maintaining a healthy weight. Adequate exercise and physical activity. Strenuous exercise more than 5 hours per weeks reduces ovulation.
- Quit smoking. Smoking has an adverse effect on fertility as well as health.
- Do not drink alcohol. Excessive use of alcohol reduces fertility.
- Healthy lifestyle and stress avoidance. Stress also has a very adverse effect on fertility.
Symptoms
The main symptom is an attempt to conceive an offspring after unprotected sexual intercourse for more than one year and after the age of 35 for more than half a year.
Secondary infertility is a condition in which a couple has already produced offspring together in the past.
Primary infertility is a condition in which a couple has never been able to produce offspring.
In women, it is often associated with a menstrual cycle disorder, where menstrual bleeding is absent, irregular, or the cycle is too long, more than 35 days, or short, less than 21 days. These signs may mean that you are not ovulating.
In some cases, there may be no signs or symptoms.
However, infertility often results in mood changes and disturbances, possibly depression, and the overall psychological impact on the woman and the couple is quite great.
Diagnostics
For a correct diagnosis, it is necessary to visit a gynaecologist who will carry out a number of examinations to identify gynaecological causes and to examine other organs and systems affecting a woman's fertility.
After overcoming unsuccessful attempts at insemination, your gynaecologist will ask about your menstrual cycle, whether it is normal, regular, painful, past pregnancies, miscarriages, pelvic pain, vaginal bleeding and discharges.
Previous pelvic infections or a history of sexually transmitted diseases are detected.
Another very important question is how long the partners have been trying to procreate and how often they have had unprotected sex.
On the basis of the answered questions, a sequence of a series of examinations follows.
Ovulation test
The method of measuring basal temperature is considered too lengthy and not completely reliable.
Based on the blood test the level of the hormone progesterone is determined on the 21st day of the cycle.
In ultrasound folliculometry, the growth of the follicle is monitored and evaluated. Already on the 7th day of the cycle it can be detected and its growth should be about 2 mm per day. At a size of 17-25 mm, ovulation occurs.
Endometrial microabrasion is another examination where a sample is taken from the lining of the uterus during ovulation and the readiness of the lining of the uterus for the fertilized egg to nestle is assessed.
Determination of LH Luteinizing hormone, as an indicator of ovulation, is done using a urine strip. Ovulation occurs 32-36 hours after the peak LH level is reached.
Blood tests are carried out to screen for HIV and Hepatitis B and C, as well as screening for syphilis and other sexually transmitted diseases.
Hormonal examinations include examinations of hormone levels in the blood:
- Foliostimulating hormone - FSH will show the state of fertility - The collection is done on the 3rd day of the cycle. Values should not exceed 10mlU/ml, if it exceeds this there is a high probability of concealed ovarian failure although ovulatory cycles are possible in these women, the probability of fertilization is low. At a lower value, a lower follicle count and deterioration in follicle quality is expected.
- Estradiol E2 – This is a hormone produced by the ovaries, the collection is done on the 3rd day of the cycle in combination with the collection for FSH to detect ovulation, diagnose infertility, menstrual cycle disorders and the onset of menopause.
- Luteinizing hormone - LH promotes the production of progesterone and testosterone, promotes the formation of the corpus luteum as well as ovulation. Together LH with FSH is essential for follicle development. It is collected to detect ovulation, diagnose infertility, menstrual cycle disorders, and is important for the diagnosis of polycystic ovaries.
- Prolactin – It is a pituitary hormone. It is taken to evaluate menstrual cycle disorders, to detect decreased ovarian function, to diagnose infertility, and to rule out hyperprolactinemia.
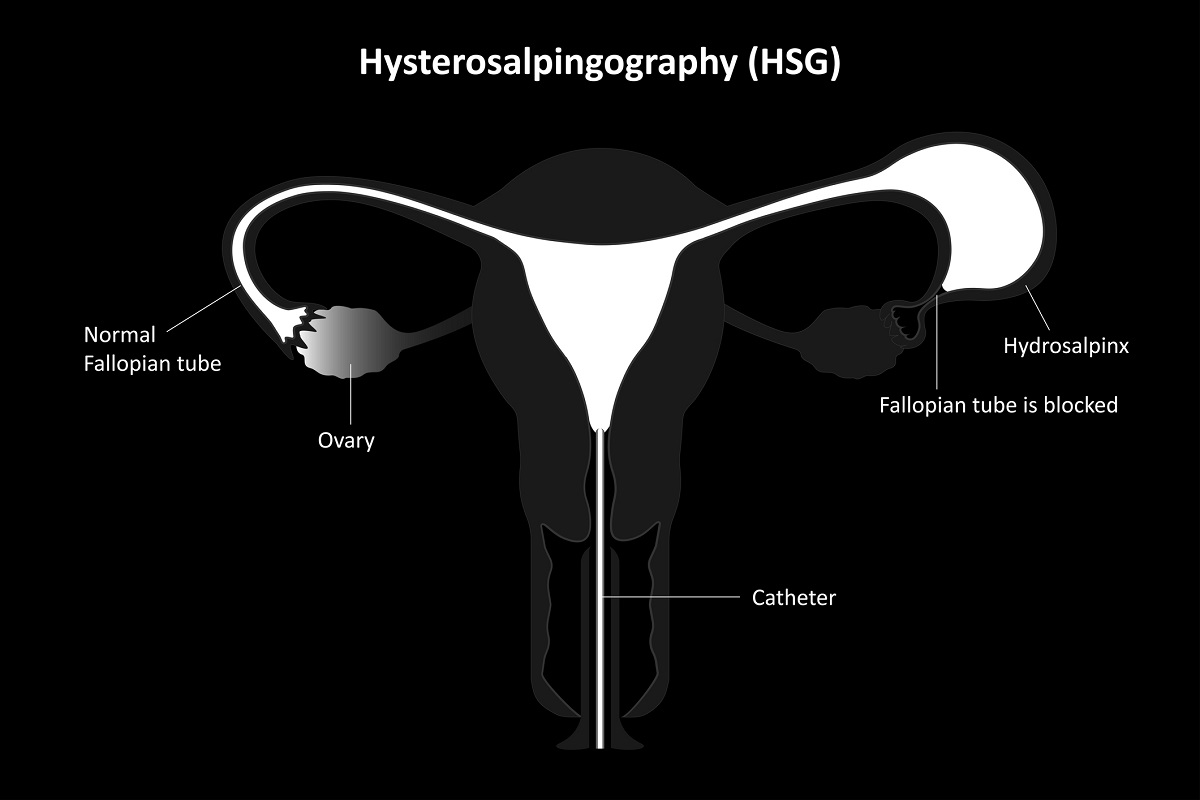
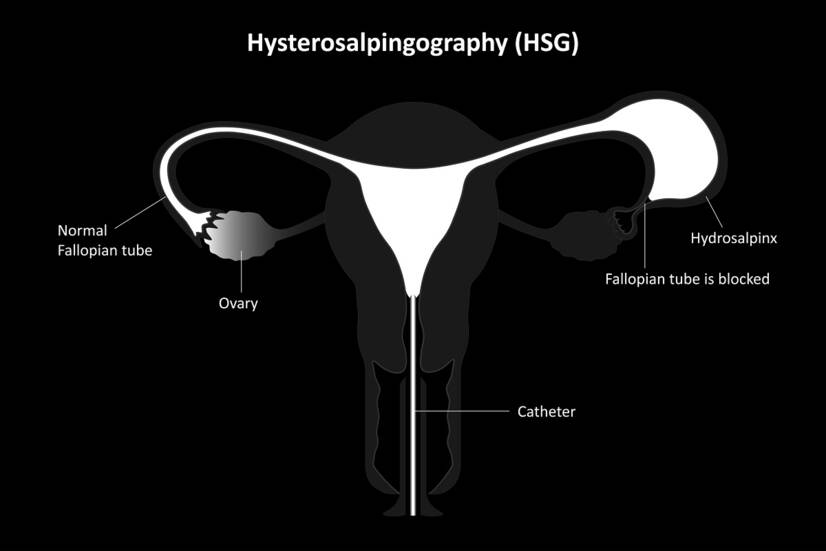
X-ray hysterosalpingogram (HSG). The advantage is that the uterus and fallopian tubes are examined at the same time. During the examination, a contrast agent is injected into the cervix, which passes through the uterus into the fallopian tube, and a subsequent X-ray is taken to determine the patency of the ovaries and the shape of the uterus.
Laparoscopy is indicated if a woman has had pelvic inflammatory disease, pelvic pain, a history of ectopic pregnancy, or a history of pelvic surgery.
A laparoscope with a camera is inserted through a small incision near the navel and the outer part of the uterus, ovaries and fallopian tubes are observed. The presence of changes, adhesions, or the presence of endometriosis is assessed. Enlargement or narrowing of the fallopian tubes may be visible. In the case of cysts or blockage of the ovary by endometriosis, adhesions are surgically removed and the blockage unblocked, and the cysts are removed.
Hysteroscopy is done through the uterine cervix, where a hysteroscope is inserted through the vagina, which is used to remove polyps and tumors on the lining of the uterus and by opening blocked fallopian tubes.
A transvaginal ultrasound is done at almost every examination of the uterus and ovaries.
Saline sonohysterogram (SIS) - is a special examination using ultrasound to assess the condition of the inner part of the uterus. This examination is done when uterine abnormalities are suspected and just before IVF.
Immunological examination. In this examination, women are evaluated for antisperm antibodies ASA in the blood and in cervical mucus, antiovarian antibodies and antiphospholipid antibodies, which prevent fertilization.
Genetic testing is indicated to detect premature or hidden ovarian failure, idiopathic sterility, recurrent and unsuccessful IVF, and habitual miscarriages.
Course
Female sterility according to the provoking causes can have different courses.
In some cases it is a congenital problem, other times the problem is triggered by another disease or after a difficult surgery.
Usually, infertility manifests only after unsuccessful insemination, whereby previously the woman did not even know that she had a fertility problem because she did not have any problems or symptoms.
How it is treated: Female Infertility
What are the treatment options for female infertility?
Show moreModern methods of Fertility Treatment
Gallery

Female Infertility is treated by
Other names
Interesting resources










