- solen.cz - Vitiligo: diagnosis and treatment
- solen.sk - Vitiligo phototherapy
- prolekare.cz - Vitiligo treatment in practice
- solen.sk - Autoimmune skin diseases I. Vitiligo, alopecia areata, psoriasis
- prolekare.cz - Overview of surgical treatment of vitiligo
- solen.cz - Pigmentation disorders - melasma and its treatment
- mayoclinic.org - Vitiligo
Vitiligo: What is vitiligo and what are its causes and symptoms? When does it start?

Vitiligo is called by some the disease of white spots. Let's look at the causes of this disease and treatment options.
Characteristics
Vitiligo was first described in antiquity. The origin of the name of the disease is not entirely clear. Various meanings come to mind, e.g. vitium = defect, vitellus = mottled flesh, vito = to protect oneself.
Vitiligo is defined as an acquired depigmentation (loss of pigment) of the skin. It results from the death of melanocytes. It is important to note that vitiligo is not an infectious disease.
Vitiligo affects approximately 1 to 2% of the world's population. It can occur at any age of life. It is most common between the ages of 10 and 30. Vitiligo affects both sexes equally. A positive family history is found in 30 to 40% of cases.
The disease affects people worldwide regardless of race, gender or age. The incidence of vitiligo is slightly higher in darker skin types.
For example, a scientific study conducted in China showed that the prevalence of the disease was only 0.093%. While in areas of India, the prevalence of the disease was 8.8%.
Did you know that....
Michael Jackson also suffered from vitiligo. Among the living celebrities, comedian Steve Martin, whom you know from the movies Pink Panther and Somehow It Gets Complicated, also has vitiligo.
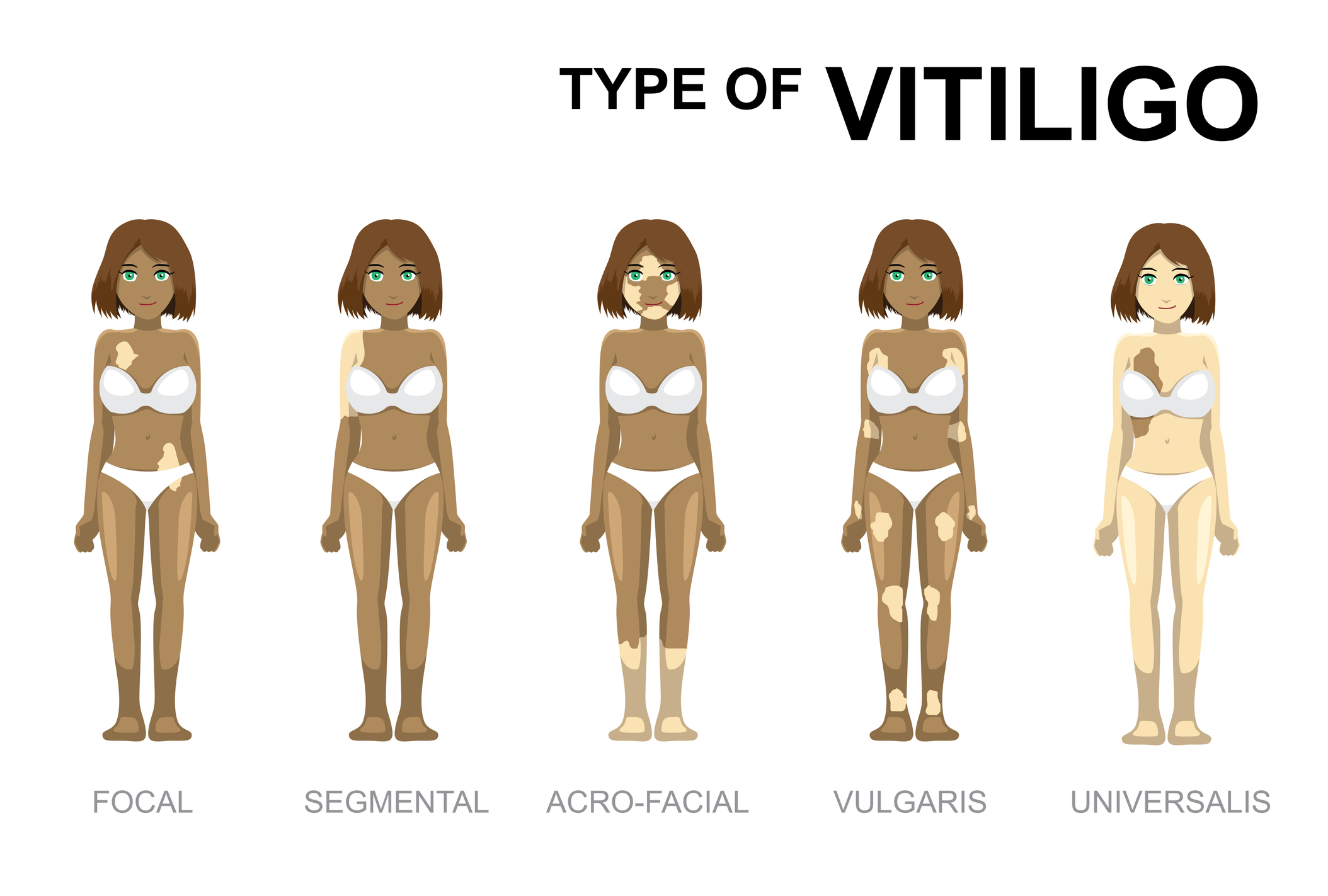
Vitiligo is divided into the following types:
- Localized vitiligo:
- Focal - One or more foci of vitiligo. It can appear anywhere on the body.
- Segmental - One or more vitiligo deposits. It affects only a specific localized area.
- Generalized vitiligo:
- Acrofacial - Numerous vitiligo deposits. Occurs mainly on the face and distal (peripheral) parts of the extremities.
- Vulgaris - Occurs on more extensive areas of the body.
- Vitiligo universalis - Characterised by complete or almost complete loss of skin pigment (80-90% of the body surface).
- It is usually preceded by generalised vitiligo, which gradually progresses to complete or almost complete loss of skin and hair pigment.
Vitiligo is not considered to be a serious health problem. It is essentially a cosmetic defect. Vitiligo can cause psychological problems in some patients, especially women.
People who have darker skin may perceive the loss of pigment as a cosmetically disturbing problem. This is especially true if the loss of pigment appears on the face, hands or feet.
Causes
The causes of the disease are unknown. 3 theories of vitiligo are considered:
- The autoimmune hypothesis
Impaired immune control leads to the production of cytotoxic antibodies against melanocyte antigens. This leads to the destruction of the cell. Simply put, our immune system thinks that melanocytes are foreign cells to the body. It therefore tries to destroy them.
- The neutral hypothesis
Melanocytes are destroyed by substances involved in signal transmission between nerve cells.
- The self-destruction hypothesis
An intercellular toxic metabolite of melanin synthesis destroys melanocytes. This occurs when the cell cycle is disrupted under oxidative stress.
What are the triggering factors?
The mediating triggering factors include mainly stressful situations (death in the family, serious illness, accident). The importance of these factors is difficult to verify in practice. Vitiligo has also been observed as Koebner phenomenon at the site of local injury.
What is Koebner's phenomenon?
In some skin diseases, new lesions form after physical, chemical or mechanical irritation. Koebner's phenomenon can be observed in psoriasis or vitiligo.
What is melanin?
Melanin is a skin pigment that determines the colour of the skin. It has a photoprotective effect. The formation of melanin (called melanogenesis) takes place in melanocytes. Melanocytes are located between the cells of the lowest (basal) layer of the skin.
Melanin is stored in melanosomes.
Diseases that are associated with vitiligo include:
- thyroid disorders (35%)
- alopecia areata (16 %)
- anaemia (8 %)
- diabetes mellitus (7 %)
- eye diseases (5 %)
- Addison's disease (2%)
- myasthenia gravis
- Crohn's disease
- lupus erythematosus
- systemic scleroderma
- biliary cirrhosis
See also:
Did you know...
Vitiligo very often occurs incidentally in patients with malignant melanoma.
Symptoms
Approximately 50% of vitiligo sufferers develop the disease by the age of 20. The main clinical manifestation of vitiligo is the loss of pigment in the skin and hair follicles. The loss of pigment results in white, sharply demarcated foci which may gradually enlarge.
Vitiligo occurs mainly in areas that are normally hyperpigmented:
- Face
- head
- hands
- armpits
- groin area
- anogenital area
On the limbs, it occurs mainly on the elbows, knees and wrists. Occasionally, vitiligo also appears on the hairy part of the head. Light strands of hair (polyosis) grow from the affected area.
The symptoms of vitiligo are more pronounced in people with darker skin. In people with lighter skin, the symptoms of vitiligo become more pronounced when they sunbathe.

Diagnostics
Vitiligo can be easily diagnosed by clinical signs in most cases.
In case of doubt, the Wood's lamp is used in practice. This lamp shows different shades on the skin. Based on these shades, we can diagnose certain skin diseases. If the patient suffers from vitiligo, we observe a bluish colour on the skin.
The following table describes the steps in the diagnosis of vitiligo
| 1. Family and personal history |
|
| 2. Pharmacological and occupational history |
|
| 3. Objective findings |
|
| 4. Laboratory examination |
|
When diagnosing vitiligo, we must also rule out other diseases that cause hypopigmentation and depigmentation.
The differential diagnosis of vitiligo includes the following diseases:
- albinism
- pityriasis versicolor
- pityriasis alba
- hypomelanosis guttata
Read also:
Course
Vitiligo is a chronic disease. The course of the disease varies from person to person. In most cases, vitiligo is progressive. In the case of highly active vitiligo, complete loss of pigment (vitiligo fulminans) can occur within six months.
In patients suffering from atopy, the course of vitiligo is unfavourable. Complete spontaneous disappearance of symptoms is rare. During the summer months, there may be a partial alleviation of symptoms.
How it is treated: Vitiligo - depigmentation / loss of skin pigment
Treatment of vitiligo: Topical - ointments, light, drugs and other forms
Show moreVitiligo is treated by
Other names
Interesting resources
Related










