- wikiskripta.cz - Endometriosis
- solen.cz - Endometriosis: significant impact on a woman's quality of life
- reprogenesis.sk - Endometriosis
- medixa.sk - Intracytoplasmic sperm injection - ICSI
How are endometriosis and infertility related + Other symptoms and health problems
Not much is known about endometriosis, but it still has a significant impact on a woman's life. The causes, manifestations and treatment of this gynaecological disease are highly individual. It can have a significant impact on fertility, changing future prospects for planned pregnancy and parenthood.
Article content
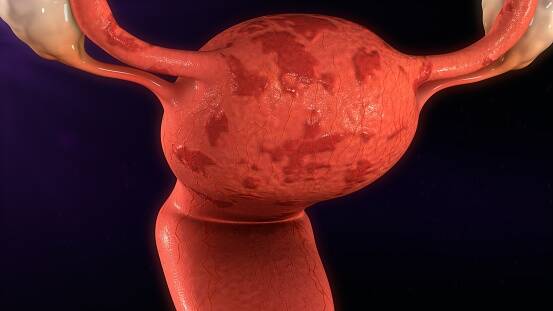
Endometriosis is a female disease considered a type of benign tumor (non-malignant cancer). More specifically, it is a chronic, systemic estrogen-dependent inflammatory disease.
It affects 5 to 15% of the female population. Female patients of childbearing age predominate, but women and girls of any age group can become ill.
Interesting:
Endometriosis in adolescent females was first described in 1929.
The youngest known patient with this disease to date is a preschool girl.
Endometriosis has even been reported in patients with Künster's syndrome, which is characterized by the absence of the endometrium and sterility.
Interestingly, it has been reported in men with prostate cancer treated with estrogens.
The impact of endometriosis on a woman's quality of life
Endometriosis may initially present as a mild, asymptomatic form of the disease. At this stage, the patient has no problems and so may not even be aware of her disease. She usually learns of her diagnosis from a gynaecological examination.
The moderate forms cause mainly pain in the lower abdomen and pelvic area and usually radiate to the abdomen or sacral region up to the rectum.
The pain is more intense during menstruation and intercourse and can therefore be a problem in a healthy sex life. Painful intercourse on the part of the woman causes rejection of the partner. In some cases it leads to estrangement.
In the most severe cases, the pain is so severe that it limits the patient's normal activities. She is unable to function normally without the use of pain-relieving medication.
In addition to pain, inflammatory changes occur in the woman's body and scarring of the tissue to such an extent that it can lead to infertility. Endometriosis can even be considered a common cause of infertility.
What is endometriosis and why does it occur?
Endometriosis is a disease characterized by the appearance of functional and ectopic endometrium (glands and stroma) outside its typical localization in the uterus.
Uterine mucosal deposits have been described everywhere except in the heart and spleen. They are most commonly found in the peritoneum (the membrane lining the abdominal cavity), on the ovaries and fallopian tubes, and in the rectovaginal septum (the septum between the vagina and rectum).
The endometrial lining is 'functional' outside the uterus. It responds to hormonal changes in the plasma and therefore undergoes regular cyclical changes. Sporadically, the deposits are composed of 'false tissue' (non-functional).
The endometrial deposits are initially made up of small pale papules which change colour to red and later brown to black deposits. As the disease progresses, the tissue at the site of the endometrial pathology becomes damaged, scarred and then shrinks.
In the final stage, a condition called frozen pelvis occurs. The atypical deposits have their own vascular supply and cause the Douglas space (the space between the uterus and the anus) to disappear.
The basic theory of endometriosis
The causes of endometriosis are multifactorial (genetics, hormones, infections, trauma, surgery...). However, there are several theories.
- The implantation theory (the so-called Sampson theory) holds that during the menstrual cycle, retrograde (reverse) bleeding occurs. The endometrial cells enter the peritoneal cavity through the fallopian tubes, where they are subsequently implanted.
- The metaplastic theory (called Meyer's theory) refers to the ability of the peritoneal mesothelium (peritoneal cell lining) to transform into endometrial tissue (tissue typical of the uterine lining). This process is also called metaplastic transformation.
- The induction theory (called the Müllerian theory) assumes that during the development of the Müllerian duct, residual cells remain in the tissues of the small pelvis. In some situations, induction (formation and transformation) into functional endometrial tissue may occur.
- The immunoalteration theory (the so-called Dmovsky theory) links the development of endometriosis to the mechanisms of cellular immunity. More and more experts are leaning towards this theory. The theory points to functional changes in the cells of the immune system. These cells normally recognise and destroy implanted endometrial cells. When they are disrupted, the destruction does not occur and endometriosis develops.
- The luteinized, unruptured follicle theory is based on the fact that there is no rupture of the luteinized follicle. Therefore, there is a decrease in the concentration of estrogen and progesterone in the abdominal cavity. The decreased concentration of these hormones increases the risk of endometrial implantation in this part.
- The transport theory explains the formation of endometriosis by a transport pathway using blood and lymphatic cells. This theory arose because the occurrence of endometrium in more distant organs, such as the lungs, could not be explained by previous theories.
Risk factors for the development of the disease
There are a number of risk factors that could theoretically influence the development of endometriosis. These factors are not to be taken lightly. If you experience any of them, you need to beware.
Risk factors for endometriosis include:
- genetic predisposition (family history is common)
- women of childbearing age (20-45 years)
- race (Japanese women have the highest incidence, followed by Caucasian women, and black women have the lowest incidence)
- short menstrual cycle (cycle less than 27 days)
- menstrual cycle disorders (hypermenorrhoea, dysmenorrhoea)
- gynaecological diseases (cysts, polycystic ovary syndrome)
- other diseases
- gynaecological procedures (medical procedure, surgery involving the endometrial glands outside the uterus)
- infertility (common in women who deliberately delay pregnancy or who are infertile)
- medication (mainly estrogen treatment)
- trauma mechanism (abdominal and pelvic trauma with damage to the peritoneum)
- psychological trauma (stress, psychological trauma, mainly of a sexual nature - abuse)
What are the symptoms of endometriosis?
Women in the early stages of endometriosis may not show any signs of the disease. However, pelvic pain and prolonged problems getting pregnant are typically considered to be its symptoms.
However, symptoms are highly individual and can vary depending on the location of the endometrial deposits, their size, extent and also the stage of the disease. This often leads to misdiagnosis.
Table with the stages of endometriosis:
| Stage I. | Stage I. Lighter degree of severity |
|
| Stage II. | moderate degree of severity |
|
| Stage III. | moderate severity |
|
| Stage IV. | severe severity |
|
Manifestations typical of endometriosis
Asymptomatic does not automatically imply that the patient has a mild form of the disease.
In asymptomatic patients, extensive ectopic endometrial findings were often found. In contrast, in patients with severe manifestations, the findings were minimal.
This is because several mechanisms are involved in the onset of pain (the influence of prostaglandins, oppression and ischemia of surrounding tissues and nerve endings).
Manifestations of endometriosis:
- chronic pain in the lower abdomen
- chronic pelvic pain in 50-60 % of cases
- chronic pain in the sacral region
- chronic pain in the sacral region
- discomfort in the rectal area, even pain shooting into the rectum
- frequent urge to urinate (pollakiuria)
- disturbance of the intestinal passage, subileosis
- in 50-90 % of cases, intense menstrual pain(dysmenorrhoea)
- pain during sexual intercourse(dyspareunia)
- disorder of ovulation and menstruation
- problems with conception, infertility
- infertility (inability to bear a fetus, repeated miscarriages)
Why and when is endometriosis a cause of infertility?
Endometriosis is a relatively common cause of infertility in women. However, assessing the direct relationship between endometriosis and infertility is quite complex. Other possible causes must also be taken into account.
Nevertheless, it is true that up to 50% of women with this condition have problems getting pregnant.
The reason for infertility in patients with endometriosis is usually due to inflammation, which leaves behind scar tissue in the fallopian tubes and causes hormonal imbalances. Scarring and post-inflammatory adhesions can lead to fallopian tube obstruction.
Infertility can also occur due to ovulation disorders, impaired function of the corpus luteum or due to the adhesive process (wear and tear).
The inflammatory process around the implanted endometrial cells has a toxic effect on the gametes and the embryo, creating unsuitable conditions for attachment and survival.
The most common influences on infertility in patients with endometriosis:
- Immunological influences - Increased production of anti-endometrial antibodies interferes with the fertilization process, resulting in altered cellular and humoral components of immunity.
- Biochemical influences - High levels of prostaglandins cause disturbances in the motility of the fallopian tube, resulting in its narrowing and even complete obstruction. They also affect luteal dysfunction (premature disappearance of the corpus luteum) and also impair egg attachment and transport.
- Endocrinological influences - Hormonal influences on infertility are varied. These include luteal insufficiency, smaller follicle growth, smaller follicle size, anovulatory cycles, absence of Graaf's follicle rupture.
What are the treatment options for infertility in a patient with endometriosis?
Not every patient with endometriosis is automatically infertile. However, it does occur at a high rate (up to 50%).
Infertility caused by this insidious disease is treated in two ways, surgically and by assisted reproductive techniques.
For endometriosis in stages I and II of the disease, surgical treatment is recommended for infertility, namely ablation (separation) of endometrial deposits and adhesiolysis (breaking of adhesions). This is a relatively effective treatment that increases a woman's chances of becoming pregnant. This procedure is not recommended for higher stages of the disease, or its effectiveness decreases significantly.
Assisted reproductive techniques are quite popular and are sought after by many infertile women. These are intrauterine insemination (in vitro fertilization). This method is effective in many cases. It significantly increases the chance of pregnancy and therefore the number of births.
- IVM method - With the help of this method, immature eggs are taken directly from the ovaries and matured outside the woman's body. Maturation takes place in embryo laboratories, in a special solution for proper embryo development. The whole process takes 24 to 48 hours. The matured egg is thus prepared for fertilization with male sperm. Fertilization is carried out with the help of a micropipette, with which the sperm is introduced directly into the egg. This procedure is called intracytoplasmic sperm injection. In this method, the drugs needed for stimulation are used minimally.
- IUI method - It is the simplest method of assisted reproduction. Sperm is inserted directly into the uterus of the patient with the help of a transfer catheter. The procedure is done during ovulation and after prior hormonal preparation, which increases the chances of getting pregnant and carrying the fetus.
Interesting resources










