- DYLEVSKÝ, Ivan. Functional anatomy. Prague: Grada, 2009. ISBN 978-80-247-3240-4.
- MARTÍNEK, Jan and Pavel TRUNEČKA. Gastroenterology and hepatology in algorithms. Prague: Maxdorf, [2021]. Jessenius. ISBN 978-80-7345-684-9.
- solen.cz - Functional intestinal disorders and their treatment. Solen. Peter Minárik and Daniela Mináriková
- praktickelekarenstvi.cz - Treatment of intestinal inflammation. Practical pharmacy. Jiří Ehrmann, Michal Konečný
- healthline.com - Small Intestine. Healthline editorial team
What functions does the small intestine perform? The most common diseases and symptoms

The small intestine is an important part of the digestive system. It is particularly important for the absorption of essential nutrients into the body. What are all its functions? What are the risk and beneficial factors that affect gut health?
Article content
- Small intestine: basic information
- The small intestine: function and importance in the body
- The small intestine is the second brain (the connection between the intestine and the brain)
- Diseases of the small intestine
- How is the small intestine examined?
- Negative factors for small bowel health
- Favourable factors for the health of the small intestine
In this article you will learn its function, importance, diseases, risk factors, prevention and many other interesting information.
Small intestine: basic information
The small intestine is technically called the intestinum tenue.
It is a tube-shaped organ that anatomically connects the stomach and the large intestine. Two important basic processes take place in the intestinal tract - digestion of food and absorption of nutrients into the body.
The small intestine is divided into 3 contiguous parts:
- The duodenum
- The duodenum (jejunum)
- The ileum
In the duodenum, ingested food meets with digestive juices from the pancreas and bile from the gallbladder. Chemical breakdown of food occurs.
The second part of the intestine, the ileum, provides the highest rate of nutrient absorption. The intestine then transitions smoothly into the ileum, which makes up about 3/5 of the total length of the intestine.
However, in order for the ingested food to move down the digestive tract, the small intestine performs peristaltic movements. By contracting and then relaxing the musculature, the food moves smoothly and mixes with the digestive juices.
The small intestine is richly supplied with blood vessels, lymph and nerves.
You often ask what is the length of the small intestine...
The small intestine is 3-5 meters long. The average width of the intestinal wall is 3-4 centimeters.
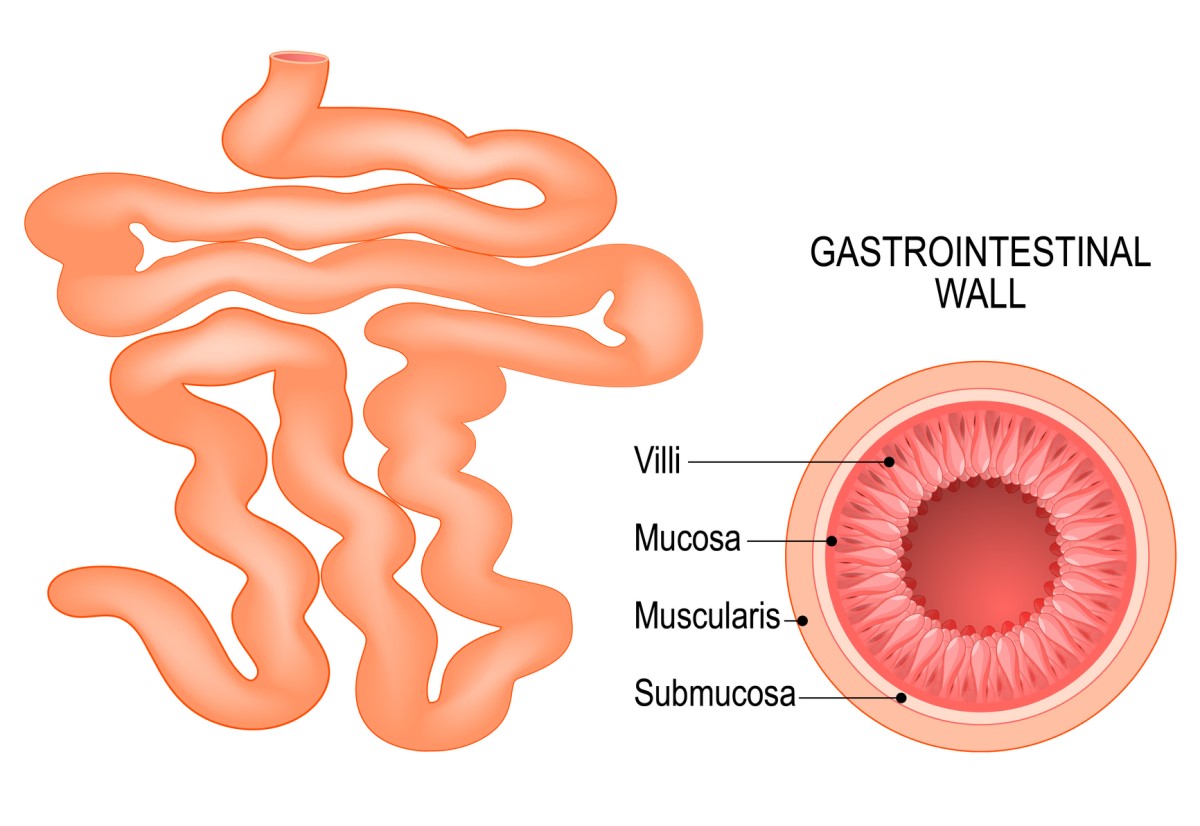
The wall of the intestine consists of 4 layers:
- mucosa
- submucosa
- Musculature
- Membrane (serosa)
- mucosa
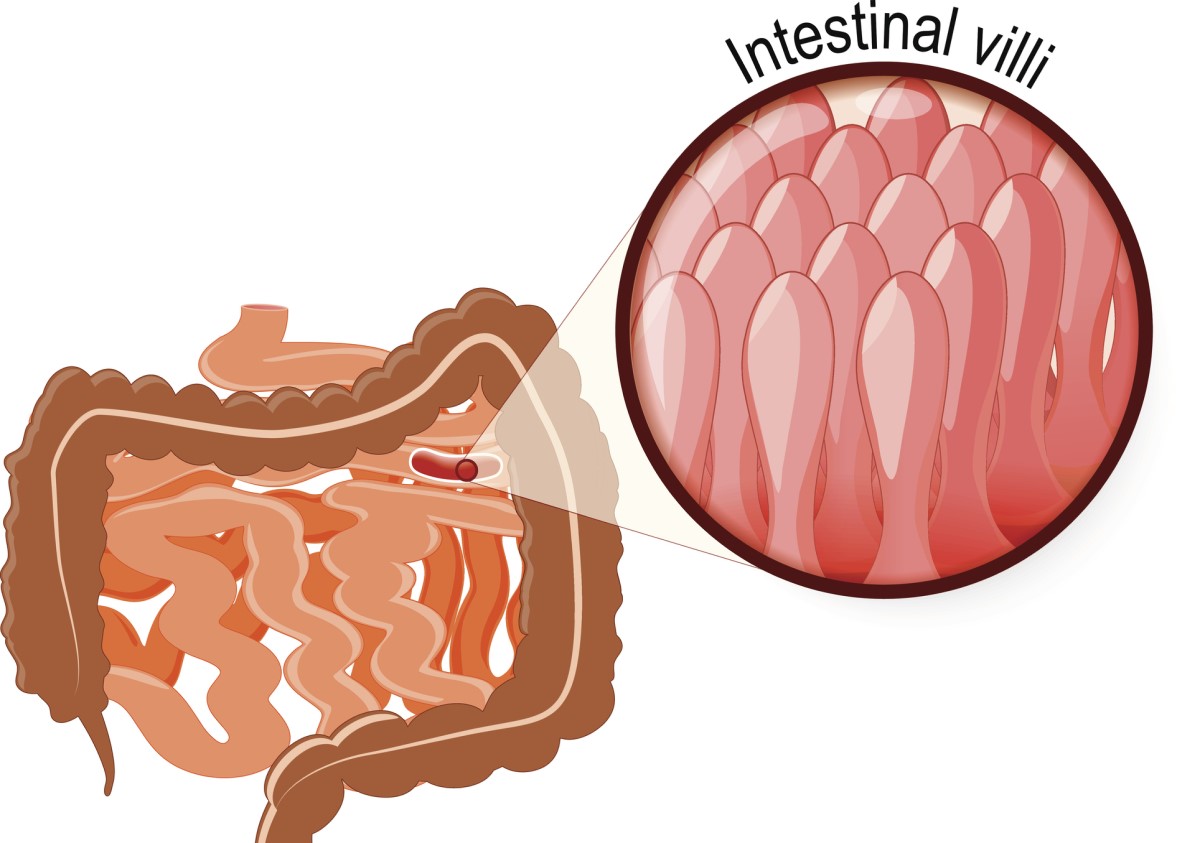
The mucosa of the small intestine is made up of characteristic projections called intestinal villi.
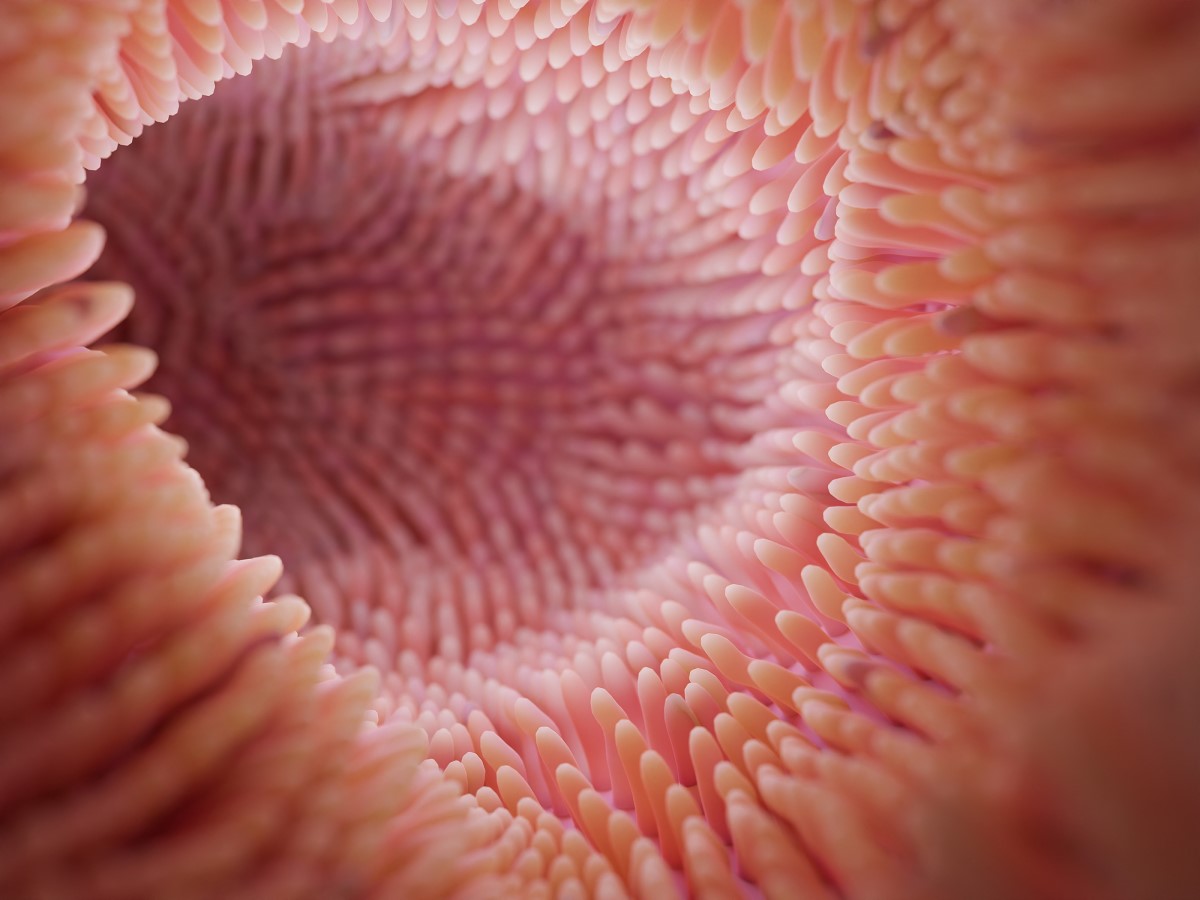
The mucosa of the small intestine is pale pink in colour. The entire surface of the intestinal mucosa is filled with finger-like projections called intestinal villi, which increase the absorptive surface of the intestine.
The villi increase the inner surface and absorption area of the intestinal wall. These special protrusions ensure the absorption of vitamins and minerals into the bloodstream throughout the body.
The mucosa is covered with a specific cylindrical epithelium containing different types of cells:
- Cup-shaped cells forming a layer of protective mucus mucin
- Cylindrical cells enterocytes with the function of absorbing nutrients
- M-cells mediating the connection between the lymphatic system and the small intestine
- Stem cells
- Submucosal tissue
Submucosal tissue, called submucosa, is a layer of sparse connective tissue rich in blood and lymphatic vessels and nerves.
- Muscle
Muscle layer composed of two layers of smooth muscle - the inner circular layer and the outer longitudinal layer.
- Serosa
Serosa (adventitia) is a peritoneal transparent coating (membrane) consisting of a single layer of flat epithelium that covers the organs of the digestive tract externally.
The small intestine: function and importance in the body
As mentioned in the previous section, the main functions of the small intestine are digestion of food and absorption of nutrients into the body.
Partially digested food, technically called chyme, mixes with intestinal juices in the small intestine. Along the way, food is gradually broken down in all parts of the small intestine by digestive enzymes.
Subsequently, these broken down food particles become small enough to pass through the intestinal wall into the bloodstream and thus into the body. Any undigested and unconsumed food particles are moved further into the large intestine.
The main function of the small intestine is the digestion of food debris, absorption of nutrients from food and absorption of water into the body.
The small intestine, due to its connection with the lymphatic system, is an important immunological organ involved in maintaining the immunological balance of the body. It is also the largest endocrine organ in the body.
Functions of the small intestine:
- Digestion of food
- Absorption (absorption of nutrients)
- Motility (motility of the intestines)
- Secretion
- Immunological function
- Endocrine function
The small intestine is the second brain (the connection between the intestine and the brain)
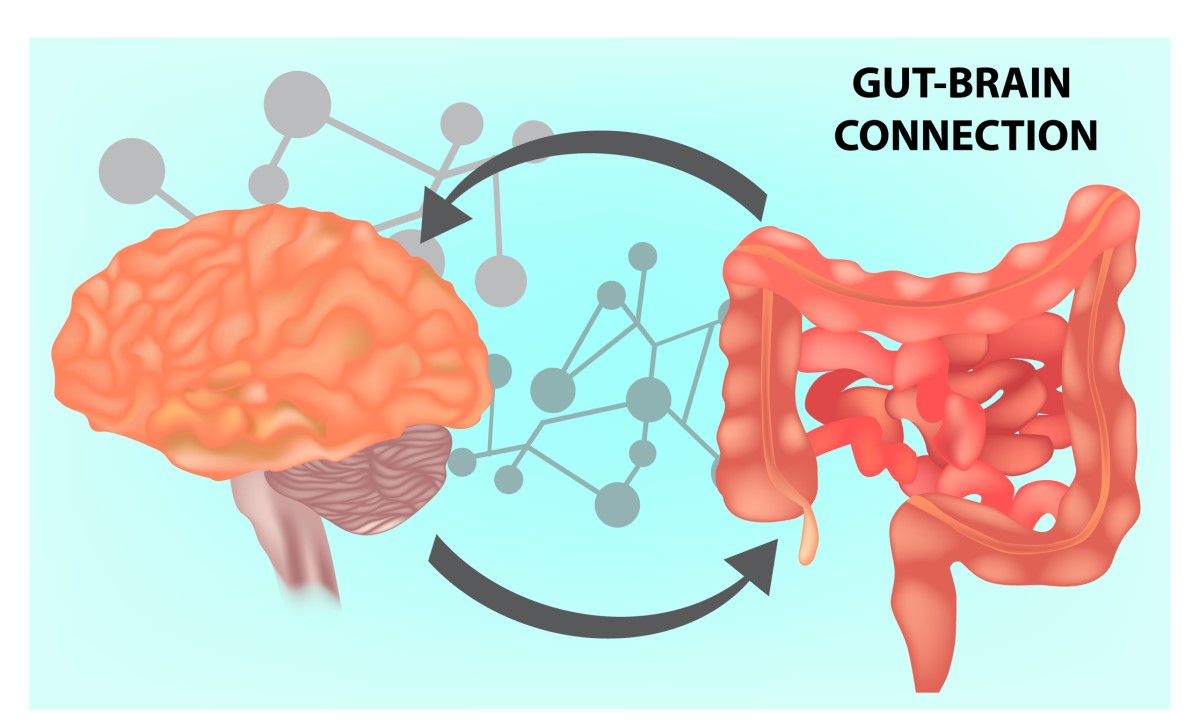
You may have come across the name second brain or gut brain. This name refers to the close connection between the CNS (central nervous system) and the human intestinal tract.
The small intestine contains one hundred million neurons. It is referred to as the enteric nervous system (ENS) or, in layman's terms, the "second brain". The close connection between the brain and the intestinal tract is scientifically proven.
The gut microbiome is the collection of microorganisms that colonize not only the intestinal tract, but the entire human body. These are bacteria, viruses, yeasts, fungi or protozoa that are found in the body. The state of this microbiome plays a significant role in physical and mental health.
Intestinal microorganisms release various substances that enter the brain through several possible routes. The first is through the lining of the small or large intestine into the bloodstream towards the brain.
The second route is via the vagus nerve, which travels from the gut to the brain and vice versa. Through this nerve, the CNS influences the blood supply to the intestinal tract, and higher blood supply also means better absorption of nutrients.
Many scientific studies over the years have shown a high correlation between gut health and the immune system, mental health, mood, autoimmune and endocrine disorders and even cancer.
Diseases of the small intestine
The aetiology of small bowel disease is multifactorial. It can be an inflammatory process caused by infection with pathogens or chronic disability. A common cause of non-physiological bowel function is food allergy and intolerance.
In contrast, cancer of the small intestine is rare within the digestive system.
The following are examples of diseases of the small intestine:
Infectious inflammatory diseases
As with other internal systems of the body, inflammatory processes can occur in the intestinal tract as a result of infection with a particular pathogen. Harmful bacteria, viruses and parasites invade the small intestine.
Intestinal influenza, commonly known as gastroenteritis, is an acute infectious disease affecting the stomach and intestinal tract. It is mainly caused by pathogens in poorly stored, contaminated or uncooked food or water. Infection is transmitted by the faecal-oral route.
These intestinal diseases are mainly accompanied by problems with defecation (diarrhoea), vomiting and increased body temperature - fever.
Diseases of bacterial origin include salmonellosis, cholera, campylobacteriosis, Escherichia coli and shigella. Viruses include the rotavirus group.
In the context of pathogenic infections of the small intestine, professional treatment by a physician is necessary for the complete cure of the infection without health risks and consequences.
Diagnosis is established on the basis of a blood sample. Treatment depends on the specific pathogen, but in most cases includes medical treatment with antibiotics, rest and dietary measures.
Crohn's disease
Crohn's disease most commonly affects the small intestine. It is a chronic inflammatory disease with phases of rest and acute inflammation.
This autoimmune disease causes inflammatory processes in various parts of the intestinal tract, but most commonly in the area of the small and large intestine junction.
Crohn's disease manifests itself in a similar way to food allergies, mainly with bloating, diarrhoea, pain and abdominal cramps. The aetiology of the disease is not fully understood, but the main factor is the improper reaction of the individual's immune system and family history.
Celiac Disease
Celiac disease is also known as gluten enteropathy. It is an autoimmune disease of the small intestine. It is the inability to digest gluten in the intestinal tract. The diagnosis is made by an allergist and a gastrointestinologist.
Lifelong treatment consists of a gluten-free diet. If the patient does not remove gluten from his diet, the intestinal villi may shrink and smooth out. Consequently, there is a risk of the intestinal mucosa being unable to absorb sufficient nutrients and malnutrition.
Food intolerance and allergies
Lactose intolerance is a disease caused by a deficiency of the enzyme lactase, which breaks down milk sugar (lactose). It is therefore a disorder of the digestive tract in the breaking down and processing of milk sugar.
An allergy to milk protein (in most cases cow's milk protein) is a pathological reaction of the immune system. The allergy is therefore related to the consumption of milk protein, not to the consumption of lactose.
It is the intake of lactose or milk protein that causes digestive problems and adverse reactions, including abdominal pain, diarrhoea, bloating and, in the case of allergy, skin manifestations (rash, eczema, itching...).
Histamine is a substance that occurs physiologically in our body. The breakdown of excessive amounts of histamine is carried out by the enzyme diaminoxidase, which is produced in the small intestine. However, if the production of this enzyme is low, histamine intolerance can occur to varying degrees.
Excessive intake of foods high in histamine (tomatoes, cabbage, cheese, pastries...) is a trigger for unpleasant digestive problems.
Oncological diseases
Although digestive tract cancer is common among cancers, small bowel cancer is rather rare.
The most common cancers of the small intestine are adenocarcinoma, carcinoid, sarcoma and lymphoma. However, in addition to malignant tumours, benign tumours also occur in the small intestine.
Genetic factors, family history, celiac disease, chronic intestinal inflammation, a weakened immune system and a long-term unhealthy lifestyle (alcohol, smoking, lack of physical activity, excessive intake of sugar, salt and highly processed foods) increase the risk of cancer.
Symptoms of small bowel cancer are mainly abdominal pain, blood in the stool, general weakness, increased fatigue and weight loss.
How is the small intestine examined?
The initial examination of the intestinal tract involves taking a comprehensive medical history, talking to the patient about clinical symptoms and finally a basic examination by looking, listening and touching.
The basic examination also includes laboratory testing of blood, urine or stool samples. Ultrasound examination of the abdominal organs is a common examination.
In the case of digestive and excretory problems, a colonoscopy imaging examination is performed. In this method, a specially adapted camera is inserted into the patient's rectum. This examination primarily focuses on the colon, but the doctor may also check the terminal part of the small intestine.
A possible endoscopic method is gastroscopy, which again can check the stomach and the beginning of the small intestine. Enteroscopy is a specific imaging examination of the small intestine.
CT enterography (computed tomography) is mainly used in the diagnosis of diseases of the small intestine. The patient is injected with a contrast agent on an empty stomach for a detailed view of the area. Another imaging method is magnetic resonance imaging (MRI). Which specific imaging method the doctor chooses is individual.
An endoscopic capsule is a diagnostic view of a part of the small intestine that cannot be examined by other methods. The patient swallows a small capsule that contains a camera. This capsule then transmits three images per second to an external machine that receives the data coming from the camera as it passes through the intestinal tract.
Negative factors for small bowel health
Risk factors can be divided into intrinsic and extrinsic. Intrinsic risk factors cannot be influenced; extrinsic risk factors can be influenced.
Internal factors include genetic factors, positive family history, autoimmune diseases, allergies, intolerances, advanced age and others.
External factors include inappropriate lifestyle and unhealthy eating habits.
An unsuitable diet means an unbalanced diet low in vitamins, minerals, protein and fibre. On the other hand, excessive intake of simple sugars and saturated fats is harmful.
Refined simple sugars are also an enemy of the gut microbiome. In high amounts, they are associated with the proliferation of yeast, which leads to inflammation in the body.
Consumption of pesticides has a negative effect on the gut microbiota as well as on the hormonal and nervous system. It is therefore advisable to reach for a quality and proven food source.
Alcohol consumption is a risk factor because it increases the amount of harmful bacteria.
Smoking, use of antibiotics and other drugs contribute to an imbalance of bacteria. Frequent use of analgesics negatively affects the intestines and increases the risk of intestinal permeability.
The enemy of the balance of intestinal bacteria is chronic stress. Excessive amounts of stress cause inadequate blood supply to the intestinal area and limit the production of digestive juices.
Negative external factors:
- Incomplete diet
- Alcohol consumption
- Smoking
- Low intake of vitamins and minerals in the diet
- Excessive intake of refined sugar
- Excessive intake of saturated fat
- Low intake of fibre, vegetables and fruit
- Excessive use of certain drugs (antibiotics, analgesics...)
- Excessive chronic exposure to stress
- Low daily physical activity
- Irregular poor quality sleep
- Failure to respect food intolerances
Favourable factors for the health of the small intestine
The health of the gut microbiome can be significantly influenced by an appropriate diet and lifestyle.
We should regularly include fruit, vegetables and whole grain products in our diet. Adequate fibre intake is essential to balance gut bacteria and support digestion.
Fermented vegetables (cucumbers, cabbage) and fermented dairy products (kefir milk) are also suitable. These foods are natural sources of probiotics and prebiotics. Supplementation with probiotics in the form of a dietary supplement is also necessary after overcoming illness and weakening of the intestinal bacterial balance.
Foods that are beneficial for the intestinal tract due to their anti-parasitic effects are garlic, onions, turmeric, chlorella and spirulina.
Sufficient fluids have a beneficial effect on the intestinal mucosa and the balance of beneficial bacteria. These include plain water, herbal tea, mineral water and fresh vegetable and fruit juices.
Clean water should be the basis of the drinking regime.
Elimination of stress factors, sedentary jobs and, on the contrary, regular exercise contribute to proper blood circulation and motility (movement) of the intestines.
Beneficial factors:
- Regular nutritious diet
- Adequate fibre intake
- Adequate protein intake
- Adequate intake of fruits and vegetables
- Adequate drinking and hydration
- Compliance with food intolerances
- Elimination of stress factor
- Getting enough regular and quality sleep
- Sufficient daily physical activity
- Supplementation of probiotics and prebiotics during periods of illness
- Not delaying visits to professional help

Interesting resources










