- Wanderås MH, Moum BA, Høivik ML, Hovde Ø (May 2016). "Predictive factors for a severe clinical course in ulcerative colitis: Results from population-based studies". World Journal of Gastrointestinal Pharmacology and Therapeutics. 7 (2): 235–241. doi:10.4292/wjgpt.v7.i2.235. PMC 4848246. PMID 27158539.
- Runge MS, Greganti MA (2008). Netter's Internal Medicine E-Book. Elsevier Health Sciences. p. 428. ISBN 9781437727722.
- Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, et al. (January 2012). "Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review". Gastroenterology. 142 (1): 46–54.e42, quiz e30. doi:10.1053/j.gastro.2011.10.001. PMID 22001864.
- Wang, Haidong; et al. (GBD 2015 Mortality and Causes of Death Collaborators) (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- Ford AC, Moayyedi P, Hanauer SB (February 2013). "Ulcerative colitis". BMJ. 346: f432. doi:10.1136/bmj.f432. PMID 23386404. S2CID 14778938.
- Akiho H, Yokoyama A, Abe S, Nakazono Y, Murakami M, Otsuka Y, et al. (November 2015). "Promising biological therapies for ulcerative colitis: A review of the literature". World Journal of Gastrointestinal Pathophysiology. 6 (4): 219–227. doi:10.4291/wjgp.v6.i4.219. PMC 4644886. PMID 26600980.
- Danese S, Fiocchi C (November 2011). "Ulcerative colitis". The New England Journal of Medicine. 365 (18): 1713–1725. doi:10.1056/NEJMra1102942. PMID 22047562.
- Vos, Theo; et al. (GBD 2015 Disease and Injury Incidence and Prevalence Collaborators) (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- Adams JG (2012). Emergency Medicine E-Book: Clinical Essentials (Expert Consult – Online). Elsevier Health Sciences. p. 304. ISBN 978-1455733941.
- Hanauer SB, Sandborn W (March 2001). "Management of Crohn's disease in adults". The American Journal of Gastroenterology. 96 (3): 635–43. doi:10.1111/j.1572-0241.2001.3671_c.x (inactive 28 February 2022). PMID 11280528. S2CID 31219115.
- Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF (April 2017). "Ulcerative colitis". Lancet. 389 (10080): 1756–1770. doi:10.1016/S0140-6736(16)32126-2. PMC 6487890. PMID 27914657.
- Magro F, Gionchetti P, Eliakim R, Ardizzone S, Armuzzi A, Barreiro-de Acosta M, et al. (June 2017). "Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, Diagnosis, Extra-intestinal Manifestations, Pregnancy, Cancer Surveillance, Surgery, and Ileo-anal Pouch Disorders". Journal of Crohn's & Colitis. 11 (6): 649–670. doi:10.1093/ecco-jcc/jjx008. PMID 28158501.
- Kaitha S, Bashir M, Ali T (August 2015). "Iron deficiency anemia in inflammatory bowel disease". World Journal of Gastrointestinal Pathophysiology. 6 (3): 62–72. doi:10.4291/wjgp.v6.i3.62. PMC 4540708. PMID 26301120.
- Hanauer SB (March 1996). "Inflammatory bowel disease". The New England Journal of Medicine. 334 (13): 841–848.
Ulcerative Colitis: Causes, Symptoms, Diagnostics
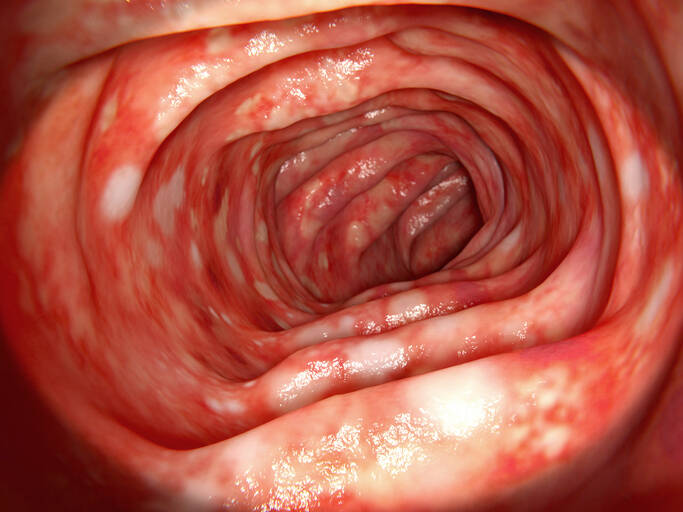
Photo source: Getty images
Most common symptoms
- Aphthae
- Malaise
- Stomach pain after a meal
- Abdominal Pain
- Joint Pain
- Anal pain
- Painful bowel movements
- Lower Abdominal Pain
- Fever
- Increased body temperature
- Cramps in the abdomen
- Nausea
- Diarrhoea
- Rash
- Bleeding
- Indigestion
- Malnutrition
- Stool with blood - blood in the stool
- Dry skin
- Fatigue
- Vomiting after eating and nausea
- Vomiting
Show more symptoms ᐯ
Treatment of ulcerative colitis: medications or surgery? Which one to choose?
Show moreUlcerative Colitis is treated by
Other names
colitis ulcerosa, colitis, non-specific chronic colitis, idiopathic proctocolitis, proctocolitis idiopathica










