- Obstetrics: 3rd completely revised and supplemented edition Hájek Zdeněk, Čech Evžen, Maršál Karel, a kolektiv
- Nursing in Gynaecology and Obstetrics: 2nd completely revised and updated edition by Slezáková Lenka, a kolektiv
- Pathology for secondary medical schools: Janíková Jitka
- Mayoclinic.org - Ectopic Pregnancy.
- nhs.uk - Ectopic Pregnancy
- webmd.com - Ectopic (extrauterine) pregnancy
Ectopic pregnancy: what causes it and what are its symptoms?
An ectopic pregnancy occurs when a fertilized egg nests outside the uterus, most often in one of the ovaries. Why does this happen, where can the egg nest and what are the risks?
Most common symptoms
- Malaise
- Flank Pain
- Right Flank Pain
- Abdominal Pain
- Anal pain
- Lower Abdominal Pain
- Pain that Radiates into the Shoulder
- Frequent urination
- Frequent urge to urinate
- Cramps in the abdomen
- Nausea
- Bleeding
- Low blood pressure
- Mood disorders
- Head spinning
- Fatigue
- Vaginal discharge
- Vomiting
- Accelerated heart rate
Characteristics
Ectopic pregnancy, abbreviated as extrauterine pregnancy, is also called ectopic pregnancy.
Under normal conditions, the pregnancy begins with fertilisation of a loose egg in the dilated part of the fallopian tube. The fertilised egg then travels through the fallopian tube into the uterus. It nestles in the lining of the uterus, where it develops further. However, it may not reach the uterine cavity and may nest elsewhere. This leads to an ectopic pregnancy.
Their incidence is estimated at 1 in 200 pregnancies, but has been increasing over the years.
Only a functionally developed uterus provides an ideal place for the baby to develop, from nesting, development to birth.
An ectopic pregnancy occurs when a fertilized egg, during its journey, nests in a place that is not suitable for its further development.
The most common site is the fallopian tube, which occurs in 95-97% of cases. Other sites are rare, but nesting can also occur directly in the ovary, in the abdominal cavity and in the cervix at its junction with the vagina.
According to the location of the fertilised egg, ectopic pregnancies are divided into
- Tubal pregnancy, nesting in the fallopian tube
- Ovarian pregnancy, fertilization and nesting occur at the level of the ovary
- Abdominal pregnancy, fetal development occurs in the abdominal cavity
- Cervical pregnancy, nesting on the outside of the cervix at the junction with the vagina
In an ectopic pregnancy, the subsequent development of the fetus cannot proceed normally as in a healthy pregnancy. The fertilized egg cannot survive and the subsequent growth can cause complications for the woman, such as life-threatening bleeding.
Causes
An ectopic pregnancy occurs when an egg gets stuck in the fallopian tube during its journey to the uterus or is expelled into the abdominal cavity.
The incidence of ectopic pregnancy has been increasing over the years.
Its cause is not always known, but is related to the following conditions
Genetic abnormalities, congenital developmental defects of the internal genitalia, incomplete development of the fallopian tubes, which can be thin, long and their mobility is violated.
Inflammation or infection of the fallopian tubes and reproductive organs can cause impaired transport of the fertilized egg.
Frequent inflammations occur in women who have begun to live an early sexual life. Repeated infections cause post-inflammatory changes in the lining of the fallopian tube, which can lead to its deformation, scarring, narrowing and even complete impassability.
Chlamydia trachomatis is a very common infection causing blockage or obstruction of the fallopian tubes. Sexually transmitted diseases are also directly related to the disruption of the transport of the fertilized egg.
Pelvic inflammatory disease may not be directly related to early sex life or communicable disease. It may also be caused by appendicitis.
Endometriosis occurring in part of the fallopian tube.
Hormonal disorders and their imbalance.
Preputiation of the fetal egg. Return of the fertilised egg from the uterus to the fallopian tube cannot be ruled out.
Postoperative conditions, operations in the small pelvis and uterus can also be the cause of ectopic pregnancy. Subsequent formation of postoperative adhesions can adversely affect the relationship between the ovary and fallopian tube, sometimes their shape and transport functions.
The increase in ectopic pregnancies is also due to the increased use of assisted reproductive techniques. When a fertilized egg is introduced, it sometimes travels towards the fallopian tube.
The insertion of an IUD prevents the fertilised egg from nesting in the uterus.
Planning a pregnancy at an older age, the risk age for a woman is above 35 years.
Sterilization performed by simple tubal ligation.
Previous ectopic pregnancy.
Symptoms
An ectopic pregnancy initially manifests itself like any other normal pregnancy.
At first, there may be no signs of pregnancy and it is only caught accidentally.
Some women may notice early signs such as missed periods, tight and tender breasts, morning sickness and on examination a leaky and enlarged uterus is found.
After a pregnancy test, a positive result is found. After the fertilized egg has already nested, the hormone HCG begins to be produced. However, an ectopic pregnancy cannot continue as a normal pregnancy takes place in the uterus.
Early warning signs are light vaginal bleeding, brownish vaginal discharge and pelvic pain.
Between the 6th and 10th week after the fertilized egg has nested, lower abdominal pain occurs.

In tubal abortion, nesting in the fallopian tube, the woman feels alternating pain, from mild to intense pain in the lower abdomen, bleeds lightly or may have a brownish discharge. On blood sampling, anaemia is often found.
Common symptoms of ectopic pregnancy that require medical attention are
- Occasional lower abdominal pain, light bleeding or spotting
- Sharp, sharp, colicky abdominal pain that comes in waves
- Severe pain that occurs only on one side
- Pain may shoot under the shoulder blade, into the shoulder joint or neck
- Tightness of the abdominal wall
- Weak or heavy spotting, genital bleeding
- Urge to urinate
- Pressure in the rectal area
If the fallopian tube ruptures or a heavily engorged organ becomes stuck in the abdominal cavity, bleeding occurs.
This is a life-threatening condition that presents with symptoms of sudden abdominal stroke. The woman goes into a state of shock, her blood pressure drops, her pulse rises. She is pale, weak, may fall unconscious. She has a thready, non-palpable pulse, rapid breathing and a feeling of anxiety.
Diagnostics
Nowadays, there is earlier and better diagnosis. In the past, such possibility of early diagnosis as today did not exist. Many ectopic pregnancies, if they did not threaten the life of a woman, were previously absorbed and went unnoticed.
An important part of early diagnosis is taking a medical history. It is taken to find out when the last menstrual period was, whether it was late, whether it was missed. The doctor examines whether the woman has any risk factors such as history of inflammation, spotting, and whether there were any early signs of pregnancy.
A gynaecological examination is performed. On examination, the lower abdominal area may be tender to painful. The uterus is swollen, soft and enlarged.
The doctor observes the area between the rectum and the vagina, called the Douglas space. In the case of an ectopic pregnancy, this area is bulging, indicating bleeding into the abdominal cavity and subsequent blood flow into this space.
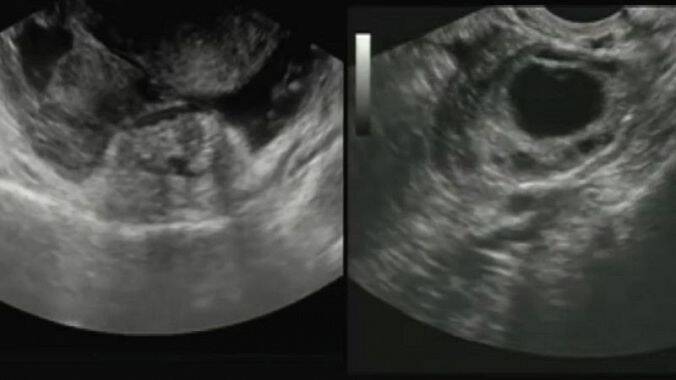
To prove pregnancy, an ultrasound examination is performed to detect the presence of a gestational sac in the uterus.
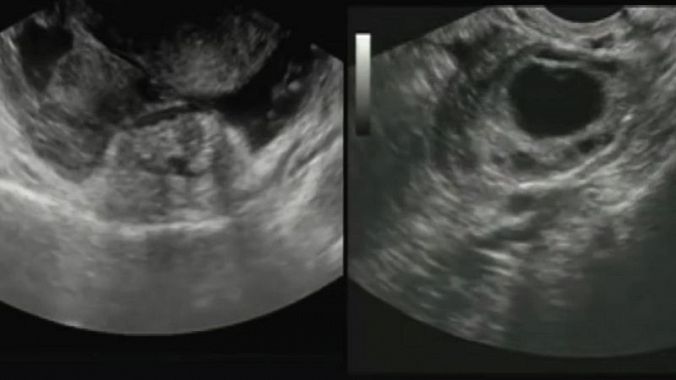
In the case of ectopic pregnancy, fluid in the Douglas space is confirmed.
Sometimes a fetal heartbeat is visible outside the uterus, or an enlarged fallopian tube. A fetal sac may be present in the uterus without signs of pregnancy.
Laboratory examination: Urine and blood tests for HCG and progesterone will confirm pregnancy. If the values begin to decrease or remain the same within a few days and there is no gestational sac present on ultrasound, it is probably an ectopic pregnancy.
Blood is taken for a blood count. A decreased hemoglobin value will show internal bleeding, and increased leukocytes indicate the presence of an inflammatory process taking place in the woman's body. Blood type and Rh factor, coagulation factors, liver tests are also examined, which are necessary in case of surgery.
In some cases, laparoscopy is performed for diagnosis, which is a direct method of visible changes in the organs in the small pelvis and possible nesting of the egg in the abdominal cavity and fallopian tube.
In the case of severe and life-threatening symptoms, there is not enough time to perform all the steps of diagnosis. Such a condition is considered a sudden abdominal episode, and urgent surgery is performed, which is necessary to start immediate treatment.
Course
Most fetal eggs die and resorb unnoticed, without the woman knowing that the egg has been fertilized.
If the fertilized egg, which is beginning to nucleate, is not found in the uterus, an ectopic pregnancy occurs.
Its further development is determined by its location, in which part it is located and, above all, by the blood supply to the area, its anatomical structure, its elasticity and strength.
If it nestles in a place with insufficient blood supply, the fertilised egg is not sufficiently nourished. Eventually it dies and its partial absorption subsequently leads to delayed menstruation.
Sometimes it happens that in its rapid development it outgrows the wall of the organ in an attempt to secure a sufficient supply of blood from the mother's body. This disrupts the wall of the blood vessels, which may cause sudden hemorrhage. Sometimes such a pregnancy located in the fallopian tube strains its wall by its growth, which cannot withstand the onslaught of the growing fetal egg and ends up rupturing.
These complications most often occur in the 8th week of pregnancy, no later than the 1st trimester. In very rare cases, the fetus grows up to the period of fetal viability.
Tubal abortion can take several forms. It can manifest as chronic inflammation or as a life-threatening condition. Chronic inflammation can occur when the fetus dies in the fallopian tube without disrupting its wall and the subsequent abortion is expelled by contractions of the fallopian tube muscles into the abdominal cavity.
The further development of the fertilised egg can take place in the fallopian tube. However, by continuous contractions of the fallopian tube, the fetal egg is expelled into the abdominal cavity. It first detaches from the wall of the fallopian tube, the fallopian tube vessels are disrupted and the amniotic sac is congested, turning the embryo into a 'mole'.
Blood from the disrupted vessels then flows in the abdominal cavity into the Douglas space, where it accumulates. In this case, tubal abortion occurs between the 6th and 8th week.
It may happen that a fertilized egg nests in the fallopian tube and develops there without being expelled into the abdominal cavity. This is often the result of an inflammatory process in the fallopian tube. When the egg nests, the wall of the fallopian tube erodes. The erosion weakens the wall and creates a high risk of rupture of the fallopian tube wall, a life-threatening condition.
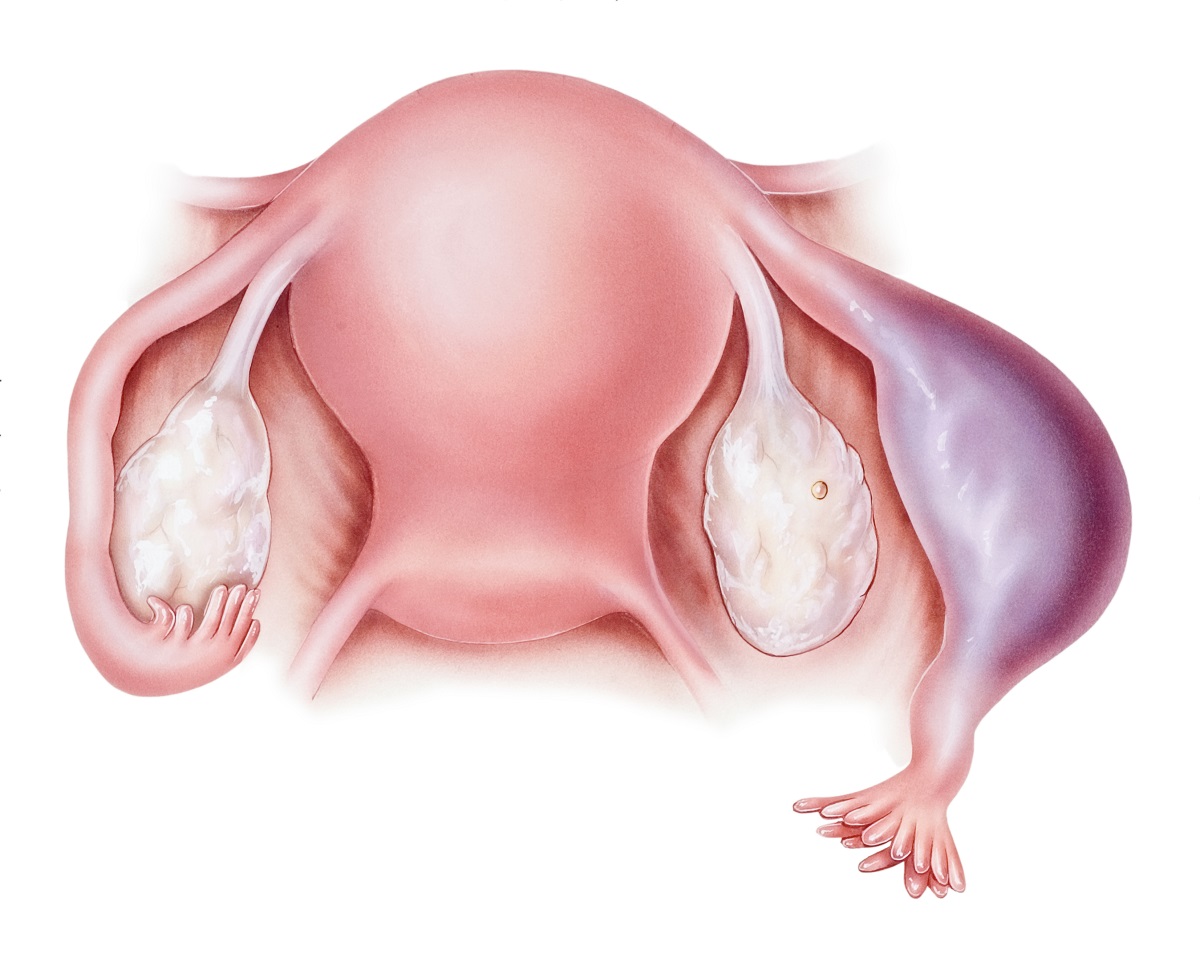
Ovarian pregnancy occurs at the level of the ovary. The cause is the retention of the egg in the ruptured follicle, where the egg is not fully released or is trapped and fertilised by the sperm.
In an abdominal pregnancy, the development of the fetus occurs in the abdominal cavity when the fertilized egg nests on an organ. If it nests on an organ that is heavily vascularized, bleeding into the abdominal cavity occurs. This type of ectopic pregnancy can occur after the embryo dies without apparent cause. If the fetus dies at an early stage when it is still small, it is absorbed.
A cervical pregnancy is the nesting of a fertilized egg on the cervix. In this case, there is a high risk of bleeding due to the occlusion of a major blood vessel feeding the uterus, causing vaginal bleeding. Sometimes, even after the pregnancy has ended, the bleeding cannot be stopped and the uterus must be removed.
Only in very rare cases does the ectopic fetus survive. If the fetal placenta is located in a place where there is an adequate blood supply, it supplies the fetus with sufficient nutrients. However, as the fetus develops, it needs more and more nutrients for its development.
As a result of inadequate nutrition, its development may regress and become mummified. Calcium salts then begin to accumulate in the fetus, resulting in a fossilised fetus.
There are also known cases in which an ectopic pregnancy was detected during an accidental examination of the abdominal cavity. The fetus developed to the size of a premature fetus and had to be surgically removed. Such fetuses were deformed and postulated as a result of pressure from surrounding organs.
Ectopic pregnancy and menstruation
An ectopic pregnancy is characterised by a number of symptoms that distinguish it from a normal intrauterine pregnancy. A woman may first experience pain in the lower abdomen and irregular uterine bleeding caused by various hormonal changes.
During pregnancy, light spotting appears during the period usual for menstruation. Gradually, the pain increases and, as a rule, irregular bleeding may appear in the period of 6 to 8 weeks from the last menstruation. Sometimes it is more visible, sometimes less.
If acute sharp pain is added to this, the ovary may rupture. In this case, medical help should be sought immediately, otherwise there is a risk of massive bleeding into the abdominal cavity.
How it is treated: Ectopic pregnancy
Treatment of ectopic pregnancy: termination of pregnancy, medication, surgery
Show moreVideo about what is ectopic pregnancy and how it manifests itself
Gallery


Ectopic pregnancy is treated by
Other names
Interesting resources










