- diabetik.sk - information about diabetes
- wikiskripta.eu - determination of glycaemia
- diabeteschart.org - mg/dl to mmol/l conversion
- diabetes.co.uk - Blood Sugar Level Ranges
- my.clevelandclinic.org - Blood Glucose Test
- mayoclinic.org - Diabetes
- who.int - Diabetes
Blood sugar levels: what is normal and what is hyper/hypoglycaemia?

Blood sugar levels, also known professionally as glycaemia, are particularly important for brain function. Neither too much nor too little sugar is good for our bodies.
Article content
What is the ideal or low and high blood sugar level?
Also the glycaemic thresholds and the fasting norm for a healthy person.
Moreover, everything is presented in a clear table.
What should be the correct glycaemia value and what should be considered as an outlier? Useful information is presented in the overview table.
The blood sugar level is technically referred to as glycaemia.
Sugar, or glucose, is important for the whole body, but especially for the brain. Brain cells need it to function properly, just like oxygen.
Glycemia or blood sugar is from the Greek glykys (sweet) and haima (blood). Glyko for relating to sugars and the suffix emia signifies the relationship with blood.
Since glucose is the only energy source, its deficiency causes impaired brain function. Usually, such a condition occurs quickly. It is technically referred to as hypoglycemia, or reduced blood sugar. And it may not occur only in a person with diabetes.
At the other end is the condition of hyperglycemia, excessive blood sugar.
It is mainly associated with diabetes mellitus, or diabetes. But it also occurs in other diseases, such as liver disease, pancreatic disease, endocrine disease, or after certain medications.
Our body gets sugar from food.
So do the other essential components needed to keep it running, such as proteins, fats, minerals, trace elements and vitamins. You can read about them in the magazine article on essential nutrients.
In the body, sugar is stored in the form of glycogen. The largest store is in the liver and muscles.
Glycogen forms the so-called glycogen energy reserve.
Sugar, like other substances in the body, is transported through the blood vessels.
The blood sugar level (glycaemia) is determined by measuring it from the blood. Blood from veins, i.e. venous blood, and capillaries are used for this. Capillaries are tiny blood vessels, a rich tangle of which is found, for example, in the bellies of the fingers.
Blood sugar levels change over the course of the day in a time-dependent manner, with exertion, stress and, of course, after eating. Glycaemic control in the body is provided by several mechanisms, namely the movement of sugar from the blood, i.e. blood plasma, into the cells.
It takes place at the hormonal, autoregulatory and nervous level. The body uses hormones such as glucagon, catecholamines (adrenaline) or thyroxine to increase blood sugar levels. This is of great importance, for example, during a stress reaction, so that sufficient sugar is available for increased consumption.
Conversely, the hormone insulin lowers blood sugar levels.
Insulin is made in the pancreas and is important in moving sugar from the blood into the cells. Without insulin, the cells are unable to take in sugar.
Blood sugar levels are strictly kept within normal limits. Increased or decreased blood sugar levels result in various health problems.
High blood sugar level is referred to as hyperglycemia.
Low blood sugar = hypoglycemia.
What are the glycaemic values?
Proper blood sugar levels are maintained at a certain level and our body tries to keep it within a suitable range with the help of regulation. This is important for adequate functioning of the body, functioning of organs and adequate function of all cells and tissues.
The brain is the most sensitive to the value of glycaemia, as the neurons use glucose as the only source of energy for work.
The table below shows the values of glycaemia
| Name | Glycaemia value in mmol/litre | Description |
| Hypoglycemia | below 2.8 | Low blood sugar sudden onset of difficulty to unconsciousness |
| Standard |
3,3-5,5
| Correct blood sugar levels these reference values reflect fasting blood sugar levels |
| After a meal | less than 8.5 | 1-2 hours after a meal the value may be up to 8.5 mmol/l |
| Borderline value | 5,6-6,9 |
Fasting value need check-up and diagnosis of possible diabetes |
| Hyperglycaemia | above 5.5 |
Elevated glycemic value in non-diabetic, non-diabetic person in diabetic fasting above 6.0 and after eating 7.5 problems occur for a longer period of time |
There is little variation in glycaemic values in the literature and in various publications.
This is also the case when comparing different laboratories that have set their reference values. Glycaemia also varies depending on the type of blood.
Plus...
It depends on whether the blood is taken from a vein, artery or capillary. Similarly, if it is whole blood, plasma or serum.
Read also:
Hypoglycaemia - low blood sugar,
Hyperglycaemia - what to know,
Diet in diabetes - suitable, unsuitable and prohibited foods
How is the sugar level determined?
Different methods are used to accurately determine glycemia, which reflects carbohydrate metabolism. Blood is made up of different components such as red blood cells, white blood cells, platelets. It contains minerals such as sodium, potassium, calcium and also substances such as sugar, proteins or fats, and of course various blood gases.
Fasting glycaemia:
from capillary blood 3.3-6.6
from venous blood 3.9-5.5
in blood plasma 4.2-6.4
The concentration of each component also varies depending on what type of blood is being tested. This can be:
- arterial blood - is blood taken from the arteries
- venous blood - blood coming from veins
- capillary blood - from tiny vascular plexuses where gases and other substances are exchanged
- blood plasma - contains various blood components such as proteins, electrolytes, organic molecules, fibrinogen and coagulation factor
- when it is collected, clotting, i.e. coagulation, is prevented
- blood serum - does not contain cellular elements, its composition is similar to blood plasma, but it does not contain haemocoagulation factor or fibrinogen
- coagulation does not stop during collection
At home or in the laboratory
Glycaemia is accurately determined in laboratory conditions. But it can also be measured in a home environment, in the outpatient clinics of primary care physicians or emergency medical services. A glucometer, which is a blood sugar meter, is used for this purpose.
This device is available to people being treated for diabetes, i.e. diabetes mellitus. A person who has diabetes on a diet or on tablets may not have such a device at home.
People on insulin treatment need to check their blood sugar more often.
Hypoglycaemia sets in quickly, especially if insulin is injected and the person forgets to eat. Another example is accidentally injecting a higher or repeated dose of insulin.
Even if pills are given, hypoglycaemia or hyperglycaemia can occur for various reasons. This happens mainly due to food and dietary error.
Glucometer can be purchased. It is available in different designs and prices.
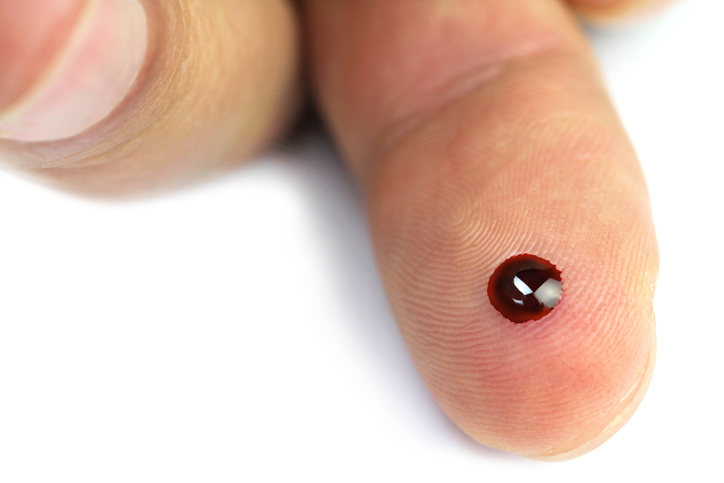
Glycaemia is measured using a glucometer, a test strip and a drop of blood.
The latter is most often obtained from capillary blood vessels, which are found in a rich tangle in the bellies of the fingers, but perhaps also in the earlobe.
The procedure for measuring blood sugar levels at home
How to measure glycaemia and take blood from the finger is given in a short procedure:
- Prepare a glucose meter
- test strip
- the glucometer and the test strip must be from the same manufacturer
- the glucometer must be identical to the type of test strip and the calibration number
- some glucose meters calibrate the test strip automatically
- others need to be manually adjusted
- attention to battery life and energy
- disinfectant
- prepare the needle
- sampling pen with needle
- can also be a conventional needle for drawing blood into a syringe
- insert the test strip into the glucometer
- disinfect the finger
- prick the belly of the finger
- put the pen, lancet or needle in the case
- wipe the spilt blood from the finger
- then squeeze the end of the finger over the belly
- preferably with two fingers just above the puncture and the fingernail
- a drop of blood comes out
- as the glucometer indicates
- catch the drop of blood on the test strip
- After a few seconds, the meter prints out a reading.
- briefly hold and press the swab at the injection site to prevent blood from leaking from the finger
Don't remember the values? Never mind, the calculator will help you:
What is my blood sugar (glycaemia): low, normal or high?
The table below shows the time of the glucose measurement
| Measurement time | Description |
| fasting |
8 hours after eating at diagnosis preventive check-up best in the morning |
| after a meal | Also referred to as postprandial glycaemia 1 hour after food intake monitoring treatment status |
| random |
unrelated to dietary intake as a guide in diagnosis in emergencies to rule out hypoglycaemia and hyperglycaemia |
| glycaemic profile | measure glycaemia more than once during the day before meals may also after meals at night |
Do you know what a glucose meter can show?
The display of a glucose meter may show the current and indicative glucose value. However, sometimes it may show something else. Depending on the manufacturer, there may be a variation of different inscriptions.
The exact description is usually given in the instructions for use.
What the meter can show on the screen, apart from the glucose value in the table
| The meter will display | Description |
| L, LO, LOW, LOW BLOOD SUGAR |
|
| H, HI, HIGH HIGH BLOOD SUGAR |
|
| E, ER, ERROR |
|
Glycaemia units
The resulting value on the glucose meter is displayed in certain units. Most often this is in mmol per litre, which is referred to as mmol/l. Some countries use mg per deciliter, or mg/dl (dcl). What can you do in this case if you need to make a conversion?
Remember the number 18:
When converting from mmol to milligram, multiply by 18
4.0 mmol/l x 18 = 72
When converting from mg to mmol, divide by 18
72 mg/dl : 18 = 4.0

Some important concepts related to glycaemia
The issue of diabetes is complicated. The average person does not need to know everything. However, some terms are good to know. Many terms are used in the text with explanations.
We now list them briefly.
Some terms used in connection with glycaemia or diabetes:
- Hypoglycaemia - low blood sugar.
- Hyperglycaemia - high blood sugar
- Insulin - pancreatic hormone, regulates glycaemia
- Insulin therapy - insulin therapy (administered into the body with an insulin pen, syringe or pump)
- Oral antidiabetic drugs - pills, referred to as PADs and their mechanism depends on the body's own production of insulin
- Glycosuria - sugar in the urine, when glycaemia exceeds 10 mmol/l, which is the renal threshold for glucose
- Glycaemic profile - multiple measurements of glycaemia throughout the day, provides an overview of fluctuations in values
- Type I diabetes mellitus - absolute insulin deficiency, need for insulin therapy
- Type II diabetes mellitus - metabolic disorder, insulin therapy not always required, diet or PAD sufficient
- Gestational diabetes - gestational diabetes
- Hypoglycaemic coma - unconsciousness when blood sugar is low
- Diabetic ketoacidosis - a life-threatening complication of diabetes
- Diabetic neuropathy - impaired nerve function for diabetes
- Diabetic retinopathy - visual impairment due to diabetes
- Diabetic nephropathy - kidney damage from diabetes
- Diabetic foot - ulcers and deformities on the tibia, due to impaired blood supply and infection
About diabetes in brief
Diabetes (diabetes mellitus) is a chronic lifelong metabolic disease characterized by an increase in blood sugar. This increase is due to either a lack of insulin, which is formed in specific cells of the pancreas, or an insufficient effect of insulin (insulin resistance).
Insulin is an important hormone produced by the islets of Langerhans (Β/β Beta cells) of the pancreas.
Insulin = insula (Latin) = island.
Its job is to "transport" sugar from the middle of the blood to the inside of the cell. There the sugar is used as energy.
Converted to ATP during glycolysis - glycos = sugar and lysis = splitting.
Insulin regulates sugar levels in our body by multiple mechanisms and in multiple places. In the liver, in the muscles, even in interaction with fat cells.
Its regulation is based on several processes. The first is blood sugar levels and then the influence of other hormones.
Diabetes is divided into two types
Type 1 diabetes mellitus
The first is type 1 diabetes mellitus. It has an autoimmune basis (the person's immunity attacks the body's own cells) disrupting the function of the pancreas. The consequence is the absence of insulin in the blood.
Insulin has to be delivered artificially into the body. It's done by injection.
This type of diabetes is usually detected in early childhood or during youth.
The cause of its onset is unknown. Genetic influence and inheritance is assumed, but also the experience of certain viral diseases (coxsackie B1, measles, mumps, rotavirus).
Type 2 diabetes mellitus
The second of these is type 2 diabetes mellitus. It used to be referred to as old-age diabetes, as it was mostly detected at an older age rather than in the young.
Nowadays, however, it is also found in people younger than 40 or 30, and even in children.
An inappropriate lifestyle has its effect...
The underlying cause is a lack of insulin production or insulin resistance. This means that insulin does not have sufficient effect and cannot bind to the insulin receptors as needed.
Insulin receptors are found in almost all cells and are needed for the penetration of sugars into the cells.
There are several factors that cause it. In addition to genetics, for example, obesity.
Regardless of the type of diabetes, it is important for a diabetic to follow the principles of a healthy lifestyle, diet and balanced eating, as well as the consistent and precise use of treatment.
Diabetes has its long-term complications anyway. Without controlling proper blood sugar levels and not following the treatment regimen, a person catches up much sooner. He or she is gambling with his or her health and life.
Diabetes is nowadays referred to as a pandemic non-communicable disease as it is one of the fast spreading diseases worldwide.
Let's think... And again we end up with the much talked about lifestyle.
Lack of exercise, stress, unbalanced diets, the prevalence of sugars in the diet, overweight and obesity, and also elevated levels of LDL - bad cholesterol. There is also mention of lack of sleep, exposure to chemicals and toxins.
- Type 2 accounts for approximately 90% of all diabetes
- Which represents approximately 380 million people with type 2 diabetes worldwide.
- Type 2 increases the risk of cardiovascular disease by up to 4 times.
- Up to 90% of all people with type 2 diabetes are overweight and obese
Pregnancy diabetes
Gestational diabetes is also known as gestational diabetes. It has a hormonal basis. Hormones in the placenta reduce the effectiveness of insulin and thus raise blood sugar levels.
Gestational diabetes = gestational diabetes.
In addition, a pregnant woman's pancreas may not be "strong" enough to increase insulin production and respond inadequately to the increased need during pregnancy.
...very simplistically and inaccurately written...
Of course, it doesn't occur in every pregnant woman. But in every pregnant woman, it is advisable and recommended to check blood sugar levels.
It affects approximately 2-3% of pregnant women.
In this case, it's only a temporary condition. It will correct itself after delivery. But there are also cases of ongoing type 2 diabetes.
The risk factors for gestational diabetes are:
- Overweight and obesity before pregnancy
- Family history of diabetes
- Pregnancy diabetes in previous pregnancies
- High blood pressure
- Elevated cholesterol levels
- Polycystic ovary syndrome
- Repeated spontaneous abortions
- Elevated blood sugar levels before pregnancy, so-called prediabetes
- Lack of exercise
- Excessive stress
Health complications of diabetes
That blood sugar levels are important for brain function is already obvious. Without sugar, the brain does not work and sudden neurological problems are the result. For example, speech impairment, mobility problems appear, a person may outwardly give the impression of drunkenness, disorientation, behavioural changes and even unconsciousness.
These problems arise quite acutely and can be managed just as quickly.
However, pathological deviation of glycaemia also creates long-term or chronic problems.
Hyperglycaemia damages blood vessels, nerves, kidneys and eyes. High blood sugar, excess fat and high blood pressure are the basis for atherosclerosis and subsequently for serious diseases such as coronary heart disease or acute myocardial infarction.
Interesting information in the following articles:
Diabetes and its complications
Coronary heart disease
Myocardial infarction
Untreated or even undertreated diabetes causes damage to blood vessels. As a result, diabetic foot, various skin defects, ulcerations or boils, and even necrosis develop. And not only on the foot, but also in other parts of the body. And various infections are more common in diabetes.
And so much for diabetes in a nutshell.
Ako sa meria glykémia
Interesting resources
Related










