- npz.sk - Hundreds of Slovaks die of pneumococcal pneumonia every year. Despite the fact that it can be prevented
How does pneumonia manifest itself and what treatment is most effective?
When we say treatment for pneumonia, most people think of antibiotics, medicines to make breathing easier and medicines for temperature. Pneumonia is indeed treated with these medicines, but only a part of it. The reason for the wide range of medicines for pneumonia lies in its various causes.
Article content
The treatment of these inflammations is therefore always complicated.
First, it is necessary to identify the underlying cause and then to initiate adequate treatment.
In some cases, treatment can be a problem, as we have seen, for example, in COVID-19.
We categorizepneumonia into two basic units, namely infectious and non-infectious inflammation.
Infectious pneumonia - pneumonia
Infectious pneumonias occur quite frequently. They are caused by various pathogens after they have established themselves in the lung parenchyma.
At the site of attachment, they cause an inflammatory process that spreads further to the lungs. They can affect one or both lung lobes (bilateral pneumonia).
The causative infectious microorganisms are bacteria, viruses, fungi and protozoa, which spread relatively rapidly. The high infectiousness and community spread have placed infectious pneumonia in third place in the population mortality rate.
Also read the magazine article:
Do home treatments and herbs help pneumonia?
Non-infectious pneumonia - pneumonitis
Non-infectious pneumonias are less common compared to infectious ones. They are caused by a non-infectious insult that also causes an inflammatory process on the lung tissue.
Allergens (pollen, dust) and various chemicals (stomach contents - HCl) are considered as triggering agents, which cause irritation of the airways with subsequent inflammation. Non-infectious pneumonia is also triggered by physical causes (radiation, irradiation).
Pneumonia can also be caused by certain medical procedures and treatments. For example, it can occur as a consequence of a medical procedure or as a complication of certain medications.
Pneumonia can kill
Some pneumonias are easier to treat, others are more difficult.
The risk of respiratory failure resulting in death is always high. It is never possible to know in advance how a patient will respond to treatment. We can only assume what will happen.
Several factors influence the success of treatment, namely the speed and time of diagnosis, correct identification of the triggering cause, current treatment options, the age of the patient, his/her general condition and associated burns.
Basic manifestations of pneumonia
- Dyspnoea worsening on exertion and lying down
- predominantly tachypnea (rapid, labored breathing)
- pleural effusion, abscess, empyema
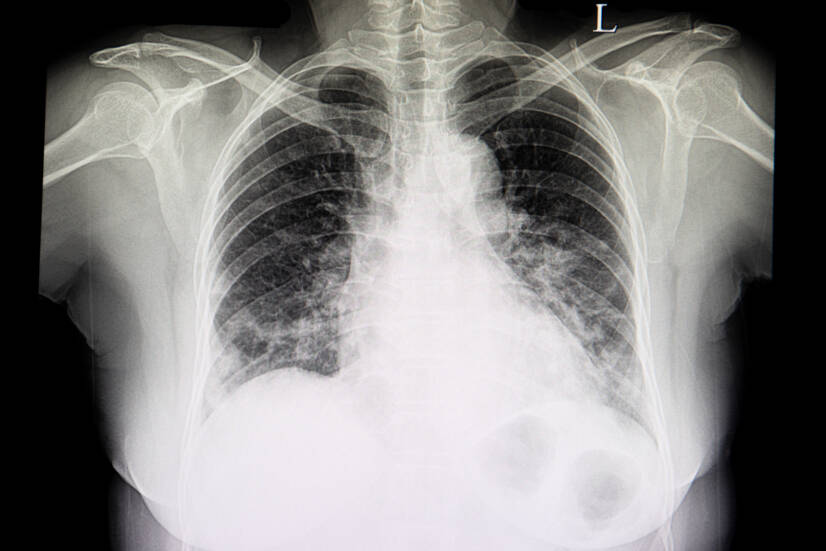
- typical picture of snow-covered lungs on X-ray
- dry cough or wet cough depending on the underlying cause
- chestpain on coughing and later on inspiration
- shivering, chills signalling a rise in temperature
- fever
- malaise, fatigue
- muscle weakness
- headache, dizziness
- pain in muscles, joints, whole body
- appetite
- nausea, vomiting
Predicted prognosis of pneumonia
The chances of survival of a patient with pneumonia decrease with increasing age of the patient (over 50 years), along with associated diseases and comorbidities.
- Late detection of pneumonia with a resistant infectious agent, or an agent for which we do not have an adequate cure, in an elderly polymorbid patient may mean death.
- Early interception of pneumonia caused by a common infectious agent in a young healthy individual, with early initiation of therapy, represents a high chance of recovery.
High risk includes:
- patients over 50 years of age
- polymorbid patients
- Patients with severe disease - heart failure, COPD, asthma, diabetes
- young children
- immunodeficient patients requiring immunosuppressive treatment
- patients with hyposplenia or asplenia
- oncology patients
- cachectic patients with malnutrition
- immobile (recumbent) patients
Read also the articles in the magazine:
Chronic obstructive pulmonary disease. How does it affect the patient's quality of life?
How to get asthma under control and relieve it? A five-point guide
What infectious pneumonias are we familiar with and how to treat them properly?
Infectious pneumonias are technically called pneumonia.
They are caused by an infectious agent, i.e. any living microorganism.
Based on the statistics so far, it is clear that bacterial pneumonias are the leading cause of pneumonia, followed by viral pneumonias. Less frequently, fungal (mycotic) pneumonias and, rarely, protozoal pneumonias, caused by the elements, occur.
Bacterial pneumonia - causes and treatment
Bacterial pneumonia is most commonly caused by the bacterium Streptococcus pneumoniae, one of the so-called pneumococci.
These cause non-invasive pneumonia, but can quickly become invasive and have a high risk of death.
Other agents include Staphylococcus aureus, Legionella pneumophila, Pseudomonas aeruginosa.
Treatment of bacterial pneumonia:
- resting regimen
- drinking regime
- balanced diet
- Adequate intake of vitamins
- antibiotics, especially macrolides (aminopenicillin, roxithromycin, 2nd generation cephalosporins, cotrimoxazole, fluoroquinolones, tetracyclines)
- antipyretics and analgesics (paracetamol, metamizol, acetylsalicylic acid)
- symptomatic treatment to facilitate breathing (antitussives, expectorants)
Interesting:
Due to the increasing resistance of bacteria to antibiotics, especially MRSA strains, there is a call for prevention in bacterial pneumonia.
Vaccination is a basic preventive measure. It is recommended for all, but especially for patients at risk.
We have a 23-valent and a conjugated 13-valent polysaccharide vaccine.
Viral pneumonia, causes, symptoms and treatment
Viral pneumonia is caused by several viruses, most commonly influenza A, B and C.
The most dangerous is influenza A virus, which mutates very often. It is the cause of epidemics and pandemics.
Influenza B virus is more peaceful to the human population. Influenza C virus causes asymptomatic infections.
The most recent to cause pneumonia are coronaviruses, which until recently were known as viruses affecting the upper respiratory tract. Other agents include rhinoviruses, adenoviruses, respiratory syncytial viruses, metapneumoviruses, cytomegaloviruses, herpesviruses, boca viruses, and coxsackie B viruses.
Treatment of viral pneumonia:
- Resting regimen
- drinking regime
- balanced diet
- adequate intake of vitamins
- antiviral drugs (zanamivir, oseltamivir, peramivir, remdesivir)
- antipyretics and analgesics (paracetamol, metamizol, acetylsalicylic acid)
- symptomatic treatment to facilitate breathing (antitussives, expectorants)
- antibiotics in case of secondary bacterial infection
Interesting:
At the moment, the most common antigenic variants of influenza A virus are the H1N1 and H3N2 variants.
However, if a large part of the genome is replaced, new variations could arise, and therefore a new subtype of the virus that we do not know.
Such a change in the genome is called an antigenic jump - the so-called shift.
This could cause another pandemic, which epidemiologists fear more than covida.
Fungal pneumonia, causes, symptoms and treatment
Fungal pneumonias are not very common, so they are usually thought of as a last resort of infectious pneumonias. The exception is protozoal pneumonias, which are usually not thought of at all.
It is characterised by a dry, irritating and prolonged cough. Auscultatory findings on auscultation of the breathing phenomena are mild, and friction murmurs are present. On the other hand, extensive infiltration of the lungs is found on radiographs.
It is caused by fungi such as Candida albicans, Candida tropicalis, Candida krusei or Candida parapsilosis or Aspergillus type fungi. The lung involvement is rarely primary. Most often mycotic pneumonia occurs secondary to another lesion in the body.
Treatment of fungal pneumonia:
- resting regimen
- drinking regime
- balanced diet
- Adequate intake of vitamins
- systemic antifungal drugs (flucytosine, fluconazole, miconazal, ketoconazole)
- macrolide antibiotics for more severe forms (amphotericin B, voriconazole)
- antipyretics and analgesics (paracetamol, metamizol, acetylsalicylic acid)
- symptomatic treatment to facilitate breathing (antitussives, expectorants)
What non-infectious pneumonias are we familiar with and how to treat them correctly?
Non-infectious pneumonias are technically called pneumonitis. They are caused by various factors of non-infectious origin that cause an inflammatory reaction in the lung tissue.
They occur less frequently. But it is not good to forget about them, because they are equally serious. Non-infectious pneumonitis includes mainly aspiration and inhalation, more rarely postradiation, hypersensitivity and eosinophilic.
Aspiration pneumonitis
Aspiration pneumonitis results from acute lung damage due to inhalation (aspiration) of gastric contents. The greater the amount of vomit inhaled and the lower the pH of the vomit, the more severe the damage. If the gastric contents are colonised by microbes, we speak of aspiration pneumonia.
Aspiration pneumonitis occurs mainly in young children, the elderly or in intoxicated individuals (alcohol, drugs). It is less frequently encountered in unconscious patients, after head injuries, stroke or anaesthesia.
In some cases, this pneumonia does not even occur because the patient dies from choking on the vomit. Young people under the influence of large amounts of alcohol or drugs who are left unattended are particularly at risk.
Treatment of aspiration pneumonia:
- aspiration of gastric contents from the airways
- oxygenation, assisted breathing
- in more severe cases with impaired consciousness, intubation, artificial lung ventilation, resuscitation
- hospitalisation in ICU/KAIM
- patient monitoring
- symptomatic treatment
- life support treatment
Interesting:
Every mother worries when her baby eats a scented ariel capsule.
However, fears of intoxication are unnecessary. Liquid washing powder capsules are not toxic.
But what to watch out for?
The capsule melts in the baby's mouth and can foam up.
If the baby inhales the foamy contents into his lungs, he risks aspiration pneumonia!
Inhalation pneumonia
Inhalation pneumonia is caused by inhaling (breathing in) harmful gases and fumes. As a result, the lungs are damaged and their function is impaired. These pneumonias are particularly dangerous. The threat depends on the type of gas, its concentration, the location of exposure and the length of exposure to the person.
Some gases have the ability to displace oxygen (e.g., carbon monoxide, methane), others cause cellular hypoxia (cyanide, hydrogen sulfide) or lead to lung tissue damage (ammonia, cadmium).
They are manifested preferably by respiratory difficulties of varying degrees, coughing and the development of pulmonary oedema. Apart from the respiratory system, they also suffer from headaches, lethargy and, in some cases, disorientation. Nausea or vomiting also occur.
Treatment of inhalation pneumonia:
- Fresh air intake
- oxygenation, if the patient is conscious
- in more severe cases with impaired consciousness, intubation, artificial lung ventilation, resuscitation
- hospitalisation in ICU/KAIM
- patient monitoring
- corticosteroids
- symptomatic treatment
- life support treatment
Less common non-infectious pneumonitis
Less common non-infectious pneumonias include, for example, post-radiation pneumonias.
- Postradiation pneumonia - Arises as a result of radiation therapy near the chest in cancer patients. Corticosteroids are used in treatment.
- Hypersensitivity (pollen) pneumonia - It is caused by iatrogenic lung damage induced by drugs. There are 350 pneumotoxic drugs and the number is increasing.
Interesting resources










