- medicalnewstoday.com - Everything you need to know about erysipelas
- ncbi.nlm.nih.gov - Erysipelas
- solen.sk - Erysipelas - diagnosis and treatment
- solen.com - Erysipelas with serious internal complications
- prolekare.cz - Erysipelas and cellulitis
- prolekare.cz - Streptococcal and pneumococcal infections from the perspective of a geriatrician, M. Pýchová; P. Husa; R. Pařízková; A. Hajná
Erysipelas: Why is rose an infectious disease, is it transmissible? + Symptoms

Erysipelas is a common acute infectious skin disease. Human-to-human transmission is rare.
Most common symptoms
- Malaise
- Tremors
- Headache
- Skin pain
- Painful Lymph Nodes
- Fever
- Increased body temperature
- Nausea
- Indigestion
- Low blood pressure
- Swelling of the limbs
- The Island
- Blisters
- Itchy skin
- Fatigue
- Vomiting
- Reddened skin
- Winterreise
- Accelerated heart rate
- Enlarged lymph nodes
Characteristics
Erysipelas is defined as an acute streptococcal disease of the skin and subcutaneous connective tissue. It is accompanied by general symptoms.
It is most common on the feet, especially on the shins (90%).
It is less common on the hands, face and neck. However, it can occur in other locations. For example, in the lumbar region in patients with artificial hip joint implants.
Erysipelas = erysipelus = rose.
The disease can affect a patient at any age. The highest incidence is between 60 and 80 years of age. It occurs in both sexes equally.
Erysipelas has a worldwide incidence. Comparing the USA and Europe, for example, the aetiology, clinical picture and treatment are similar in both cases. The incidence is higher in the summer months.
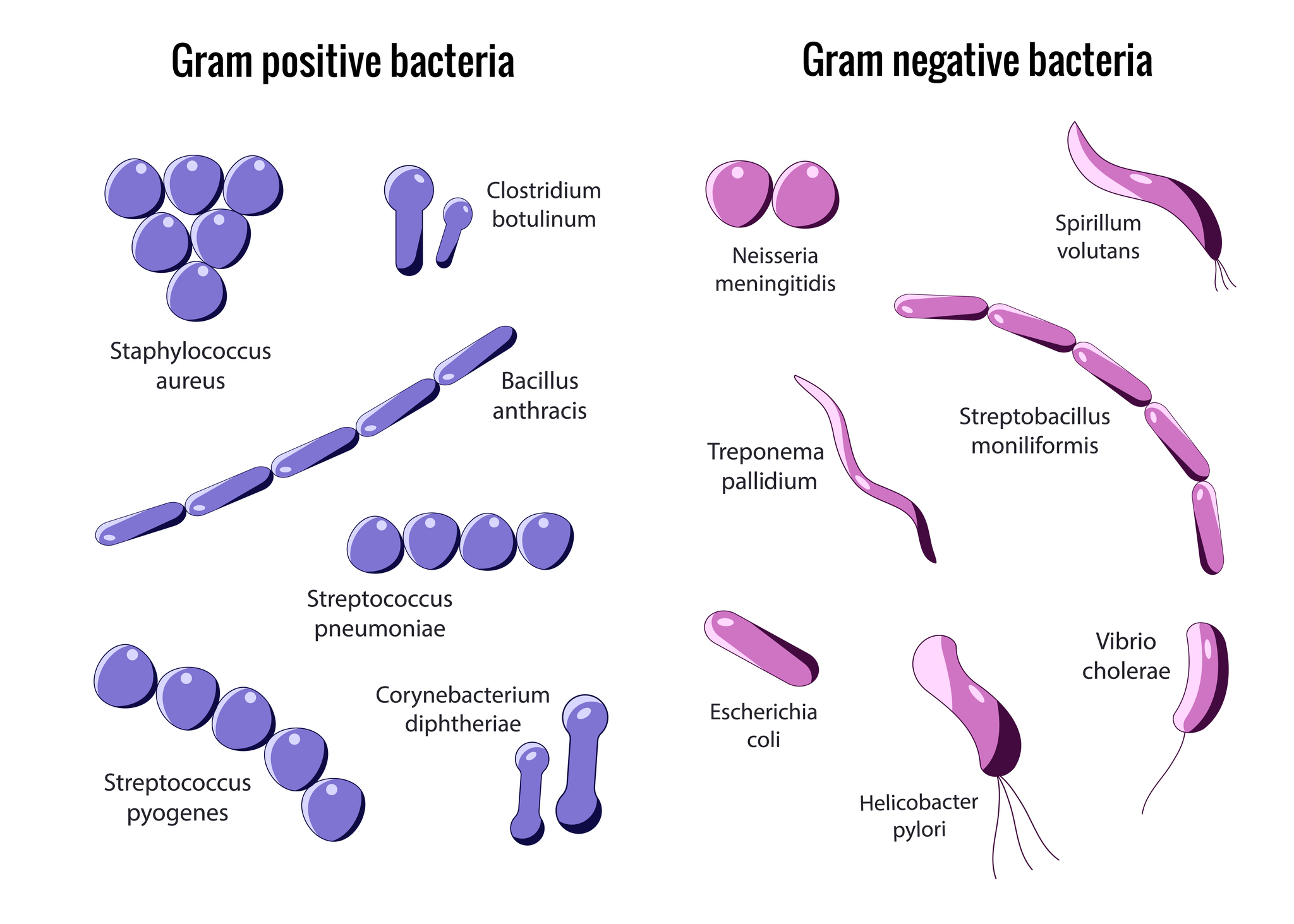
Erysipelas belongs to the group of bacterial skin infections (pyoderma). The most common causative agents of pyoderma are Staphylococcus aureus and group A β-haemolytic streptococci.
The incidence of infection depends on the following factors:
- general condition of the organism - systemic diseases
- local skin condition - chronic skin diseases, skin injuries
- characteristics of the bacteria - virulence
- influence of the external environment - temperature, humidity
Pyodermas can be divided into two groups. The first group consists of primary pyodermas, which include impetigo, furuncle, carbuncle and erysipelas.
The second group are secondary bacterial infections that further complicate pre-existing skin changes. Examples are secondary infections on eczema, ulcers, skin wounds, burns or chickenpox.
The following table gives an overview of pyoderma by causative agent
| Golden staphylococcus aureus | Streptococcus pyogenes |
| Bullous impetigo | Non-cellular impetigo |
| Dermatitis exfoliativa staphylogenes | Ecthyma |
| Folliculitis | Erysipelas |
| Furunkl | |
| Carbuncle | |
| Hidradenitis suppurativa |
Causes
The causative agent of erysipelas is Streptococcus pyogenes (beta-hemolytic group A streptococcus).
Streptococci are a diverse group of bacteria:
- viridal streptococci in the oral cavity and vagina - part of the physiological flora of mucous membranes
- primarily pathogenic - S. pneumoniae, S. pyogenes, S. agalactiae
- conditionally pathogenic - S. mutans, S. milleri
The S. pyogenes envelope contains hyaluronic acid. This is indistinguishable from hyaluronic acid in connective tissue. The envelope is weakly immunogenic, allowing the bacteria to escape immune mechanisms.
What diseases are caused by different types of streptococci?
- Streptococcus pyogenes - pharyngitis, skin and soft tissue infections, bacteremia, rheumatic fever, glomerulonephritis
- Streptococcus agalactiae - neonatal infections, endometritis, urinary tract infections, wound infections, bacteraemia, pneumonia, skin and soft tissue infections
- Streptococcus dysgalactia - pharyngitis, acute glomerulonephritis
- Streptococcus anginosus - abscesses
Streptococcus pyogenes causes angina, pharyngitis and skin infections (impetigo, pyoderma, cellulitis, phlegmon). Strains that produce erythrogenic toxin cause erysipelas.
Some strains can cause late sequelae of streptococcal infections (rheumatic fever, acute glomerulonephritis).
The causative agent of erysipelas usually enters the body at a site where the skin barrier is breached. The predilection sites on the shins and face are considered as entry points.
A certain spatial distance between the erysipelas and the site of entry of the pathogen is typical. Examples are the ragades in the interdigital spaces of the lower limbs (entry of the pathogen) and the subsequent erysipelas on the shins.
The nasopharynx is considered the source of the pathogen.
The most common factors contributing to erysipelas include minor injuries, disorders of venous and lymphatic circulation, diabetes mellitus and alcoholism. Prolonged standing or strenuous hiking for several hours may also play a role.
Predisposing factors for first attacks of erysipelas may be local, systemic or social. Social factors include poor hygiene.
In the following table, we list each of the local and overall predisposing factors
| Local | Overall |
| Broken skin barrier | Obesity |
| Eczema | Diabetes mellitus |
| Herpes zoster | Nephrotic syndrome |
| Herpes simplex | Immunosuppression |
| Tinea pedis | Chronic venous insufficiency |
| Onychomycosis | Neurological disorders |
Symptoms
The incubation period lasts from a few hours to two days.
The disease starts suddenly with chills and fever (40 °C). Symptoms such as nausea, malaise and headache also appear.
Within a few hours, an asymmetrically localised, intensely red, flat, oedematous lesion appears on the skin. The lesion spreads rapidly into the surrounding area. The lesion is well circumscribed. It protrudes into the surrounding area in typical tongue-like projections.
Patients often experience tingling or mild pain before the redness develops. The redness spreads into the surrounding area at a rate of approximately 2 to 10 cm per day. It may reach large sizes. Regional lymph nodes may be enlarged and painful.
With a more severe course, vesicles, pustules, blisters or small areas of haemorrhagic necrosis may appear.

The most common symptoms of erysipelas include:
- erythema (redness of the skin), which is flat and painful.
- swelling
- overheating
- chills
- fever
- headache
- lymphangitis
- lymphadenitis
Tachycardia and hypotension may also occur. These symptoms signal a more severe course of the disease.
We distinguish the following types of erysipelas:
- Erysipelas erythematosum - The surface of the lesion is warm and slightly painful to the touch.
- Erysipelas vesiculosum et bullosum - In this type, blisters and large vesicles appear on the erythema.
- Erysipelas gangraenosum - A necrotic form that occurs with weakened immunity or predisposing factors.
- Erysipelas phlegmonosum - Occurs when the process migrates to the subcutaneous connective tissue. Phlegmon to abscesses may form this way.
What is a phlegmon?
A phlegmon is a violent purulent inflammatory process that takes place in the subcutaneous tissue. From there it spreads upwards (to the skin) and downwards (to the tendons and fascia). It is caused by the introduction of infection into the deeper layers after injuries, erysipelas and others.
Erysipelas on the face is very common and dangerous. It starts in the saddle of the nose and spreads in a butterfly pattern. Bilateral swelling of the eyelashes occurs.
Erysipelas can also affect the mucous membranes. Erysipelas of the larynx is very dangerous and can be fatal.
Erysipelas of the vulva is manifested by massive swelling and reddening of the labia minora, which may necrotically disintegrate. Erysipelas of the penis may also be gangrenous.
Diagnostics
Diagnosis is made on the basis of clinical signs (fever, chills, high sedimentation rate, leukocytosis). The basis of diagnosis is the history, clinical picture and laboratory examination.
Laboratory results show leukocytosis. Other inflammatory parameters such as sedimentation rate and C-reactive protein (CRP) are also elevated.
An excellent indicator of streptococcal infection is antistreptolysin O (ASLO).
What is ASLO?
Antistreptolysin O (ASLO) is a protein produced against the antigen streptolysin O. It is part of the cell wall of group A streptococci.
Elevated levels of ASLO alert us that antibodies against streptococci are circulating in our body, but also against our own tissues. The normal level in healthy adults is 200 IU/ml. In children, the level is higher (400 IU/ml).
In practice, we must assess the dynamics of the antibody response. Antibodies to streptolysin appear in the blood approximately 1 to 3 weeks after the outbreak of infection.
Maximum levels usually appear after 3 to 6 weeks. Normal levels are reached within 6 to 12 months.
Differential diagnosis
In some cases, the diagnosis of erysipelas is misdiagnosed. Most commonly, eczema, lymphedema and lipodermatosclerosis are misdiagnosed as erysipelas.
Examples of differential diagnosis are given in the following table
| Infectious diseases | Non-infectious diseases | Vein disease |
| Erythema migrans | Contact irritant dermatitis | Deep vein thrombosis |
| Herpes zoster | Contact allergic eczema | Superficial thrombophlebitis |
| Osteomyelitis | Local allergic reaction to insect bites | |
| Septic arthritis | Acute gout | Stasis dermatitis |
| Septic bursitis | Carcinoma erysipelatoides | Lipodermatosclerosis |
| Vasculitis |
Course
In the normal erythematous form, the temperature begins to drop after a week, the inflammation subsides and the process heals. Erysipelas does not leave immunity. Multiple relapses are frequent. Various erosions and fissures (ragades) are the gateway for the entry of infection.
What are the complications of erysipelas?
Complications occur especially in cases where the disease is treated late. With significant swelling, blisters form. These are filled with serous fluid. Secondary staphylococcal infection leads to their impetiginization.
Blisters are more common in elderly patients with atrophic skin. Abscess is also a local complication.
Rare complications include bacteremia and septicemia (less than 5%). Recurrence of the disease is a frequent complication (15% to 34%). The cause is persistence and untreated risk factors.
Such risk factors include:
- swelling
- tibial ulcer
- onychomycosis
- injury
- minor skin injuries
- overweight
Other complications include:
- Myocarditis, endocarditis or pericarditis.
- glomerulonephritis
- rheumatic joint involvement
- metastatic pneumonia
- lymphoedema
- local tissue devastation
- phlebothrombosis
Currently, the above complications are rare. They can occur in children, the elderly and patients with risk factors. The prognosis of the disease is very good with early treatment.
How it is treated: Erysipelas - rose
Treatment of erysipelas, rose: Medications, antibiotics and topical ointments
Show moreErysipelas is treated by
Other names
Interesting resources










