- TESAŘ, Vladimír and Ondřej VIKLICKÝ, ed. Klinická nephrologie. 2nd, completely revised and supplemented edition. Prague: Institute of Nephrology and Biochemistry of the CAS, v. v. i.: Grada Publishing, 2015. ISBN 978-80-247-4367-7.
- HORA, Milan and Olga DOLEJŠOVÁ. Urology for students of general medicine. Prague: Faculty of Urology, Charles University in Prague: Karolinum, 2020. ISBN 978-80-246-4544-5
- urologiepropraxi.cz - Prostatic syndrome - bacterial inflammation. Urology for practice. Kamil Belej, Dr., FEBU
- urologiepropraxi.cz - Prostatitis - practical notes on diagnosis and treatment. MUDr. Martina Porsová , MUDr Ivan Kolombo, FEBU, MUDr Jaroslav Pors
- healthline.com - Prostatitis. Healthline. Joseph Brito III, MD
Inflammation of the prostate (prostatitis): what are its causes and symptoms?
Prostatitis is the lay name for inflammatory processes in the prostate from various causes and diseases. It is a urological-sexual problem in men. Why does prostatitis arise and what are all the possible causes?
Most common symptoms
- Lower Abdominal Pain
- Painful urination
- Frequent urination
- Increased body temperature
- Nausea
- Testicular pain
- Blood in the power
- Back Pain
- Fatigue
- Decrease in libido
Characteristics
Why does prostatitis (inflammation of the prostate) occur and what are the symptoms? What is effective prevention?
The prostate is an important organ of the male genital and urinary system. Inflammation of the prostate tissues has a multifactorial cause of occurrence.
According to the symptoms and duration, prostatitis is divided into acute and chronic. A common symptom is difficulty urinating and local pain.
Etiology of occurrence, distribution, first symptoms, diagnosis, treatment options, prevention and many other interesting information can be found in the article.
Prostate inflammation
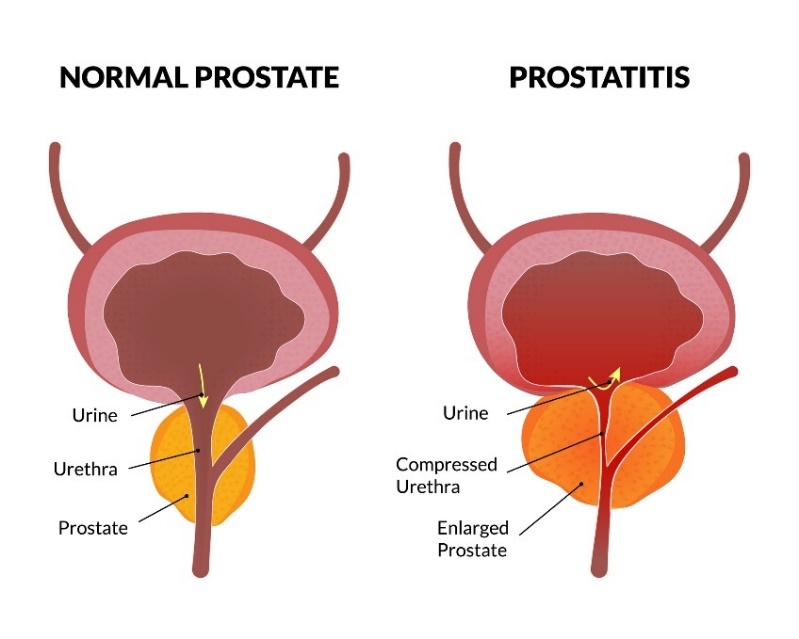
The prostate is an internal organ of the male reproductive system. It is the size of a walnut. It is located under the bladder and surrounds the urethra.
The main function of the prostate is to produce fluid that protects the male sex cells (sperm) and mediates their movement to the female sex cells during intercourse.
Inflammation of the prostate can take an acute or chronic form. It varies slightly according to the symptoms and their duration.
Acute bacterial prostatitis occurs when health problems develop rapidly and has relatively strong symptoms. In contrast, the chronic form has milder manifestations and can persist for a long time, including an asymptomatic (symptomless) period.
In inflammation, there is an inflammatory process in the tissues of the prostate and their eventual swelling (enlargement). This can lead to a reduction in the function of the organ and affect the surrounding genitourinary structures.
The basic symptoms include local pain in the prostate area, difficulty in urinating sufficiently, discomfort when urinating, pelvic pain, decreased libido or problems with the quality of erection.
Causes
Prostatitis can have various provoking factors and causes.
The cause of the acute form is mainly a bacterial infection, which can pass into chronicity if not treated.
Chronic prostatitis of non-bacterial origin, known as pelvic pain syndrome, is common. This form of prostatitis can be both inflammatory and non-inflammatory, depending on the findings.
Professional classification of prostatitis:
- Acute bacterial prostatitis
- Chronic bacterial prostatitis
- Chronic prostatitis (pelvic pain syndrome)
- Asymptomatic prostatitis (incidental finding)
Possible causes of prostatitis
What are the most common causes?
Bacterial/viral infection
The cause of acute prostatitis is mainly bacterial infections caused by bacteria such as E. coli, staphylococcus, Neisseria gonorrhoeae, chlamydia and other pathological organisms.
The infection spreads from the urethra towards the prostate.
Unprotected sexual intercourse is risky as it can lead to transmission of infectious diseases. Including anal intercourse. In most cases, due to the anatomical connection between the male excretory and reproductive systems, both the urinary tract and the prostate are inflamed.
If there is frequent inflammation of the urinary tract, the risk of prostatitis increases at the same time.
Any inflammation of the urinary tract should therefore not be underestimated. It should be treated professionally.
The most common cause of chronic prostatitis is repeated urinary tract infections.
Prostatitis can also be associated with other diseases in the surrounding area. Infection can enter the prostate by ascending from the urethra or, conversely, by descending from the bladder.
Transmission of infection is also possible through the bloodstream.
Prostate enlargement (hyperplasia)
As the prostate tissue enlarges, pressure on the urinary tract increases. There is close contact with the urinary organs and the increased pressure causes a sensation of frequent urination. Problems with excretion also occur.
Residual urine in the urinary tract increases the risk of infection.
Prostatic hyperplasia can be benign due to advanced age and hormonal changes. However, it can also be malignant, so prevention and consultation with a urologist is necessary.
Medical interventions in the prostate
Rarely, bladder catheterisation, cystoscopy or other invasive procedures in the prostate and surrounding structures can also contribute to the development of infection.
Prostate biopsy is one of the most common procedures that can cause a risk of infection from the surrounding external environment. Therefore, the patient is prescribed prophylactic antibiotic treatment at the time of the procedure.
Risk factors for the development of
As a man ages, the level of the hormone testosterone decreases and the immune system weakens at the same time. This makes the body more susceptible to developing the disease.
Irregular sexual intercourse and too few ejaculations is another factor that contributes to the risk of prostatitis. Another risk factor is insufficient drinking and insufficient or incomplete urinary excretion from the urinary tract.
Summary of risk factors and causes of prostatitis:
- Bacterial/viral infection
- Unprotected sexual intercourse
- Inadequate urine output
- Prostate enlargement (hyperplasia)
- Medical interventions in the prostate area
- Decreased testosterone levels and hormonal imbalance
- Irregular intercourse and ejaculation
- Inadequate drinking regime
- Anomalies of the genitourinary tract
Symptoms
The course and nature of symptoms may vary depending on the cause.
The acute infectious form may cause increased body temperature, blood in the urine or ejaculate and a burning sensation when urinating. The chronic form has milder symptoms but also symptomless periods alternating with severe acute worsening of symptoms.
The most common manifestation of prostatitis is a feeling of incomplete urine voiding, frequent urinary frequency and discomfort when urinating. The chronic form may also manifest itself in erectile function and a general decrease in sex drive.
Possible symptoms of the acute form:
- Pain and burning during urination
- Difficulty urinating completely
- Local pain in the prostate area
- Pain in the lower abdomen and back
- Nausea and general weakness
- Increased body temperature
- Painful intercourse
- Painful ejaculation
- Presence of blood in urine/ejaculate
Possible symptoms of the chronic form:
- Frequent frequency of urination
- Feeling of incomplete emptying
- Weak inadequate stream of urine
- Pain in the urinary and genital organs
- Pain in the pelvic area
- Painful ejaculation
- Uncomfortable intercourse
- Decrease in sex drive and libido
- Decrease in erection quality
Diagnostics
Men are most often brought to the urologist by unwanted symptoms when urinating. The beginning of the diagnosis consists of taking a medical history, assessing clinical symptoms and a basic medical examination by palpation.
Physiological examination of the prostate by palpation is also performed with a finger over the patient's anus.
A urine sample is taken for laboratory analysis and to detect or exclude the presence of bacteria. Blood sampling and assessment of inflammatory markers such as CRP are also common.
It is also possible to perform a swab and laboratory analysis of prostatic secretions to confirm the presence of white blood cells and the inflammatory process.
Within the imaging methods, ultrasonography (ultrasound), computed tomography (CT) or magnetic resonance imaging (MRI) are common. Instrumental methods are used to view internal soft structures in detail.
The goal of these tests and examinations is to determine the etiology and exact cause of the health problem and then determine the appropriate type of treatment.
Prevention of prostatitis
Some prevention is possible with prostatitis. This includes, in particular, careful intimate hygiene, sufficient drinking with regular urination and, last but not least, protected sexual intercourse.
Prevention of overall prostate health includes a balanced diet with plenty of fibre, vitamins and minerals, regular physical activity, limiting smoking, alcohol and eliminating stress factors.
Excessive intake of foods high in salt, fat and refined sugar is problematic.
On the other hand, cranberries, blueberries, broccoli, leafy greens, pumpkin seeds and others are protective foods.
Regular preventive checkups with a urologist are important, especially because of the possibility of asymptomatic and chronic prostatitis. Part of the care is not to postpone health problems and to see a doctor in time for acute problems.
Regular ejaculation helps to keep the prostate in a physiological state. Regular intercourse and ejaculation are important for the urethra, the testicles, and male spermatogenesis itself.
Natural herbal help in the form of teas or dietary supplements to support male genital and urinary tract health is a prevention option. Examples include willowherb, anchorwort, saw palmetto (serenoa), nettle, goldenseal, plum and others.
The basics of prostate inflammation prevention:
- Preventive checkups with a urologist
- Solving acute problems with a urologist
- Adequate drinking of clean water
- Regular urine output and not retaining urine
- Protected sexual intercourse
- Adequate intimate hygiene
- Regular ejaculation
- Regular physical activity
- Avoidance of smoking and alcohol
How it is treated: Inflammation of the prostate - prostatitis
Treatment options for prostatitis: drugs, antibiotics, surgery?
Show moreInflammation of the prostate is treated by
Other names
Interesting resources
Related










