- ROZTOČIL, Aleš and Pavel BARTOŠ. Modern gynaecology. Prague: ISBN 978-80-247-2832-2.
- ROB, Lukáš, Alois MARTAN and Pavel VENTRUBA. Gynaecology. Third, supplemented and revised edition. Prague: Institute of Gynaecology and Obstetrics of the CAS, v. v. i.: Galén, [2019]. ISBN 978-80-7492-426-2
- HURYCH, Jakub and Roman ŠTÍCHA. Medical microbiology: repetitorium. 3rd edition. Czech Republic: Stanislav Juhaňák - Triton, 2021. ISBN 978-80-7553-976-2.
- journals.asm.org - Genital herpes: a review of the epidemic and the potential use of type-specific serology. Reviews of clinical microbiology. Rhoda L. Ashley, Anna Wald
- pubmed.ncbi.nlm.nih.gov - Genital herpes: an overview. national library of medicine. mary Jo Groves
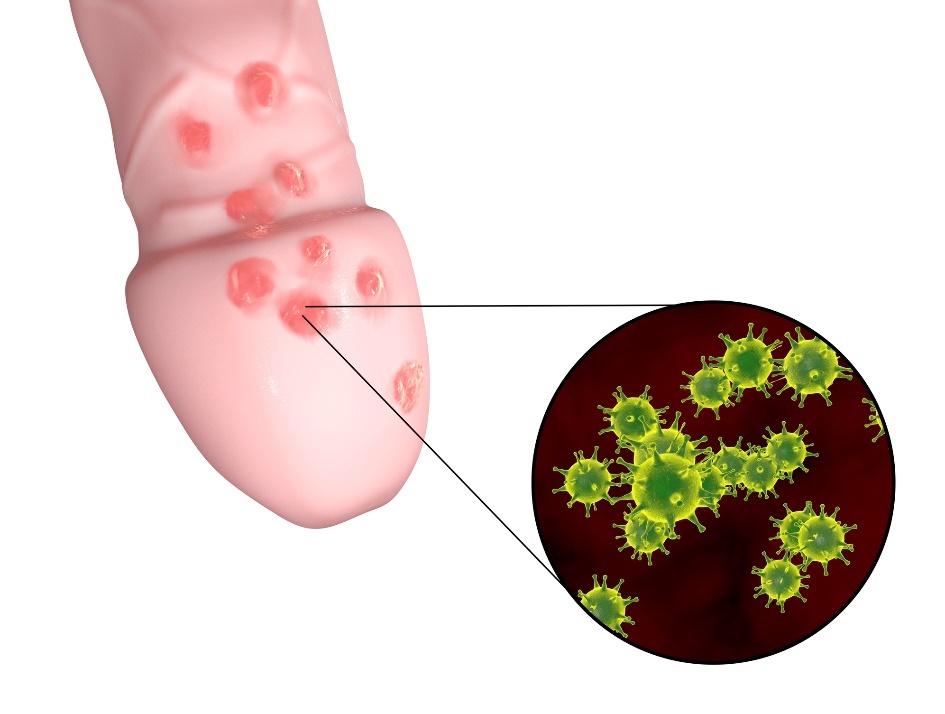
Genital herpes: what does it look like and what symptoms does it have? Method of prevention

Genital herpes is one of the most common sexually transmitted diseases. It is an easily transmissible infectious disease occurring in both men and women. How to recognize genital herpes correctly? What are the ways in which the virus can be transmitted and what treatment options are available?
Most common symptoms
- Headache
- Urethral pain
- Fever
- Increased body temperature
- Nausea
- Blisters
- Fatigue
- Vaginal discharge
- Reddened skin
- Reddened penis
Characteristics
Genital herpes, also known as genital herpes, is a viral disease caused by a type of herpes simplex virus. In the case of genital infection, it is usually of the HSV-2 subtype.
Genital herpes is a common infectious disease transmitted primarily through sexual contact. It is classified as a sexually transmitted disease (STD).
Genital herpes is characterised by its unpleasant external manifestations in the genital area.
Herpes simplex genitalis manifests itself on the mucous membranes and skin around the genital area. In a woman it is mainly around the vagina, labia and in a man usually at the end of the genitalia.
A characteristic feature of genital herpes is its latency. The virus can survive and 'sleep' in the human body for a long time. It does not multiply and migrates to the posterior spinal ganglia (nervous system formations).
Hidden from the protective cells of the immune system, it waits for an opportunity to weaken the organism and the host's immunity, when the virus reactivates.
Genital herpes is a disease with a relatively short incubation period. From the first infection or contact of the virus with the organism, the first visible symptoms soon appear.
The usual incubation period of the herpes simplex virus usually ranges from 2 to 7 days.
Causes
Genital herpes is transmitted through mucous membranes.
The virus is mainly transmitted through sexual contact (saliva, blood, vaginal secretions or male ejaculate), anal and oral contact. The virus is transmitted directly from the host to the infected person.
Even mechanical barrier sexual protection (condom) may not provide 100% protection against genital herpes.
Transmission can also occur by direct skin or mucous membrane contact with the herpes. In rare cases, transmission by an infected object such as cutlery, a towel or a sponge is also possible. However, outside of contact with a living organism, the virus dies very quickly.
As with most venereal diseases, herpes simplex genitalis affects the female sex more often. This is due to the excessively moist and warm vaginal environment, which creates ideal conditions for the development of microorganisms.
A possible mode of transmission is the transmission of the virus infection from mother to child perinatally, i.e. during childbirth. However, the most common mode of transmission is during vaginal delivery through the natural birth canal.
Therefore, regular health monitoring and consultation with a doctor is necessary during pregnancy.
Recurrence and reactivation of infection can occur if the virus goes from a latent dormant phase to an active phase again.
This is the time when the body is weakened mentally and physically by deterioration of the immune system, overexposure to stress, hormonal imbalance or irritation of the genital area.

Symptoms
In some cases, the HSV infection is asymptomatic without visible symptoms, making the person a potential silent carrier.
Alternatively, the virus may behave latently, dormant and waiting for the body's immunity to weaken. In most cases, however, symptoms of genital herpes become apparent just a few days after the infected person has been infected.
The characteristic symptom of genital herpes is the formation of numerous fluid-filled blisters in the genital area.
Initially, there is increased redness where a small blister forms. Later, small blisters begin to form and spread to the genital area.
In the next stage, the blisters get bigger and wider, accumulate fluid and then the fluid bursts.
In women, the pubic area is most affected and in men the foreskin and glans penis. In the case of anal intercourse, the anal area and rectum may be affected.
In the case of oral intercourse, the oral cavity and lips may be affected.
In addition to the formation of characteristic fluid vesicles, genital herpes may also be accompanied by associated internal symptoms such as headache, enlarged lymph nodes, nausea or pain when urinating and many others.
The most common symptoms and manifestations of genital herpes are:
- Characteristic blisters in the genital area
- Redness with itching in the genital area
- Enlargement of the lymph nodes
- Increased fatigue
- General weakness and malaise
- Headache
- Muscle pain
- Nausea
- Increased temperature
- Discomfort when urinating
- Vaginal discharge
Diagnostics
Diagnosis of the disease is carried out by means of a specialist examination by a doctor. In the case of genital herpes, the woman is examined by a gynaecologist, the man by a dermatovenerologist or urologist.
The patient's medical history is taken and an examination by examination and palpation is carried out. The doctor uses clinical and laboratory examination to assess the presence of the herpes simplex virus and its specific subtypes (HSV-1, HSV-2) from a blood sample.
The patient's blood is drawn to determine the presence of antibodies to the virus. The blood test may detect the virus itself before the first outward signs of infection appear.
It is also performed if sexual contact with an infected person is suspected.
In many cases, a culture test in the form of a fluid swab is performed to detect the presence of the virus. The fluid swab is a short test performed using a special cotton swab and is not painful for the patient.
If the test is positive for the presence of the herpes simplex virus, it is necessary to inform the current sexual partners. In this way, it is possible to diagnose, treat and prevent further spread of the virus in time.
Prevention of genital herpes
Prevention of transmission of genital herpes simplex infection involves sexual abstinence and a non-promiscuous lifestyle (no frequent changes of sexual partners).
The ideal choice is to get tested for the presence of the virus and other STDs in the body of both partners and then be faithful to one sexual partner.
Regular preventive check-ups with a gynaecologist or urologist are strongly recommended. If any unusual symptoms occur, medical help should be sought as soon as possible.
Due to the easy course of the disease, it is advisable to have a stable strong immune system and high immunity of the organism.
Tips for preventing genital herpes:
- Safe sexual intercourse
- Limit promiscuity
- Regular intimate hygiene
- Preventive check-ups with a doctor
- Strong immune system
- Testing for sexually transmitted diseases
Myths and facts about genital herpes
Myth: A condom will 100% prevent transmission of the herpes simplex virus.
The condom as a mechanical barrier sexual protection may prevent or reduce the percentage chance of infection in some cases, but is not considered reliable and 100% protection against transmission of the virus.
Fact: The female sex is at higher risk of contracting the virus.
The female sex is slightly more susceptible to developing or transmitting infection within the body. The internal environment of the vagina is moist, warm and prone to the formation of micro-cracks in the mucosal tissue during intercourse.
As a result, it is an ideal gateway for the transmission and multiplication of theherpes simplex genitale virus.
Myth: Genital herpes can also be cured with a "grandmother's recipe".
Genital herpes is not recommended to be treated with home recipes. Professionally untreated genital herpes can cause subsequent health problems. Alternative natural treatment support in the form of herbs is a benefit, but not the primary solution.
It is recommended to consult home recipes with the treating physician.
Fact: The viral disease is dangerous during pregnancy.
Genital herpes and a woman's period of pregnancy is definitely not a safe combination. With extensive infection of the disease, the virus can be transmitted by the mother to the fetus.
However, the bigger problem is the birth itself, where the baby can become infected while passing through the mother's natural birth canal. The ideal is to prevent this situation by preventing the disease.
If the genital virus is present in the body during pregnancy, regular follow-up with a gynaecologist is necessary to determine the treatment. It is necessary to monitor the health of both mother and child before and after delivery.
How it is treated: Genital herpes
Treatment of genital herpes? How to get rid of it, what drugs will help?
Show moreGenital herpes is treated by
Other names
Interesting resources
Related










