- ROZTOČIL, Aleš and Pavel BARTOŠ. Modern Gynaecology. Prague: Grada, 2011. ISBN 978-80-247-2832-2
- healthline.com - Cervical Dysplasia: Causes, Risk Factors, Diagnosis, and More. Healthline. Jaime Herndon
- nierakovine.sk - Symptoms, diagnosis, treatment of cervical cancer. No to cancer
- emedicine.medscape.com - Conization of Cervix. MedScape. Istvan Nyirjesy
What is cervical conization and how is it performed? Recovery and pregnancy

Cervical disease can be an indication for surgery - conization. How does the surgery and subsequent recovery proceed? What risks can cervical conization bring?
Article content
Cervical conization is a surgical procedure that removes abnormal cervical tissue. What causes unwanted changes to the cervix? When is the procedure necessary and what are the risks?
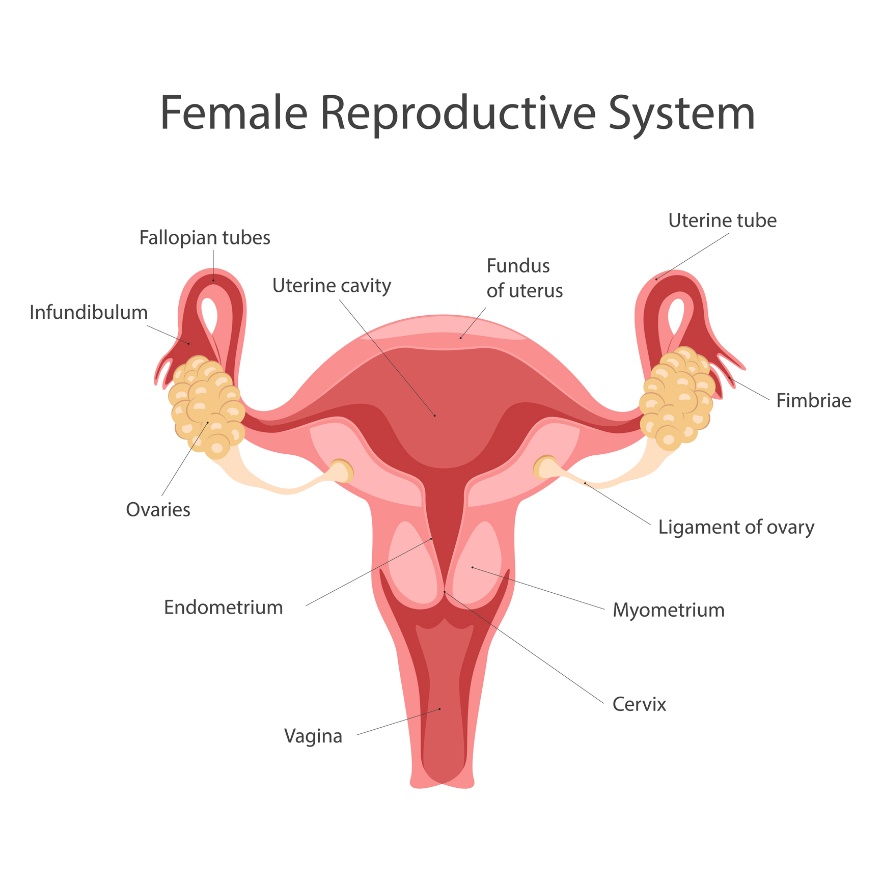
The cervix in a nutshell
The cervix is a convex circular formation located between the uterus and the vaginal tube. A narrow canal passes through the cervix and forms an opening into the uterus.
A woman can palpate the cervix per vaginam because it is located at the end of the vaginal tube. During menstruation, the cervical canal opens slightly to allow blood to pass from the uterus into the vagina, but not in the opposite direction.
At the same time, the cervix allows the passage of male sperm to the egg. The cervical mucus produced by the cervix plays an important role in ovulation and pregnancy. It is also nicknamed as fertile mucus because it improves the patency and longevity of male sperm.
Subsequently, during pregnancy, the cervix closes and fills with more secretion, which closes the birth canal and protects the fetus from infection from the outside environment.
In pregnancy, it serves as a protection for the baby from premature birth and at the same time, by opening at the right time, it allows birth through the woman's natural ways.
The basis of prevention of cervical health is a regular preventive examination by a gynaecologist. The cervix can be threatened by an inflammatory process, polyp, fibroid, sexually transmitted disease or carcinoma.
The indication for conization is mainly cervical disease with HPV.
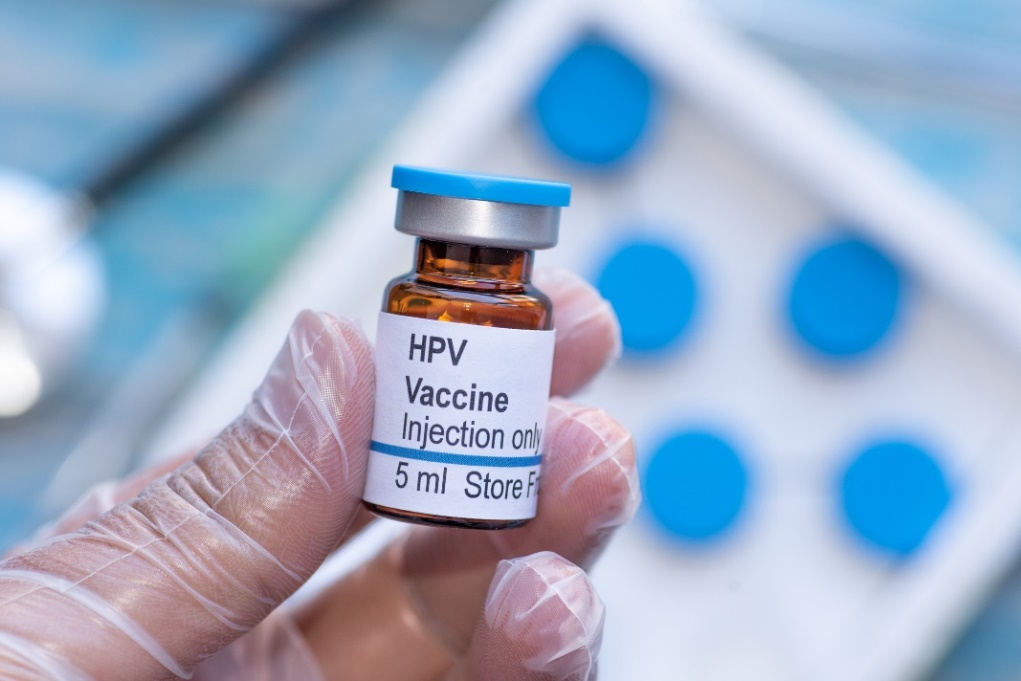
HPV virus
Human papillomavirus (HPV) is a common virus that is transmitted through the skin and through interpersonal sexual contact. Up to 80% of the population of women and men will be repeatedly exposed to HPV during their lifetime.
In approximately 20% of cases of HPV infection, the disease can become life-threatening or even fatal. Early diagnosis and treatment by a specialist is therefore recommended.
The human papillomavirus HPV is the cause of more than 95% of cervical cancers.
The key to HPV prevention is a strong immune system, sexual abstinence, a non-discreet lifestyle, sexual protection, regular gynecological exams and HPV vaccination.
The HPV vaccine should be given before a woman starts having sex. However, women who have already had sex can also be vaccinated against HPV. Consultation with a gynaecologist is recommended.
Read also.
Diagnosis of HPV on the cervix
The presence of HPV cervical virus can be detected from a cytology swab directly from the patient's cervix using a special brush. The cervical cytology swab is part of a preventive examination by a gynecologist.
The cytological examination helps to detect whether there are any unwanted changes on the cervix. In most cases, they appear before a woman develops the first symptoms. The examination may be slightly uncomfortable, but it is not painful.
The actual examination of the sample then takes place in the laboratory where the swab was sent.
Regular prevention by a gynaecologist prevents abnormal changes on the cervix, pre-cancerous stages and the development of cancer.
Abnormal changes on the cervix
The tissue on the cervix can be changed and may not immediately be cervical cancer.
There is a professional scale for these abnormal changes. It determines whether they are benign changes for which regular outpatient monitoring and certain lifestyle modifications are sufficient.
Conversely, in some cases, surgery to remove the changed cervical tissue is necessary. When cervical conization is suspected, it is often performed as a preventive measure to prevent the cervical changes from developing into a more serious disease.
In many cases, it is not cervical cancer directly, but pre-cancerous changes called cervical dysplasia. This is the presence of abnormal cells in the lining of the cervix.
Professionally, these precancerous changes of the cervix are called cervical intraepithelial neoplasia - CIN.
There are 3 types of cervical dysplasia according to the thickness (part) of the mucosa affected by this disease:
- mild CIN 1 dysplasia
- moderate dysplasia CIN 2
- severe dysplasia CIN 3
CIN 2 and especially CIN 3 have a high likelihood of subsequent cervical cancer. Surgery (conization) is required to remove the affected part of the cervical tissue.
The eventual development of cervical cancer is a process that has several stages. In the process of transforming a normal cell into a cancerous cell, infection of the cells in the deepest layer of the cervical mucosa is crucial.
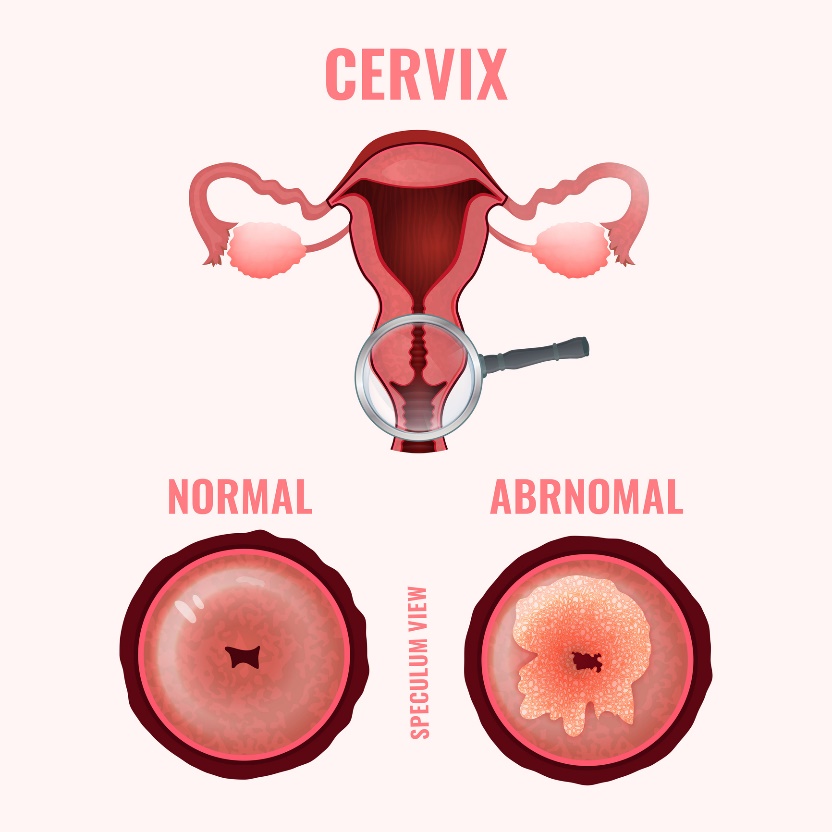
In most cases, a woman does not experience the initial symptoms and learns about the change on the cervix only after a cytological smear performed by a gynecologist.
However, in more advanced stages, she may notice specific symptoms:
- Heavy menstrual bleeding
- Weak off-cycle bleeding
- Long menstrual phase
- Painful intercourse
- Pain in the lower abdomen and pelvis
- Unusual vaginal discharge
- Unpleasant odour
Prevention of abnormal cervical changes
The prevention of HPV infection and the formation of abnormal cells in the cervical mucosa is the elimination of HPV infection. Protected intercourse is therefore essential as protection against sexually transmitted diseases.
Prevention of cervical health:
- A strong immune system and immunity
- Healthy lifestyle
- Unpromiscuity
- Sexual protection
- HPV vaccination
- Good intimate hygiene
- Preventive gynaecological check-ups
- Elimination of urogynecological inflammation
- Limiting smoking of tobacco products
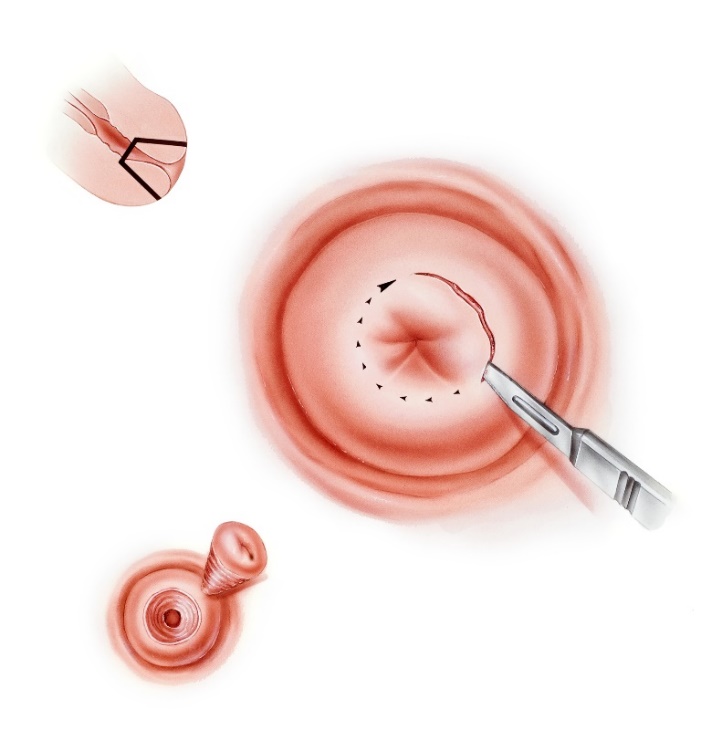
Cervical conization
Cervical conization is a short, common surgical procedure. During surgery, abnormal, unwanted tissue lining the cervix is removed.
The procedure is primarily used to remove pre-cancerous changes to the cervix caused by the development of HPV.
Conization is the removal of abnormal tissue in the shape of an imaginary cone. The size of the cone is determined by the extent and depth of the changes in the cervical tissue. Properly and gently performed, conization removes HPV-infected cells and leaves healthy cervical tissue.
Leaving as much healthy tissue as possible is important for the patient's future pregnancy. The cervix should be firm enough not to endanger the baby by loosening and premature birth.
Surgery is usually performed under general anaesthesia (after the patient has been put to sleep) or, less commonly, under local anaesthesia (numbing part of the body). Before surgery, an internal pre-operative examination is necessary.
The procedure of cervical conization can currently be performed in different ways: with a scalpel, laser, LEEP or cryotherapy.
In the LEEP (loop electro excision procedure), a small special wire handpiece is used to remove the changed infected tissue. A low-voltage electric current is used to remove the abnormal cervical tissue.
In LEEP, the conus is removed electrically. The action of the electric current also stops bleeding from the resulting wound.
It is currently the most commonly used method. It is used to treat both more and less severe cervical changes. The advantage of this method is its suitability for women who are planning a pregnancy in the future.
The LEEP procedure is usually performed under short-term anaesthesia and the patient goes home on the day of the procedure.
Laser conization is based on the use of an instrumented laser that vaporizes (removes) the altered, damaged cervical tissue. The patient goes home on the day of the procedure.
Scalpel conization is appropriate if the damaged tissue extends high and deeper into the cervical canal. However, this method is disadvantageous if the woman plans to become pregnant in the future. The patient remains in hospital for several days after the procedure.
Cryotherapy is a method that uses the effect of cold in the form of liquid nitrogen. The tissue is frozen and thus removed. It is mainly used for less severe changes, but it requires a long healing time, so it is rarely used.
Recovery after the procedure
Due to the routine nature of the procedure and the use of modern surgical methods, recovery after cervical conization is relatively quick and uneventful.
After the procedure, the cervix takes approximately 6 weeks to heal. During the recovery period, it is advisable to limit excessive physical activity and physical and mental stress on the body.
It is not recommended to bathe, have sexual intercourse, use vaginal tampons or apply other objects per vaginam after the procedure.
The presence of postoperative light bleeding or spotting is possible. If a woman bleeds lightly, she may use menstrual pads but not vaginal tampons.
It is not recommended to visit swimming pools, sauna or wellness centres where there is an increased risk of infection. Home showering is appropriate.
If postoperative bleeding is heavier than menstruation, an elevated temperature is present, or a woman notices an unusually foul-smelling discharge, she should see a doctor.
In some cases, pre-cancerous changes may reappear and recur after the procedure. Therefore, the postoperative condition requires regular outpatient follow-up.
Rare complications include the development of heavy vaginal bleeding during the procedure or in the short postoperative period.
The occurrence of inflammatory postoperative complications is equally rare and requires subsequent pharmacological treatment in the form of antibiotics. Quite rarely, injury to surrounding organs may occur.
Cervical conization and pregnancy
The cervix has the task of supporting the weight of the growing uterus during pregnancy. Its condition and strength are therefore very important. The cervix is mainly used in the second half of pregnancy, when it serves as a functional closure of the uterus and maintains the position of the fetus in the uterus.
Subsequently, at birth, the cervix must open and dilate sufficiently to allow the newborn to pass through it.
Before the procedure, it is therefore necessary to consult the health of the cervix with the gynaecologist and surgeon, who will inform the patient about possible post-operative risks and complications.
The function and condition of the cervix depends on the amount of tissue removed and the surgical procedure chosen.
A properly and gently performed conisation to remove pre-cancerous changes does not automatically mean that it is difficult or impossible to conceive. However, consultation with a gynaecologist and surgeon is necessary.
After the conization procedure, it is recommended to have at least a six-month interval between conization and pregnancy.
Interesting resources
Related










