- Moore, Keith L. (2018). Clinically oriented anatomy. A. M. R. Agur, Arthur F., II Dalley (8 ed.). Philadelphia. pp. 98–108. ISBN 978-1-4963-4721-3. OCLC 978362025.
- Windsor, Robert E (2006). "Frequency of asymptomatic cervical disc protrusions". Cervical Disc Injuries. eMedicine. Retrieved 2008-02-27.
- Ernst CW, Stadnik TW, Peeters E, Breucq C, Osteaux MJ (Sep 2005). "Prevalence of annular tears and disc herniations on MR images of the cervical spine in symptom free volunteers". Eur J Radiol. 55 (3): 409–14. doi:10.1016/j.ejrad.2004.11.003. PMID 16129249.
- "Prolapsed Disc Arizona Pain". arizonapain.com. Retrieved 2015-02-10.
- Simeone, F.A.; Herkowitz, H.N.; Garfin (2006). Rothman-Simeone, The Spine. ISBN 9780721647777.
- Del Grande F, Maus TP, Carrino JA (July 2012). "Imaging the intervertebral disk: age-related changes, herniations, and radicular pain". Radiol. Clin. North Am. 50 (4): 629–49. doi:10.1016/j.rcl.2012.04.014. PMID 22643389.
- Anjankar SD, Poornima S, Raju S, Jaleel M, Bhiladvala D, Hasan Q. Degenerated intervertebral disc prolapse and its association of collagen I alpha 1 Spl gene polymorphism: A preliminary case control study of Indian population. Indian J Orthop 2015;49:589-94
- Kawaguchi, Y. (2018). "Genetic background of degenerative disc disease in the lumbar spine". Spine Surgery and Related Research. 2 (2): 98–112. doi:10.22603/ssrr.2017-0007. PMC 6698496. PMID 31440655.
- Hirose, Yuichiro; et al. (May 2008). "A Functional Polymorphism in THBS2 that Affects Alternative Splicing and MMP Binding Is Associated with Lumbar-Disc Herniation". American Journal of Human Genetics. 82 (5): 1122–1129. doi:10.1016/j.ajhg.2008.03.013. PMC 2427305. PMID 18455130.
- Shimozaki, K.; Nakase, J.; Yoshioka, K.; Takata, Y.; Asai, K.; Kitaoka, K.; Tsuchiya, H. (2018). "Incidence rates and characteristics of abnormal lumbar findings and low back pain in child and adolescent weightlifter: A prospective three-year cohort study". PLOS ONE. 13 (10): e0206125. Bibcode:2018PLoSO..1306125S. doi:10.1371/journal.pone.0206125. PMC 6205614. PMID 30372456.
- Kraemer J (March 1995). "Natural course and prognosis of intervertebral disc diseases. International Society for the Study of the Lumbar Spine Seattle, Washington, June 1994". Spine. 20 (6): 635–9. doi:10.1097/00007632-199503150-00001. PMID 7604337.
- Ball, J. R.; Harris, C. B.; Lee, J.; Vives, M. J. (2019). "Lumbar Spine Injuries in Sports: Review of the Literature and Current Treatment Recommendations". Sports Medicine - Open. 5 (1): 26.
Spinal Disc Herniation: Bulging and Protrusion of the Intervertebral Disc

We speak of a bulging intervertebral disc or disc herniation rather than a popped or protruded disc. Pain of this origin is intense, significantly impairs the quality of life of the affected person and is the reason for incapacity for work.
Most common symptoms
- Shoulder Blade Pain
- Malaise
- Chest pain
- Abdominal Pain
- Headache
- Limb pain
- Nerve pain
- Leg Pain
- Flank Pain
- Groin Pain
- Spirituality
- Pain that Radiates into the Shoulder
- Pain under the Right Shoulder Blade
- Nausea
- Head spinning
- Testicular pain
- Muscle stiffness
- Defence
- Tingling
- Erectile dysfunction
- Shooting pain in fingers and toes
- Back Pain
- Pressure on the chest
- Fatigue
Characteristics
When the intervertebral disc is dislocated, intense pain arises, which is at the site of the affected area or moves, that is, shoots to other parts of the body. In some cases, damage to the disc is the reason for other neurological difficulties.
The bulging of the disc can take different forms, causing different difficulties. It arises from a variety of causes, mainly as a result of incorrect posture while standing or sitting.
Diagnosis is not difficult, however, treatment requires patience. Sometimes a thorough reassessment and lifestyle change is sufficient, and other times surgery is necessary.
It is stated that the problem arises as a result of a long-term process. The flare-up of the acute stage occurs suddenly.
The pain is acute, i.e. sudden, and persists chronically, i.e. for a long time.
It reduces the quality of life, bothers with unpleasant pain, impaired mobility and other neurological difficulties. It is a cause of incapacity for work.
Intervertebral disc bulging is technically referred to as disc herniation, but we know it more colloquially as disc protrusion.
Disc disorders - discopathies include several disc problems and diseases. We describe some of them briefly, however, we spend more time on disc herniation.
Spinal problems are not only affecting seniors. Many young people have already discovered this. They occur frequently from 30 to 50 years of age.
- 4.8% of males and 2.5% of females older than 35 experience sciatica during their lifetime.
- Of all individuals, 60% to 80% experience back pain during their lifetime.
- In 14%, pain lasts more than two weeks.
- Generally, males have a slightly higher incidence than females.
Question: Why is that?
For example: sedentary lifestyle, sedentary work, prolonged standing and forced posture, incorrect posture, poor lifting of loads, and of course degenerative changes due to ageing.
They are the most common reason for a fit note (statements of fitness for work) at this time of life. They represent the 5th to 6th leading cause of hospitalisation in the European Union.
Rightly, spinal problems are referred to as a disease of civilization. This is also because every person encounters this problem at least once in the patient's life.
Back pain is collectively referred to as vertebrogenic algic syndrome. It stems from muscle spasms, such as in lumbago. Lumbago is more commonly known as a blockage in the spine or a chipping in the back.
A more serious condition is compression of the nerve for disc protrusion.
Read also:
Lumbago - acute spinal block
Sciatica, an inflammation of the sciatic nerve
Pain can occur in any part of the spine, from the neck to the coccyx (such as when sitting for long periods of time or after an accident). It is intense, irritating, sharp, prickly and aggravated by movement, even a slight change in position.
Let's describe what the spine and disc are.
Spine and discs at a glance
The spine, Lat. columna vertebralis, is the axis of the human body, which, together with muscles and ligaments, forms the supporting and locomotive apparatus of the human body.
Of course, the spine is also of protective importance for the spinal cord.
It is physiologically curved, with forward curvature referred to as lordosis - in the cervical and lumbar region, and backward curvature as kyphosis - in the thoracic and sacral region. This curvature is physiological, i.e. natural.
The opposite of a natural curvature, for example, is scoliosis, which is an unnatural - pathological sideways curvature of the spine. Although mild and slight (physiological) sideways curvature is present in every person.
Transient sideways curvature of the spine can be observed when standing on one leg, transferring weight to one limb or when carrying a heavier load in one hand.
The spine is made up of 33 or 34 vertebrae.
Table: vertebrae divide the spine into segments according to their location
| Segment | Latinn name of the spine | Description |
| Cervical spine | vertebrae cervicales |
|
| Thoracic spine | vertebrae thoracicae |
|
| Lumbar spine | vertebrae lumbales |
|
| Sacral spine | vertebrae sacrales |
|
| Coccyx | vertebrae coccygeae |
|
The vertebrae (along with other soft structures) form the support for the human body, and their foramina vertebralis, or vertebral openings, form the spinal canal through which the spinal cord passes. The spinal cord is located between vertebrae C1 to L1 - L2.
Spine - the vertebrae are firmly connected to each other; the connection is formed by, for example:
- ligaments - ligamentous apparatus, ligaments of the spine, strengthen the spine and assist in movement
- that are long and short
- long ligaments go alongthe entire spine
- short ligaments connect the adjacent discs
- that are long and short
- intervertebral joints - art. intervertebrales
- the muscular system, the muscles of the spine together with the muscles of the abdomen and the muscles of the neck and pelvis
- form the movement and fixation component of the spine
- significant overall in movement and posture
- intervertebral discs
- a special connection, such as
- synchondrosis
- cartilagous connection
- non-moving connection
- in the sacrum and coccyx they ossify with age - they turn into bone
- synchondrosis
Intervertebral discs are...
Disci intervertebrales, as they are called in Latin, are flexible, but on the other hand, rigid discs that are located between the vertebrae of the spine.
Their shape and structure are adapted for pressure relief, for stretching or rotation in the spine. They are flexible fillings - inserts between the vertebrae.
The function of the discs is, for example:
- shock absorption when moving, walking, running, jumping
- stabilise the spine
- maintain balance
- equalizes pressure and tensile forces, spreading it over the entire surface
- they are effective in any spinal movement, bending or rotation of the body
Their shape follows the shape of the vertebrae. They vary in height, being higher between the cervical and lumbar vertebrae. The highest disc is between the L5 and S1 vertebrae.
The discs are not at the junction of the skull and spine, and also between the 1st and 2nd vertebrae of the cervical spine.
The discs are located between the vertebrae of the spine from the junction of C2 and C3 to L5 and S1. Their combined length is approximately 20-25% of the total length of the spine.
There are 23 intervertebral discs.
Table: the intervertebral disc consists of two main parts
| Disc segment | Medical (Latin) term | Description |
| Fibrous ring | Anulus fibrosus |
|
| Centre | Nucleus pulposus |
|
| Vertebral endplate | Vertebral body endplate |
|
The disc, and therefore we are thinking mainly of its centre, has no blood supply.
Nutrition to the disc occurs through the passage of fluid.
This is aided by movement, changes in the position of the spine, especially walking.
As it is, for example, when sucking the liquid with a sponge.
Therefore, inactivity and prolonged sitting or standing impairs the nutrition of the centre of the disc.
That contributes to the emergence of difficulties in the future.
The discs are loaded both statically and dynamically throughout their lifetime.
The load causes expulsion of fluid, which is also referred to as the creep phenomenon.The height of the disc decreases. Conversely, on release, the fluid is sucked back in, thus restoring the height.
Alternating the load and release of the disc creates fluid flow in the core. And thus its nutrition.
The static load causes the elastic rings to stretch, leaving the core inside almost incompressible. The force is evenly distributed over the entire plate - uniform loading.
The dynamic load acts differently.
Loads in motion cause uneven distribution of force and overload. This is where the vulnerable space emerges.
Examples include the prone position and lifting a load. The vertebrae are tilted, thus loading the disc unevenly.
In the same way, prolonged positioning causes a restriction in the nutrition of the disc, thereby limiting its functionality and elasticity.
Let's take a closer look at disc herniation
The discs can be affected by various problems. One of them is disc herniation.
Degenerative damage to the disc, which is also referred to as discopathy,is the main basis of the problem. There is a decrease in the height of the disc, which is the result of biochemical and structural changes.
The disk's properties are changed and the function malfunctions. Thus, degenerative change and disc herniation are closely related.
A disc herniation refers to a condition where there is an anatomical deviation in the position of a disc or part of a disc, outside of its normal location. It mostly extends beyond the margin of the vertebral body.
The degenerative process starts early, already during adolescence. It is reported to be around 13 to 19 years of age. However, after the age of 30-50, the process reaches its peak.
And it is after the age of 30-50 years that the most frequent occurrence of disc herniations is reported.
It affects men to a greater extent.
The most flexible parts of the spine are the cervical and lumbar spine. These are the most loaded. And it is in these places that disc dislocation occurs most often.
More precisely:
The most common area of intervertebral disc dislocation is reported to be the lumbar part of the spine.
Even more precisely:
The main area of disc herniation is the area between vertebrae L4 - L5 or L5 and S1.
In the cervical region, the intervertebral spaces between vertebrae C4 - C5 or C5 - C6 are frequent.
The thoracic spine is less frequently to rarely affected by herniation.
Most commonly, it is the intervertebral discs between the vertebrae L4 - L5 or L5 - S1.
Question: Where is the cause of intervertebral disc protrusion?
The answer is given in the section on causes.
However, the issue of herniation is more complex. Since herniation can take different forms.
The degenerative process damages the structure of the anulus fibrosus ligamentous ring for a long time. This damage causes the ring to weaken. Through this weakened site, the nucleus of the disc may bulge under increased load.
Please note, however...
It is reported that the process of degeneration and damage does not only affect the annulus of the disc itself. But it is a negative impact in the whole segment.
That means it affects:
- intervertebral disc
- intervertebral joints
- the vertebra itself - i.e. the body of the vertebra
- ligaments
- and other soft structures
Tableau: the degenerative process itself is classified into three stages
| Stage | Description |
| Dysfunction, stage 1 |
|
| Instability, stage 2 |
|
| Restabilistation, stage 1 |
|
Table: degenerative cascade according to Kirkaldy and Willis
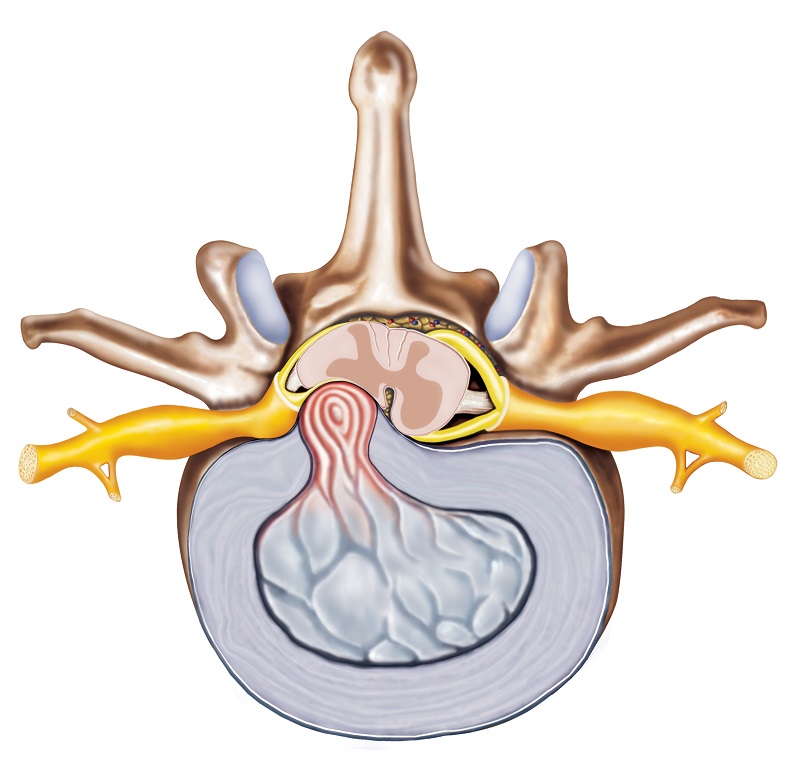
Herniation of the intervertebral disc can take various forms.
1. Disc bulging
Bulging of the disc is a symmetrical bulging of the anulus fibrosus up to 3 millimetres over the edge of the vertebral body. At the same time, the height of the disc decreases in one place only. The anulus fibrosus is not violated.
At this stage, it is not yet referred to as a hernia. Mostly it does not create compression, i.e. oppression of nerve roots.
2. Disc protrusion
In this form, the anulus fibrosus structure is delaminated; however, its outer lamellae are still preserved. However, the bulging is asymmetrical but circumscribed.
The centre of the disc thus does not get through the space of the disc area. The edges of the disc are still smooth.
3. Disc extrusion
In this case, it is already a prolapse or herniation of the disc. The lamellae of the ring are torn and they rupture.
Následne preniká jadro, čiže nucleus pulposus, cez trhlinu v prstenci, a to mimo oblasť platničky. Vyklenutie má nepravidelné okraje.
This form is further subdivided according to the dislocation of part of the disc:
- subligamentous extrusion - part of the disc is dislocated, i.e. it is outside the disc
- does not yet exceed the ligament - lig. longitudinale posterius
- it just lifts it up and pushes it out
- most major herniations are just this type of extrusion
- extrusion with sequester - is a condition where there is a rupture of this ligament (lig. longitudinale posterius)
- the contents of the hernia penetrate beyond the ligament
- completely detaches from the disc
In addition to structural changes in the vertebral segment, the main problem is the compression of nerves in the region of the spinal canal. Subsequently, according to the place of oppression, neurological difficulties are also associated.
According to the place of oppression, hernia is divided into:
- lateral
- medial
- mediolateral
- foramenal
- extraforaminal
Causes
The exact cause of the damage to the disc is not fully understood. Several theories of the origin have been put forward. Examples are the genetic theory or the developmental theory.
Genetic assumes gene disorders that are the cause of structural weakening. Developmental, in turn, states that it is a disorder during intrauterine development.
The degenerative process is considered to be one basic theory.
Just as the characterization states, it is a process that begins at a young age. The disturbance of vascular supply and nutrition causes impaired function. This is followed by a change in the structure of the disc.
A healthy disc is able to distribute the load evenly.
However, over time it loses this ability. The uneven, non-linear and asymmetrical application of overload to the spinal segment is the underlying problem for the development of disc herniation.
Uneven loading of the spine + prolonged and repetitive overloading of a specific area of the spine = problem.
In this context, the interaction of different factors is mentioned. They could be described as negative multifactorial risk factors in the development of degenerative changes and the triggering of dislocation to herniation of the intervertebral disc.
Significant risk factors include:
- trauma, injury
- hypermobility
- developmental disorders
- metabolic disease
- the natural ageing process
- age
- sex
- family history and therefore family burden
- obesity
- incorrect posture and habits when walking, sitting or lying down
- type of profession
- excessive vibration, e.g. in the work environment, industry
- lack of exercise - inactivity
- lack of proper exercise
- sedentary lifestyle
- sedentary job
- inappropriate seating
- prolonged standing and forced positioning, e.g. at work
- unilateral loading and repetitive overloading - forced position during work, activity
- improper lifting of loads
- bending in an unnatural position, rotation in prone position
- fajčenie
It is not so much the sitting itself as inappropriately long sitting or incorrect sitting that causes the difficulty.
Therefore, it is necessary to change the position from time to time when working in a sedentary position.
Bad habits, incorrect posture, prolonged sitting, uneven and careless loading of the spine lead to problems that can lead to disc herniation.
The reason for this is a weakening of the muscles of the spine or body core and the overall support system, which results in instability of the spine. The load acts unevenly on the shock absorbers - the discs, between the vertebrae.
Overloading of the intervertebral disc:
In lying position = 25 %
In standing position = 100 %
In a sitting position = 150 %
Leanig forward = 200 %
Pri zdvíhaní záťaže z predklonu s vyrovnanými dolnými končatinami = 1000 %
The cause of the difficulty is nerve compression
One side of the issue is why it arises. However, the other is causing the difficulty.
The cause of pain or neurological discomfort is the bulging of the disc into the spinal canal space or nerve roots.
If the bulging contents of the disc are the cause of compression, it provokes pain that is intense to severe. The pain is associated with various neurological disorders.
The type thereof depends on the site of spinal cord or nerve compression.
In the cervical spine, difficulties can radiate to the upper limbs. If the problem is in the lumbar region, then lower down from the site of the affection.
Symptoms
The main symptom of a herniated disc is pain. This is followed by other difficulties that stem from oppression. Of course, the specific difficulties depend on the site of the damage.
Question:What are the symptoms of a ruptured disc?Disc/back pain is not the only manifestation.One is bothered by a set of problems...
Symptoms occurring in disc herniation:
- sudden pain, usually of high intensity
- sharp
- irritating
- stabbing
- the pain is aggravated by movement, change of position, sneezing or coughing, but also by pressure on the stool
- antalgic tilt of the torso
- from the disability side
- antalgic, i.e. pain-relieving
- relief position
- standing on a painful limb
- examination of the limb to which the discomfort radiates
- muscle tension
- congealing
- tingling
- nerve root symptoms
- impaired sensitivity, even loss of skin sensitivity
- impaired mobility, muscle weakness, muscle spasms
- relief in the supine position, sideways with the limbs bent at the knees
The pain is localized to the affected segment of the spine. Accordingly, the discomfort then radiates to the upper limbs and chest - when the cervical spine is affected, or to the lower limbs, in the case of damage in the region of the cervical spine.
Nerve root syndromes - what does this term mean?
If you have a problem with your spine, you've probably already noticed the term nerve root syndrome.
It arises in the case of direct pressure on the nerve root. And in this case, as the most common cause cites disc herniation.
Read more in: Nerve root syndrome - radicular syndrome, radiculopathy
Others that need to be differentiated include, for example, a condition after a spinal injury, inflammation or a tumour in the nerves and spinal cord.
The manifestations are the typical difficulties that characterize the affected segment, ranging from reduced muscle tone, impaired mobility, as well as impaired sensitivity and reflexes.
Pain due to nerve compression is referred to as radicular pain. Other neurological discomforts that radiate in the area of innervation in the respective dermatome are also associated.
Severe cauda equina syndrome
This is a serious condition that arises as a result of the oppression of a tangle of nerves referred to as the cauda equina.
The spinal cord runs through the spinal canal to approximately the 1st to 2nd cervical vertebrae, and hence L1 to L2. A bundle of nerves also referred to as the cauda equina, or horse's tail, extends from it.
This syndrome is characterised by significant impairment of either motor or sensory functions. The impairment occurs at the level of the pelvic organs and pelvic floor, but also in the lower limbs.
Learn more: Cauda equina syndrome.
This is due to a medial type herniation in the region of the cervical spine below the L2 vertebra - the second cervical vertebra. Symptoms are variable and dependent on the site and extent of the compression.
An example is a disorder of sensitivity in the genital and rectal area. Pain in the anus with bilateral or unilateral radiating after the dermatome.
An example of motor dysfunction is the weakening of the muscles in the lower limbs, but also the dysregulation of the sphincters and incontinence, i.e. the passage of urine and faeces. Alternatively, sexual function is impaired.
Diagnostics
Diagnosis is not difficult nowadays. It is based on medical history and physical examination.
To this are added other special investigation methods.
The clinical examination is carried out by a specialist, i.e. a neurologist.
The condition is visually evaluated, i.e. posture, gait. Palpation, i.e. touching of muscle tension. Examination of the spine and its function is important - examination of the dynamics of the spine and range of motion. Neurological examination also includes other specialized methods, such as the presence of reflexes and maneuvers (Laségue maneuver and others).
Important imaging methods include:
- X-ray
- CT
- MRI
- EMG
Differential diagnosis is important, the task of which is to differentiate it from another cause of the difficulty. Examples include pseudoradicular syndrome, spinal fractures - after a fall, inflammatory disc or vertebral disease, degenerative nerve disease, cardiac disease, oncological disease or psychiatric disorder.
Course
The course of the disease on the basis of the degenerative process may be initially mute, i.e. it proceeds asymptomatically. The acute stage can be triggered, for example, by lifting a load, but also by turning in an inappropriate position.
An example is if we are lifting a heavy load from a prone position with our lower limbs straightened.
Subsequently, as the herniation progresses and worsens, it manifests with pain and various neurological problems. The pain tends to be of high intensity, possibly aggravated by movement and incorrect position or attempt to change it.
Getting out of bed in the morning, standing in a prone position (for morning hygiene), sitting for long periods of time or longer rides in the car and other means of transport, coughing, sneezing or pressure on the stool are also problems.
The pain is accompanied by a weakening of the muscles in the area and during the dermatome - that is, in the area of innervation. Other neurological symptoms include impaired limb mobility or skin sensitivity.
The acute stage may alternate with a period without difficulties.
The opposite of a rapid onset is a slow and gradual progression. Mild pain in the spine escalates and other difficulties are associated.
The trigger can be an accident, inappropriate sports activity, bending over, lifting a load, even a sneeze or a cold in the spine.
The course, like the symptoms, is dependent on the site and extent of the disc herniation.
Prevention
It is important to remember that treatment of this type, and other spinal problems in general, requires a long-term approach and a change in overall lifestyle.
Treatment is long-term, and depends on the other measures that a person is willing to take/adjust/sacrifice for the better condition of his/her spine. Even before the onset of the problem itself, it is necessary to think about prevention. Prevention is #1.
Prevention includes:
- regular and appropriate exercise
- keep walking
- correct posture
- appropriate seating with occasional changes of position - sufficient breaks while working
- the correct technique for lifting loads
- elimination of inappropriate movement habits
- beware of one-sided loading
- back school
These preventive measures also serve to improve outcomes for spinal problems that are already present. You should never wait. It is very important to start immediately.
How it is treated: Spinal Disc Herniation
Herniated disc, treatment: medication, exercise or surgery
Show moreSpinal Disc Herniation is treated by
Other names
Interesting resources










