- mayoclinic.org - Cervical cancer
- medicalnewstoday.com - What you need to know about cervical cancer
- cancer.gov - Cervical Cancer - Patient Version
- World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 5.12. ISBN 978-9283204299.
- "Cervical Cancer Treatment (PDQ®)". National Cancer Institute. 14 March 2014.
- Kumar V, Abbas AK, Fausto N, Mitchell RN (2007). Robbins Basic Pathology (8th ed.). Saunders Elsevier. pp. 718–721. ISBN 978-1-4160-2973-1.
- Kufe D (2009). Holland-Frei cancer medicine (8th ed.). New York: McGraw-Hill Medical. p. 1299. ISBN 9781607950141.
- Bosch FX, de Sanjosé S (2007). "The epidemiology of human papillomavirus infection and cervical cancer". Disease Markers. 23 (4): 213–227.
- "Cervical Cancer Prevention (PDQ®)". National Cancer Institute.
- "Human Papillomavirus (HPV) Vaccines". National Cancer Institute. 29 December 2011.
- "Global Cancer Facts & Figures 3rd Edition" (PDF). 2015. p. 9.
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (May 2021). "Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries". CA: A Cancer Journal for Clinicians. 71 (3): 209–249.
- "Defining Cancer". National Cancer Institute. 17 September 2007.
- Yadav, Prakash Chand; Pandey, Shibendra Raj; Thapa, Ankit; Kishor Chaudhary, Deepak; Sah, Krishna Kumar (30 October 2021). "Updates on Cervical Cancer". North American Academic Research Journal.
- Tarney CM, Han J (2014). "Postcoital bleeding: a review on etiology, diagnosis, and management". Obstetrics and Gynecology International. 2014: 192087.
- Dunne EF, Park IU (December 2013). "HPV and HPV-associated diseases". Infectious Disease Clinics of North America. 27 (4): 765–778.
- Ramachandran D, Dörk T (October 2021). "Genomic Risk Factors for Cervical Cancer". Cancers. 13 (20): 5137.
- "FDA approves Gardasil 9 for prevention of certain cancers caused by five additional types of HPV". U.S. Food and Drug Administration. 10 December 2014.
- Tran NP, Hung CF, Roden R, Wu TC (2014). Control of HPV infection and related cancer through vaccination. Recent Results in Cancer Research. Vol. 193. pp. 149–71.
- World Health Organization (February 2014). "Fact sheet No. 297: Cancer".
- "SEER Stat Fact Sheets: Cervix Uteri Cancer". NCI. National Cancer Institute. 10 November 2014.
- World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 1.1. ISBN 978-9283204299.
- "Cervical cancer prevention and control saves lives in the Republic of Korea". World Health Organization. Retrieved 1 November 2018.
- Canavan TP, Doshi NR (March 2000). "Cervical cancer". American Family Physician. 61 (5): 1369–1376.
Cervical Cancer: Causes, Symptoms, Prevention
Photo source: Getty images
Most common symptoms
- Malaise
- Vaginal Discharge
- Abdominal Pain
- Urethral pain
- Lower Abdominal Pain
- Painful urination
- Back Pain
- Bleeding after sexual intercourse
- Indigestion
- Nausea
- Swelling of the limbs
- The Island
- Menstrual cycle disorders
- Smelly discharge from the vagina
- Fatigue
- Vaginal discharge
- Water in the abdomen
- Enlarged lymph nodes
Show more symptoms ᐯ
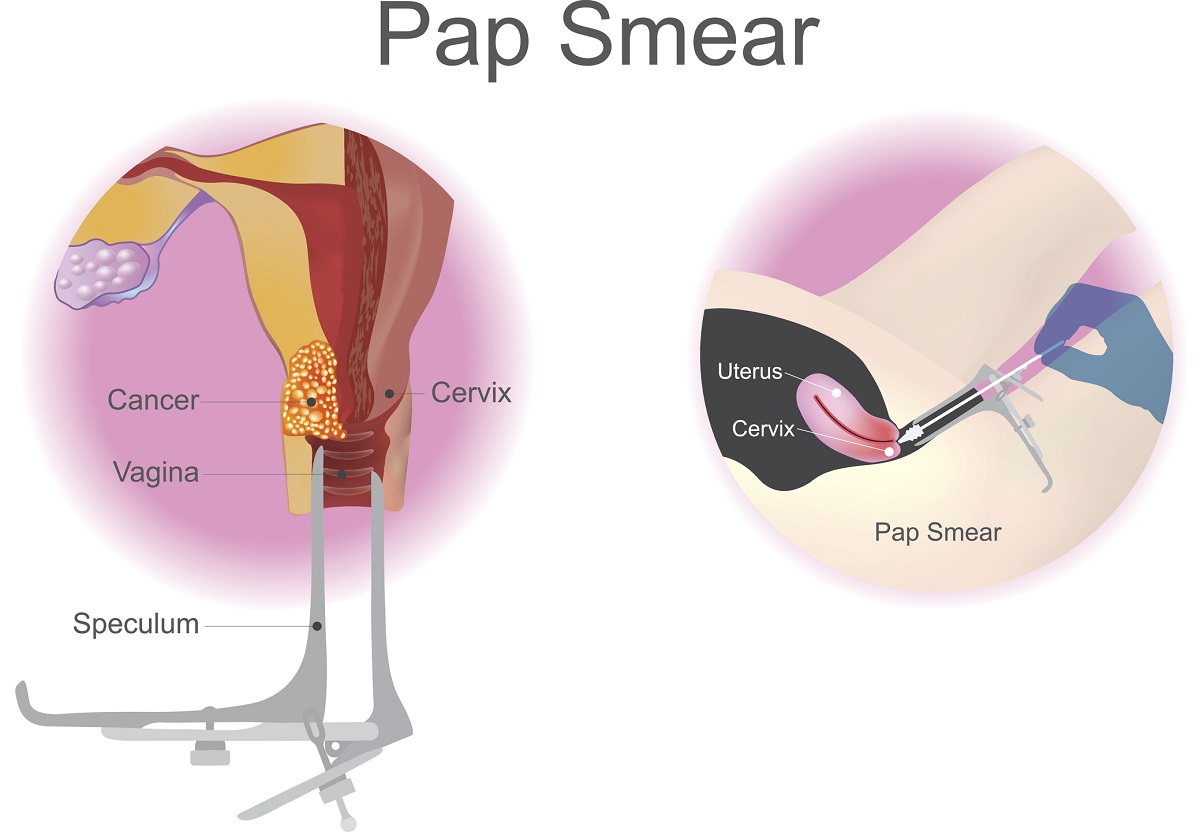
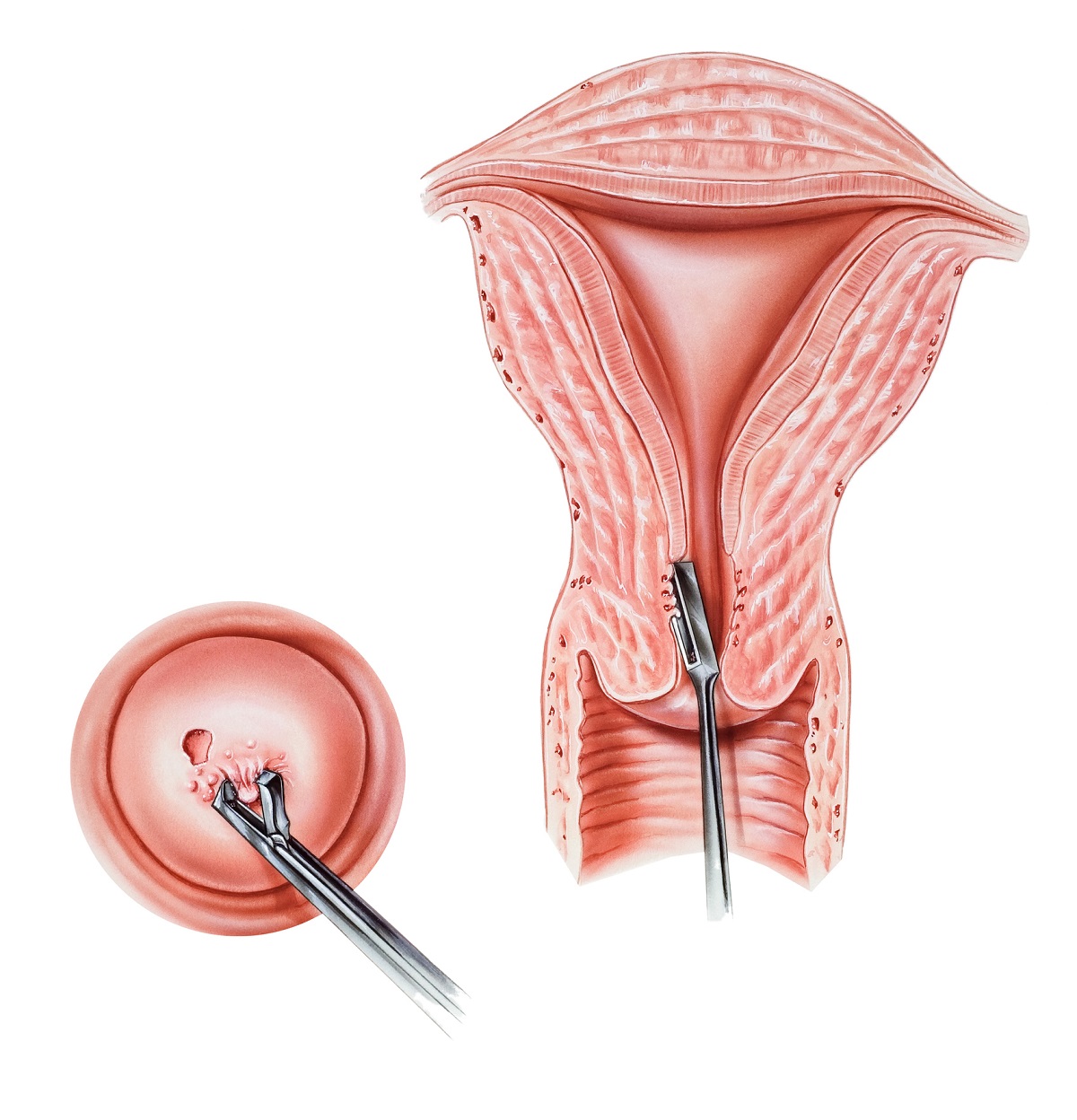
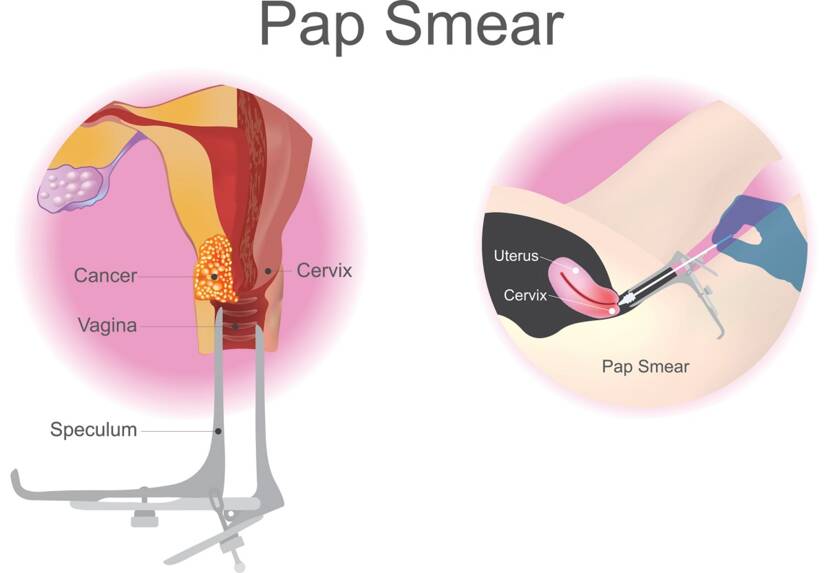
Treatment of cervical cancer: conization chemotherapy and other methods.
Show moreCervical Cancer is treated by
Other names
Rakovina hrdla maternice, karcinóm krčka maternice, karcinóm hrdla maternice, cervikálny karcinóm