- Cover of Hacker & Moore's Essentials of Obstetrics and Gynecology". Hacker & Moore's essentials of obstetrics and gynecology (6 ed.). Elsevier Canada. 2015. pp. 276–290. ISBN 9781455775583.
- Dallenbach-Hellweg, Gisela; Schmidt, Dietmar; Dallenbach, Friederike (2010). Atlas of Endometrial Histopathology. Springer Science & Business Media. p. 135. ISBN 9783642015410.
- Lobo, Rogerio A.; Gershenson, David M.; Lentz, Gretchen M.; Valea, Fidel A. (2016). Comprehensive Gynecology E-Book. Elsevier Health Sciences. p. 548. ISBN 9780323430036.
- Ferri, Fred F. (2014). Ferri's Clinical Advisor 2015 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 423. ISBN 9780323084307.
- Gabbe, Steven G. (2012). Obstetrics: Normal and Problem Pregnancies. Elsevier Health Sciences. p. 1146. ISBN 978-1437719352.
- Crum, Christopher P.; Lee, Kenneth R.; Nucci, Marisa R. (2011). Diagnostic Gynecologic and Obstetric Pathology E-Book. Elsevier Health Sciences. p. 430. ISBN 978-1455708956.
- Arora, Mala; Walavalkar, Rajalaxmi (2013). World Clinics: Obstetrics & Gynecology: Postpartum Hemorrhage. JP Medical Ltd. p. 237. ISBN 9789350904244.
- "Sexually Transmitted Diseases & Pelvic Infections". Current diagnosis & treatment : obstetrics & gynecology (11 ed.). McGraw-Hill Education. 2012. p. Chapter 43. ISBN 978-0071638562.
- Mackeen, AD; Packard, RE; Ota, E; Speer, L (2 February 2015). "Antibiotic regimens for postpartum endometritis". The Cochrane Database of Systematic Reviews (2): CD001067.
- Hubert Guedj; Baggish, Michael S.; Valle, Rafael Heliodoro (2007). Hysteroscopy: visual perspectives of uterine anatomy, physiology, and pathology. Hagerstwon, MD: Lippincott Williams & Wilkins. p. 488. ISBN 978-0-7817-5532-0.
- Noakes, David E. (2009). Arthur's Veterinary Reproduction and Obstetrics E-Book. Elsevier Health Sciences. p. 411.
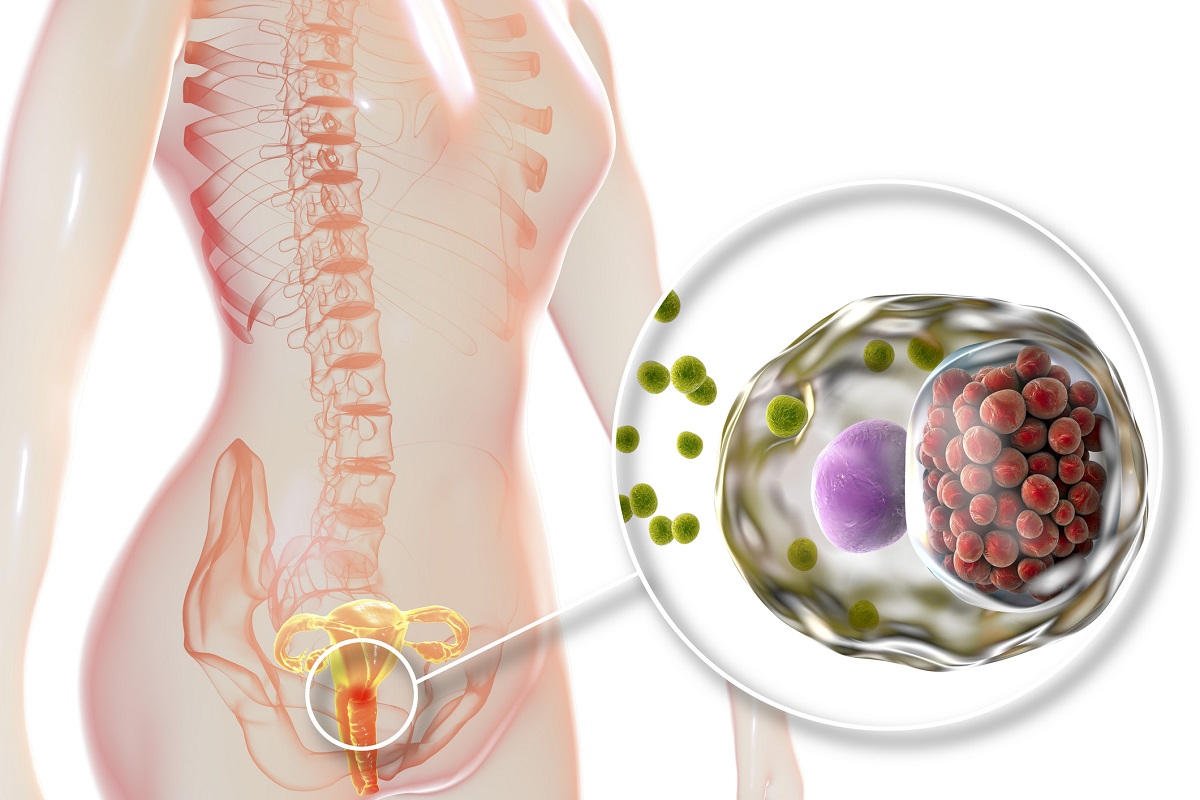
Inflammation of the uterus: Causes and Impact on Fertility

Photo source: Getty images
Most common symptoms
- Malaise
- Abdominal Pain
- Anal pain
- Period pain
- Painful bowel movements
- Lower Abdominal Pain
- Groin Pain
- Painful urination
- Fever
- Increased body temperature
- Nausea
- Constipation
- Flatulence - bloating
- Bloating - flatulence
- Indigestion
- Low blood pressure
- Menstrual cycle disorders
- Smelly discharge from the vagina
- Muscle weakness
- Fatigue
- Vaginal discharge
- Winterreise
- Long menstrual bleeding
- Accelerated heart rate
Show more symptoms ᐯ
Endometritis is treated by
Other names
cervitis, endometris, myometris