What can cause inflammation of the uterus?

Inflammation of the uterus, or endometritis, is a less common infection of the female reproductive system. The infection usually enters the uterus from other sites, rarely through the blood. Untreated, it causes serious health problems, including severe pain. It spreads further into the surrounding area and can be one of the causes of infertility or the reason for prematurity (infertilitas) and subsequent miscarriage. It can also develop as a complication after miscarriage or from other causes. What are its most common causes, you can read in the article.
Article content
Inflammation of the uterus occurs in women quite often. To gynecological examination, they are forced to go to pain and unpleasant discharges, which are accompanying symptoms of this disease.
Inflammation affects young women, often after childbirth or miscarriage, but also older women.
The most common causes of uterine inflammation
The inflammatory process in the uterus or transferred to the uterus from the surrounding area is most often caused by bacterial aerobic or anaerobic flora. However, it is increasingly common to encounter chlamydial infections and mycoplasma as the causative agents.
This is due to early onset of sexual life, frequent change of partners, promiscuity and poor hygiene habits.
TIP: Article in the magazine What is the risk of changing sexual partners or what STDs we know
The most common causative agents
- Aerobic bacteria - are bacteria that need at least 10% oxygen to live, grow and reproduce.
- Non-sporulating anaerobes - these are bacteria that need a reduced oxygen tension to grow. They commonly colonise the superficial mucous membranes of the human body. The maximum number of anaerobes is found naturally in the intestine, with a few percent also found in the uterus. Their presence only causes problems if they somehow get into the deeper layers of the mucous membranes, which are normally sterile (surgery, trauma).
- Sporulating anaerobes - are also found predominantly in the gut. The toxins produced by these bacteria play a major role in inflammatory processes.
Recently, the number of chlamydial and mycoplasma infections has been increasing. Chlamydial infections are bacterial infections, also called intracellular parasites. Chlamydial infections are often asymptomatic, but can have a very rich clinical picture.
Mycoplasmas are the smallest and simplest cells ever. They are bacteria that in the past were thought to be the transition between virus and bacteria because of their simplicity.
TIP: Article in STDs in the summer, the dangers of sex tourism
What happens to the uterus during infection?
During the inflammatory process, the uterus is subject to the influence of microorganisms. This can have an impact on the health and later on the fertility of the woman.
The anatomical basis of the uterus
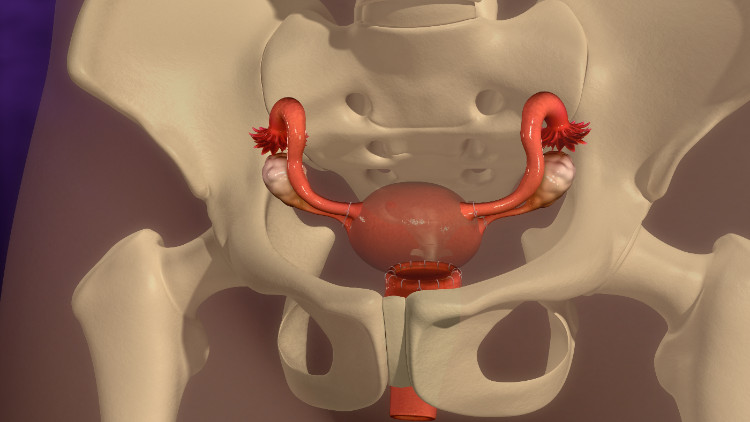
The uterus (Latin uterus) is an unpaired female sex organ shaped like an inverted pear located in the small pelvis between the bladder and bowel with the rectum.
Anatomically, it has two parts. The narrower part is called the cervix uteri and the larger part is called the body of the uterus (isthmus uteri).
It consists of three layers. The inner uterine lining is called the endometrium, the middle layer of muscle is the myometrium, and it is surrounded by connective tissue - the perimetrium.
In inflammation, these layers play an important role, because the inflammatory process can affect only the mucosa or go to the deeper layers of the myometrium to the perimeter. The perimeter is made up of the peritoneum. Therefore, when it is inflamed, there is a risk of peritonitis and transmission of infection to the pelvic organs, which is a very serious, life-threatening condition.
The inflammatory process, the formation and spread of
Inflammation of the uterus is an inflammatory process caused by bacterial flora affecting different layers of the uterus. If it is localised only in the lining of the uterine lining, it is called endometritis. From the endometrium, it can spread deeper to the musculature. When the myometrium is affected, we speak of myometritis.
Inflammation of the peritoneal lining of the uterus is perimetritis.
From there it can spread very quickly to the adnexa (uterine appendages) and the peritoneum. Peritonitis is a very serious complication with unbearable abdominal pain.
Interesting:
This condition can usually be seen in infection caused by Neisseria gonorrhoeae - the causative agent of gonorrhoea. This can cause up to pyometria when the cervix becomes blocked and the uterus subsequently fills with purulent effusion.
As such, endometritis mainly arises ascending (bottom-up) from another site. The most common source of infection is the vagina or cervix. Very rarely, it is haematogenous (blood-borne) and descending (top-down), for example, in pulmonary tuberculosis or other respiratory tract infections (rare).
Infection most commonly occurs during menstruation, iatrogenically after abortion and other intrauterine (IUD) procedures.
How does endometritis manifest itself?

Manifestations vary depending on which layer of the uterus is affected by the inflammation. The clinical picture also varies based on the causative infectious agent and whether complications and involvement of surrounding organs are present.
The course of the disease and its symptoms are highly individual. Depending on the causative infection, they may progress from a completely asymptomatic to a severe painful course with the presence of complications and sepsis.
Basic symptoms common to most endometritis
- The onset of the disease is usually manifested by high fever with chills. The fever is associated with general malaise, weakness and malaise as in most febrile illnesses to complete debility.
- There is initially a mild tightness in the lower abdomen, gradually becoming painful, which intensifies during defecation (emptying) and, due to the anatomical proximity of the uterus to the bladder from the front, there is often pain during urination (dysuria). The pain often radiates to the small pelvis.
- One of the symptoms is obstipation (constipation) and flatulence (excessive gas).
- In the early stages of the disease or in the acute form, dysmenorrhoea, which is heavy and painful menstruation, is common. In the progressive and chronic form of uterine inflammation, the endometrium is gradually destroyed. This in turn results in very light menstruation, leading to amenorrhoea (absence of menstruation) and complete sterility.
- Vaginal discharges are almost always present. Their character, quantity and odour are individual, depending on the causative bacteria. The discharges are watery, with the presence of pus, and finally bloody. For example, in gonorrhoea, discharges that typically smell of fish are common.
Proper treatment cures the inflammation and prevents complications
Endometritis is a consequence of the action of a bacterial infection. The infectious agents that cause it are a wider variety. Therefore, a culture microbial analysis of the cervical flora and an accurate determination of the bacterial species is required. Accordingly, it is necessary to start treatment with antibiotics to which a particular bacterium is sensitive.
Early antibiotic therapy can not only cure uterine inflammation, but also prevent the spread of inflammation to other organs of the female reproductive system.
Analgesics are also useful for pain. More effective are spasmolytics, which relax the muscles of the uterus (relax the cramps) and thus very effectively relieve the pain. Spasmolytics, which are commonly used for menstrual pain, can also be used.
For fevers, antipyretics - temperature lowering drugs - are given.
Estrogens are used to support the regeneration of the endometrium. This is a hormone therapy that acts supportively on the female reproductive organs.
Bed rest and minimizing physical activity are important. The most suitable position for endometritis is supine with the lower legs bent at the knees. In this position, the abdominal wall is relaxed, which helps in pain control.
It is also suitable for other causes of abdominal pain.










