- solen.sk - TUBERCULOSIS AT THE BEGINNING OF THE 21ST CENTURY - PRACTICAL PERSPECTIVE, Ivan Solovič, Institute of Tuberculosis and Lung Diseases and Thoracic Surgery, Vyšné Hágy
- solen.sk - Tuberculosis - still a topical problem, Doc. MUDr. Ivan Solovič, CSc. from the National Institute of Tuberculosis and Lung Diseases and Thoracic Surgery, Vyšné Hágy, Faculty of Health of the Catholic University of Ružomberok.
- Standard procedure.
- ncbi.nlm.nih.gov - Tuberculosis, Rotimi Adigun, Rahulkumar Singh
- pubmed.ncbi.nlm.nih.gov - Steps to the discovery of Mycobacterium tuberculosis by Robert Koch, 1882, E. Cambau, M. Drancourt
- clinicalmicrobiologyandinfection.com - From antiquity to the discovery of the tubercle bacillus.
Tuberculosis of the lungs: what are the symptoms, causes and contagiousness of TB?

Tuberculosis is one of the most feared infectious diseases. It mainly affects the lungs. How does it manifest itself? What are its causes? What is the contagiousness of tuberculosis and how is it transmitted?
Most common symptoms
- Malaise
- Chest pain
- Increased body temperature
- Spirituality
- Blue leather
- Sweating
- Indigestion
- Dry cough
- Fatigue
- Damp cough
- Coughing up mucus
- Coughing up blood
Characteristics
"If the importance of a disease were measured by the number of victims, even the most dreaded infectious diseases, such as plague and cholera, would remain far behind tuberculosis" Robert Koch, 24 March 1882.
Of the extrapulmonary organs, it most commonly affects the pleura, lymph nodes, central nervous system, bones, joints, urinary tract, gastrointestinal system, or skin.
A major problem today is the increasing incidence of resistant forms of TB. The bacteria can resist even the most bactericidal antituberculosis drugs in their numerous combinations.
The treatment of tuberculosis is very specific and challenging.
It requires expert supervision, adherence to a strict dosage regimen and a treatment schedule with effective antituberculosis drugs.
Characteristics of tuberculosis
Tuberculosis (TB) is an infectious bacterial disease caused by Mycobacterium tuberculosis.
Paleomicrobiology was responsible for the discovery of the causative agent of tuberculosis.
It is the science that deals with the analysis of dead organisms. The causative agents of tuberculosis have been discovered on animal and human skeletons thousands of years old.
The most famous scientist associated with this discovery is the German physician Robert Koch.
But he was not alone in this discovery. He was helped by the earlier scientific work of the French physician Jean-Antoine Villemine. It was he who discovered that tuberculosis was a contagious disease. He devised a new microbiological staining procedure and a new culture procedure.
Thanks to these new findings, Robert Koch was able to announce to the Berlin Physiological Society on 24 March 1882 that he had discovered the microorganism that causes the deadly and dreaded tuberculosis. He then called this new microorganism the "tuberculovirus".
It was not until 1883 that the bacterium was given its current name, Mycobacterium tuberculosis.
The disease mainly affects the lungs, but extrapulmonary disease is also common.
The most common forms of pulmonary tuberculosis
- Infiltrative pulmonary TB is characterised by inflammatory pulmonary infiltrates that form numerous effusions and tend to caseify rapidly. They affect any part of the lungs.
- Tuberculoma falls under the infiltrative form. On chest X-ray it appears as a solitary, round and sharply demarcated mass. Its centre may be collapsed, i.e. caseated.
- Cavernous tuberculosis of the lung (disseminated) is a very severe form of tuberculosis that arises from the pulmonary infiltrate by disintegration (necrosis) of the caseous tuberculoma. The patient subsequently coughs up the necrotic mass.
- Nodular TB of the lung often presents asymptomatically or with a very poor clinical picture. Numerous nodules are found in the lungs.
- Tuberculous pneumonia is an acutely progressive form of TB. It is characterised by the rapid onset of severe symptoms such as fever, rigors, dyspnoea and cough with expectoration of sputum. The sputum is purulent and contains large numbers of mycobacteria.
- Miliary TB of the lung is characterised by the formation of small nodules up to 1 mm in size. It spreads by haematogenous spread (blood) to other organs throughout the body. The result is a generalised form of the disease. The disease can vary from mild subfebrile to dramatic with predominantly respiratory distress. It can also present as sepsis with tachycardia, hypotension and hepatosplenomegaly (Landouzy sepsis).
Extrapulmonary tuberculosis
The extrapulmonary form of tuberculosis is relatively rarer. However, it can affect any organ or tissue.
It usually arises by haematogenous spread (blood) of mycobacteria from a primary site that is localised in the lungs.
- Tuberculous pleurisy - One of the most common extrapulmonary TB.
- Tuberculous lymphadenitis - This is an involvement of the lymph nodes, usually cervical, which are painlessly swollen.
- TB of the bones and joints - The spine is most commonly affected, the disease is called spondylitis tuberculosa - Pott's disease. The vertebrae and intervertebral discs are affected.
- TB of the central nervous system - A life-threatening form of the disease. Tuberculous meningitis (basilar) occurs with the manifestations of miliary TB.
- TB of the urogenital system - Affects the kidneys, ureter and bladder.
- TB salpingitis - May cause infertility in women.
- TB of the gastrointestinal system - Affects the intestines, abdominal lymph nodes or peritoneum. Symptoms include abdominal pain, abdominal discharge and weight loss.
- TB of the skin - Manifested by the formation of ulcers or nodules.
- TB of the sensory organs - The eye and its components may be affected, but also the ear when destructive inflammation of the middle and inner ear is present.
In the last few decades, a concerted global effort has succeeded in partially eradicating TB.
In 2017, the World Health Organization (WHO) estimated that the global incidence of tuberculosis is declining by 1.5% per year.
The number of deaths from the disease has also declined significantly. From 2000 to 2015, the number of deaths from TB decreased by 22%.
Causes
Other members of this group include e.g:
- Mycobacterium africanum
- Mycobacterium bovis
- Mycobacterium microti
Most of these other named microorganisms are classified as non-tuberculous or as so-called atypical mycobacteria.
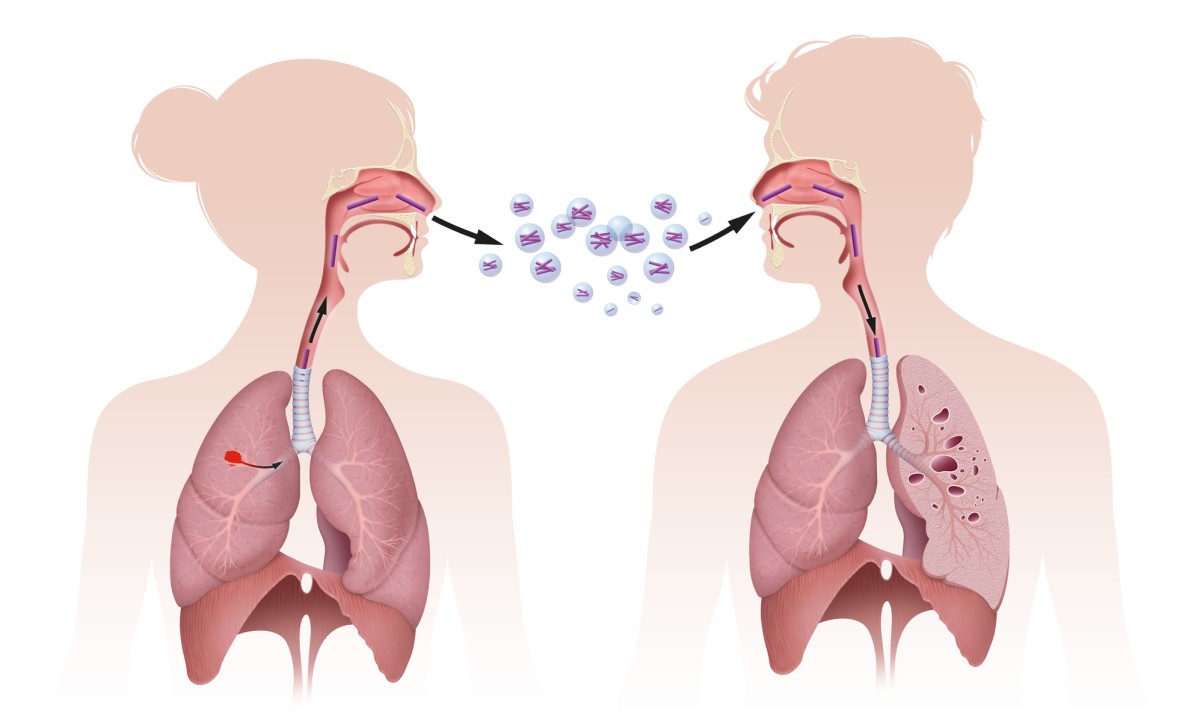
Humans can become infected in several ways:
- by inhalation
- dry route - inhalation of infected dust
- the wet route - so-called droplet infection, this is the inhalation of aerosol droplets containing the bacteria
- by inoculation - direct contact with bacteria that enter the bloodstream through broken skin or mucous membranes, e.g. by health care workers, surgeons, pathologists, etc.
- alimentary route - infection from contaminated food in widespread bovine TB, via unpasteurised and uncooked milk and dairy products
M. tuberculosis is a highly transmissible bacterium.
There is a group of people who are significantly more susceptible to this infection. This includes patients who are exposed to the main risk factors for infection. These are mainly those who have reduced cellular immunity and are therefore immunosuppressed.
Major risk factors include:
- Socio-economic factors such as poverty, lack of access to health care, low levels of hygiene, malnutrition and war, associated with population migration and global shortages.
- Immunosuppressed patients, e.g. HIV positive or AIDS patients, chronic and prolonged immunosuppressive treatment, e.g. corticosteroids, monoclonal antibodies to tumour necrosis factor, poorly developed immune systems in premature infants, newborns or persons with primary congenital immunodeficiency.
- Occupations at risk, e.g. miners, construction workers (risk of pneumoconiosis and silicosis), but also health and social workers who are more likely to encounter potential carriers of the disease.
More recently discovered risk factors include the use of a monoclonal antibody. It is directed against an inflammatory cytokine called tumour necrosis factor alpha (TNF-alpha). These monoclonal antibodies are used to treat autoimmune inflammatory diseases. This treatment is also known as biological therapy.
Examples of these agents include drugs:
- infliximab
- adalimumab
- etanercept
- golimumab
Diseases treated with these monoclonal antibodies include, for example, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis (so-called Bechterew's disease), psoriasis, Crohn's disease, ulcerative colitis, non-infectious uveitis and hidradenitis suppurativa.
Patients taking any of these drugs should be screened for the presence of latent TB before treatment. They should be monitored regularly during treatment for reactivation of the disease.
The body can effectively prevent the spread of TB infection in the body. However, this ability is influenced by a person's immune status, genetic factors and whether the exposure is primary or secondary.
Well-developed so-called M. tuberculosis virulence factors make it difficult for immune cells, especially alveolar macrophages, to fight the pathogen.
The most important virulence factor is the high content of mycolic acid in the outer envelope of the bacterium. Such a protective barrier makes phagocytosis, i.e. the ingestion of the bacterium by immune cells (alveolar macrophages), more difficult.
Multidrug-resistant tuberculosis (MDR-TB) and extremely multidrug-resistant tuberculosis (XDR-TB)
There are two 'exceptional' strains of M. tuberculosis that pose an extremely high risk to the patient. This is mainly due to their resistance to commonly available and proven antituberculosis drugs.
MDR-TB
This is a form of tuberculosis caused by strains of mycobacteria that have developed resistance or immunity to common antituberculosis drugs.
This tuberculosis is a particular problem in the HIV/AIDS population.
A form of MDR-TB is diagnosed when resistance to multiple antituberculosis drugs is demonstrated, including at least two standard antituberculosis drugs, which are rifampicin or isoniazid.
Most cases of MDR-TB are so-called primary MDR-TB, which is directly caused by infection with resistant pathogens.
However, approximately 25% of patients have an acquired form of MDR-TB.
This occurs when a patient becomes infected with the common M. tuberculosis but develops resistance to the bacterium during the course of treatment for tuberculosis.
The reason for the emergence of such acquired resistance in the host is inappropriate treatment of tuberculosis, improper use of antibiotics, inadequate dosage and failure to allow sufficient time for cure and subsequent return to treatment.
XDR-TB
This is the most serious and dangerous type of MDR-TB ever.
Such M. tuberculosis bacteria are resistant to at least four antituberculosis drugs. This includes resistance to rifampicin, isoniazid and resistance to any two modern antituberculosis drugs.
Modern antituberculosis drugs are fluoroquinolones (levofloxacin and moxifloxacin) and second-line injectable aminoglycosides (kanamycin, capreomycin and amikacin).
The cause of XDR-TB is similar to that of MDR-TB, but the occurrence of XDR-TB is much rarer.
Antibiotic resistance: why take them exactly and as prescribed by your doctor?
Symptoms
Symptoms at the onset of infection include:
- increased fatigue
- malaise, fatigue
- weight loss
- slightly raised temperature
- night sweats
- pallor in the face
- cough, which is dry at first, later becoming wet with expectoration (coughing up) of mucoid sputum, may also be admixed with blood
Symptoms of more advanced disease include:
- subjective sensation of shortness of breath and shortness of breath, often occurring in combination with pleural effusion
- chest pain occurs when the pleura is affected
- chronic cough with coughing up large amounts of blood (haemoptysis)
- marked weight loss and wasting of the whole body
Diagnostics
- we start with a thorough history of the patient
- an expert assessment of the epidemiological situation, the patient's background, nationality, occupation, etc. is important.
- physical examination, which includes in particular an examination of the respiratory tract, skin, nervous system, etc.
- imaging examinations, especially posterior X-ray lung or CT scan, are very useful in the diagnosis of TB
- microbiological examination of biological material, e.g. sputum or urine
- endoscopic examination (bronchoscopy)
- histological examination of a biological sample of tissue affected by TB
- screening tests
Screening tests
The most commonly used TB screening tests include:
1. tuberculin skin tests, the Mantoux test.
The test provides information about the patient's exposure to tuberculosis.
It is performed by injecting a PPD (purified protein derivative) into the patient's skin. The skin reaction, which is the swelling (induction) of the injection site above the skin level, is observed. The size of the 'pimple' is measured. A mere redness is not considered a significant reaction.
Based on this skin reaction, the test is evaluated.
The result is interpreted with respect to the patient's overall risk of exposure.
Patients are divided into 3 groups:
- Low risk patients - Those with minimal risk of exposure are considered positive for the Mantoux test only if the size of the swelling is 15 mm or more.
- Intermediate risk patients - If a person has some likelihood of exposure, their test is considered positive if the size of the induration is greater than 10 mm.
- High risk - Patients with a high probability are e.g. HIV positive patients, patients with known previous TB or known contact with a patient with a chronic cough. For this group of persons, the Mantoux test is considered positive if the size of the induration is greater than 5 mm.
The Mantoux test provides information on exposure or latent TB. The test does not have sufficient specificity. Therefore, patients should undergo other investigations such as chest X-ray and repeated check-ups with a physician. In addition, the test may give false positive results in persons who have been exposed to the BCG vaccine.
2. Interferon release tests (Quantiferon test)
This is a TB screening test similar to the Mantoux test. It has the advantage of higher specificity while maintaining the same sensitivity as the Mantoux test.
The principle of this test is to test the level of inflammatory cytokines, especially interferon gamma.
Another advantage is the way in which the test is performed. The Quatiferon test requires only one blood draw. This means that the patient is not traumatised by additional visits to the doctor, especially if other diseases, such as HIV, need to be tested from the blood (with the patient's consent).
The test is more expensive than Mantoux. It also requires more technical expertise to perform.
Screening for immunocompromised patients is different because their immunity responds differently to the tests.
In immunocompromised patients, the Mantoux test may be a false negative due to skin anergy, i.e. a reduced immune response. Therefore, the Quantiferon reaction is preferable in these patients.
The importance of screening testing
A positive screening test result means that the patient has been in contact with tuberculosis, i.e. has been exposed to the disease. Such a patient has a high probability of developing active tuberculosis in the near future.
A patient with a positive test has a 2% to 10% risk of developing active disease without treatment.
At the same time, such a person should undergo lung imaging, at least a chest X-ray. Patients at risk of latent tuberculosis should be treated prophylactically with isoniazid.
Course
Primary tuberculosis is a form of the disease in which tuberculous deposits, known as a GHO infarction, form in the central part of the lungs. This tuberculous deposit and the adjacent lymph nodes also affected by tuberculosis form the GHO complex.
In most infected persons, the Ghon complex goes into a state of latency. This means that the disease is inactive for years. This state is called latent tuberculosis.
Latent tuberculosis can reactivate, especially after immunosuppression of the host.
A small percentage of infected persons will develop active disease immediately after first exposure. This form is called primary progressive tuberculosis. Primary progressive tuberculosis is particularly common in children, malnourished persons, immunosuppressed patients and persons who have been taking corticosteroids for a long time.
In most people, tuberculosis develops after a long latency period.
Latent tuberculosis may last for several years after the initial primary infection. This form is called secondary tuberculosis.
Secondary tuberculosis is a reactivated latent tuberculosis infection. The lesions of secondary tuberculosis, unlike primary tuberculosis, are located in the apices of the lungs.
Some persons with secondary tuberculosis have become re-infected with M. tuberculosis, i.e. have been re-infected.
How it is treated: Tuberculosis of the lungs - TB
Treatment of tuberculosis: how to treat, what drugs are effective? ATB and other principles
Show moreTuberculosis of the lungs is treated by
Other names
Interesting resources
Related










