Why does shingles occur? What is its most effective treatment?

It interferes with the patient's comfort, causes severe burning pain, manifests itself in ugly, unaesthetic blisters, takes a long time to heal and can leave unpleasant scars anywhere on the body. We are talking about shingles - herpes zoster.
Article content
It is caused by the 3rd human herpes DNA virus. The causative agent is the varicella zoster virus, the so-called VZV virus. It persists in the body as a consequence of chicken pox (varicella).
It normally remains hidden deep in the nerves. If immunity is reduced for any reason, it starts to multiply and comes back to the surface along the nerve fibres as the familiar shingles.
How does shingles form?
Shingles is an acute viral disease caused by the VZV virus that remains in the body after contracting chickenpox in childhood. It is a secondary disease.
The virus is found in the sensory nerves of the basal ganglia, specifically the spinal and cranial nerves. Here it can either remain undetected without manifesting the disease, or it can manifest itself in an outbreak.

Manifestation (manifestation, outbreak) of the disease does not occur in every individual. Only about 10% of the population is affected.
The right conditions need to be in place for the disease to break out.
The main provoking factor is the weakening of the immune system in other chronic infections severe enough, immunodeficiency diseases with the need for immunosuppressive therapy(AIDS), in cancer with cytostatic therapy or chemotherapy, in Hodgkin's disease, lymphoma or diabetes mellitus.
As age increases, the body's defence mechanisms become weaker, which is why shingles is more common in the elderly population.
The risk is almost 50% higher in those over 65 years of age.
However, this does not exclude the occurrence at any age. Various types of radiation are also a provoking factor.
When in contact with a sick person, another person who has overcome chickenpox in childhood with the development of sufficient immunity may become infected only in very rare cases. However, such cases are recorded.
Symptoms of herpes zoster virus in the different stages
Latent stage - no symptoms
This is a period when the patient has no outward symptoms, although the virus is present in the host's body.
Those who overcame smallpox as children and never had herpes zoster during their lifetime had strong enough immunity to suppress it by reactivating the herpes zoster virus.
The latent stage can last for many decades without the virus fully manifesting itself. In most people, however, it never appears.
Prodromal stage

Precedes the active stage itself with blisters. It starts subtly with general weakness, fatigue, muscle, joint and head pain, malaise and a slightly raised body temperature.
The initial symptoms are common to more general illnesses. It resembles, for example, flu symptoms or symptoms of other common infections.
An uncomfortable, local itchiness sets in, which forces the sufferer to start scratching. The more he does this, the more the itchiness turns into soreness, to which it eventually turns anyway.
The pain is at the site where the vesicles later appear. This pain tends to be severe, excruciating or even tingling in intensity. It is burning and tearing in character, with frequent radiating into the surroundings.
It most often occurs in the back on one side and radiates through the side of the chest wall to the ribs or chest. It is often difficult to distinguish at this stage from other diseases presenting with chest symptoms. It may resemble acute myocardial infarction, pleurisy or renal pain (renal colic).
A red erythema (redness) begins to form on the skin in the shape of a band, indicating a transition to the next stage.
Active stage

After the previous prodromal stage, small vesicular blisters appear in the erythema (redness) within 12 to 24 hours.
They act superficially but actually extend into the deeper layers of the skin and mucous membranes.
The blisters are filled with clear fluid containing millions of viral particles and gradually enlarge over the course of a day and cluster into a larger deposit. Some of them may fuse together to form visually larger macules.
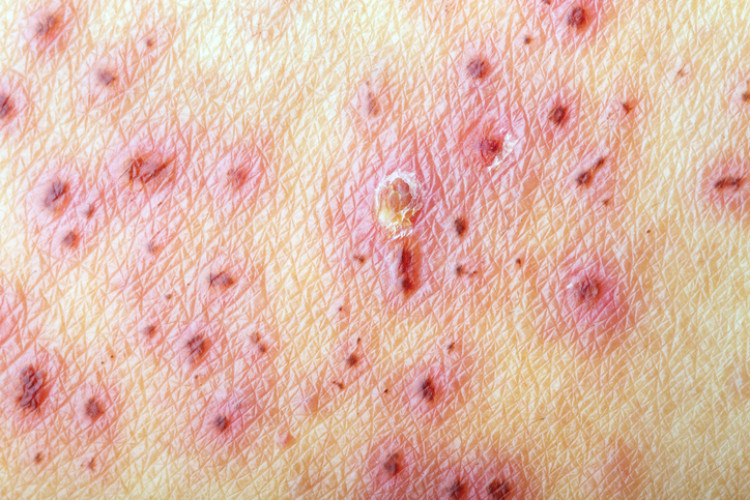
The vesicle may be found separately outside the lesion, but this is rather sporadic. The fluid changes from primarily clear to turbid (opaque) due to the influence of leukocytes.
The whole process is also very painful, and the former unpleasant itching of the skin may occur repeatedly. The affected part of the skin is usually with local swelling and edema in the vicinity of the skin.
The vesicles normally begin to dry up after one week at the earliest. However, this period varies in length.
As they dry out, they turn into brownish-red swollen vesicles, which are also the gateway to secondary bacterial infection.
A red ring forms around the ulcer, making it appear circumscribed.
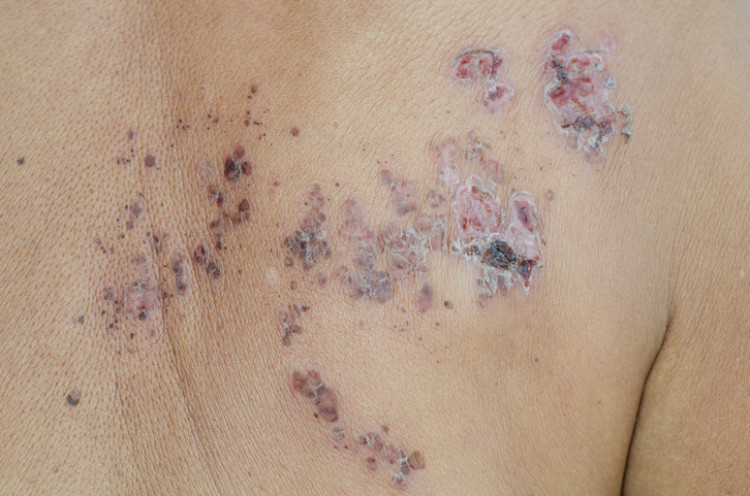
The crust (scab) is initially yellowish in colour, soft and, after its accidental, unwanted detachment, it forms a swollen and very painful wound. It usually begins to bleed slightly. The pain is pulsating.
It is important that the scabs heal without further mechanical damage as they may leave unaesthetic scars.
What complications and sequelae can we expect during and after herpes cure?
Shingles is an unpleasant disease accompanied by pain, but it is not always harmful. One could even say that in most cases it proceeds without consequences or at least major consequences. In rare and more severe cases, they do occur.
Zoster virus and its danger also depend on the place where it is found.
Herpes zoster haemoragicus
Herpes zoster haemorrhagicus is a condition in which the vesicles are not only filled with serum but also partially with blood to form a haemorrhagic (bleeding) exanthema and enlarged lymph nodes. Gangrenous changes are found in the surrounding area and gangrenous herpes develops.
Herpes zoster gangraenosus
The blisters may turn into necrosis (dead tissue). This condition is called herpes zoster gangraenosus. The dead tissue is a breeding ground for bacteria and there is a risk of secondary infection and even life-threatening sepsis.
Herpes zoster oticus
When the ear is affected, it is herpes zoster oticus. The blisters are found in the outer ear and inside the ear. They can also damage the inner ear canal, causing hearing loss of varying degrees, dizziness and facial nerve paralysis.
Herpetic encephalitis
From the ear, they can easily move deeper and be the cause of herpetic encephalitis (inflammation of the brain). A rarer but more serious condition is acute disseminated encephalitis. However, both are life-threatening to the patient.
Herpes zoster ophthalmicus
Herpes zoster ophtalmicus is an affection of the eye specifically the formation of ulcers on the cornea and around the eye to the cheek. This results in various disorders up to complete loss of vision. Spread of the herpes zoster to the face causes paralysis of the facial nerve.
Neuralgia
Pain is not only a symptom during the active phase of shingles, but sometimes persists for months or years after shingles. These are called neuralgias. They have a longer duration of pain, which is why the patient usually seeks medical attention.
How to cope with herpes zoster virus?
Treatment for herpes zoster is not of any use during the latency stage. The virus persists in the body and does not respond to overall virostics at this stage.
It is most effective to start therapy within 72 hours of the onset of symptoms, which is when blisters appear on the body.
Initiated therapy should be completed according to the physician's orders and, in the case of resistant infection or spread of vesicles to the surrounding area, should be continued longer until dry scabs begin to appear. This indicates the healing phase, in which virostics are no longer necessary.
The best known virostatics
Acyclovir - we know it under different names. It is produced in the form of topical creams, but also systemically acting tablets. The cream is applied to the affected area in a thin layer and should not be forgotten also around about 0.5 cm around the vesicles.
In the case of simple herpes such as herpes simplex, treatment is approximately 5 days long. It should not exceed 10 days or more. The cream can be used in pregnant women, nursing mothers and children. Absorption of the drug is minimal and not measurable. However, the oral form (by mouth) of the drug is not recommended in these cases.
Valaciclovir - this is the metabolic precursor of acyclovir. This means that it is converted into acyclovir after it is taken in the body. Once it enters the cells, its concentration in the cells is high.
It is recommended to start treatment as soon as possible. It is not scientifically proven to be less effective after 72 hours. It is very effective in the treatment of shingles. It should be taken for 5 days, maximum 10 days as with acyclovir. If used in time at the first symptoms, it can prevent skin lesions.
Famciclovir - is metabolised in the body to penaciclovir. The generic name famciclovir is also the name under which it is commonly found in the pharmacy. It reaches high serum concentrations when ingested. This means it does not need to be taken as often. One tablet 3 times a day is usually prescribed.
The treatment of herpes zoster with this preparation is more effective and faster if raloxifene is given at the same time, which converts the basic substance in the drug more quickly into penaciclovar. It thus acts as an inhibitor. As regards pregnancy and breastfeeding, there are still not enough clinical studies to confirm the effect of the drug on pregnancy and fetal harm and breastfeeding (lactation).
However, adverse effects are not clearly excluded.
Brivudine - is a very effective prescription virostatic. It is in tablet form and is taken one tablet once a day. Again, initiation of treatment should not exceed 72 hours.
The therapy itself usually lasts 7 days. In more severe and relapsing (persistent) forms, it is necessary to see a doctor and not to arbitrarily exceed the duration of treatment. In general, it is indicated only for short-term treatment.
The preparation is contraindicated (prohibited) in pregnant and lactating women and, due to lack of knowledge and a large number of side effects, is not used to treat children.
What to do for a more serious form of herpes zoster?
Therapy with virostatics alone in severe forms of the herpes zoster virus may not always be enough. The combination of acyclovir with corticosteroids (corticosteroids alone are of no value) brings positive results. They are administered into the muscle or into a vein. They accelerate the course of the disease, improve the treatment, relieve pain.
However, they are not sufficient as an analgesic on their own. In severe pain and neuralgia, it is recommended to add analgesic treatment (pain medication) to the patient.
For pain during the active phase of the disease, ordinary preparations are sufficient. For unbearable pain, tramadol is used. This drug belongs to the opioid class, acts on the central nervous system and, with long-term use, there is a risk of addiction.
Shingles itself, the unpleasant and long course and, last but not least, neuralgia as a painful complication reduce the patient's quality of life.
The more relapses an individual has, the worse the course and the more severe the neuralgia and other consequences, the worse the patient experiences.
In some cases, at least during an outbreak, antidepressant therapy is necessary. It improves the patient's psychological state and alleviates depression, thereby improving the patient's experience.
Related










