- "Chronic obstructive pulmonary disease (COPD)". Fact Sheets. World Health Organization. Retrieved 1 July 2021.
- Gold Report 2021, pp. 20–27, Chapter 2: Diagnosis and initial assessment.
- Gold Report 2021, pp. 33–35, Chapter 2: Diagnosis and initial assessment.
- Gold Report 2021, pp. 40–46, Chapter 3: Evidence supporting prevention and maintenance therapy.
- GBD 2015 Disease and Injury Incidence and Prevalence Collaborators (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602.
- Gold Report 2021, pp. 4–8, Chapter 1: Definition and overview.
- Myc LA, Shim YM, Laubach VE, Dimastromatteo J (April 2019). "Role of medical and molecular imaging in COPD". Clin Transl Med. 8 (1): 12.
- "ICD-11 - ICD-11 for Mortality and Morbidity Statistics". icd.who.int.
- Martini K, Frauenfelder T (November 2020). "Advances in imaging for lung emphysema". Ann Transl Med. 8 (21): 1467.
- Gold Report 2021, pp. 8–14, Chapter 1: Definition and overview.
- De Rose V, Molloy K, Gohy S, Pilette C, Greene CM (2018). "Airway Epithelium Dysfunction in Cystic Fibrosis and COPD". Mediators Inflamm. 2018: 1309746.
- Ignatavicius, Donna D.; Workman, M. Linda; Rebar, Cherie R. (2022-04-02). Heimgartner, Nicole (ed.). Medical-Surgical Nursing: Concepts for Interprofessional Collaborative Care (9th ed.). Elsevier. p. 573. ISBN 978-0-323-46158-0.
- Ignatavicius, Donna D.; Workman, M. Linda; Rebar, Cherie R. (2022-04-02). Heimgartner, Nicole (ed.). Medical-Surgical Nursing: Concepts for Interprofessional Collaborative Care (9thed.). Elsevier. p.574. ISBN 978-0-323-46158-0.
- "COPD causes - occupations and substances". www.hse.gov.uk.
- Torres-Duque CA, García-Rodriguez MC, González-García M (August 2016). "Is Chronic Obstructive Pulmonary Disease Caused by Wood Smoke a Different Phenotype or a Different Entity?". Archivos de Bronconeumologia. 52 (8): 425–31.
- "Air pollution exposure in cities — European Environment Agency". www.eea.europa.eu.
Chronic obstructive pulmonary disease: Why does it occur and who is at risk?
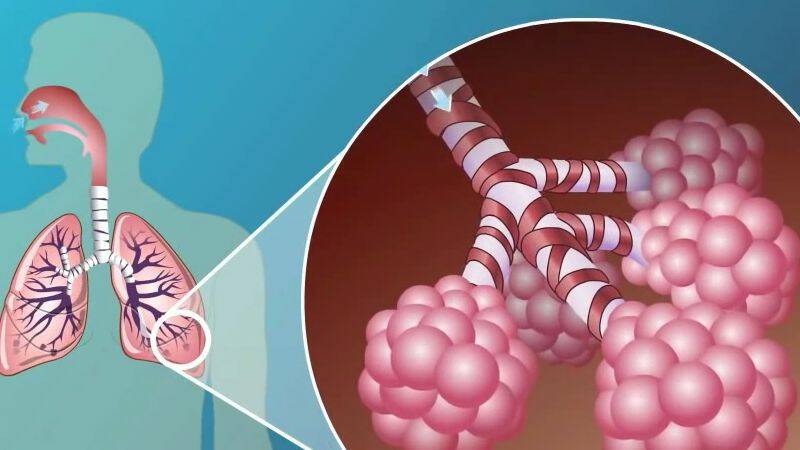
Photo source: Getty images
Most common symptoms
- Malaise
- Chest pain
- Hoarseness
- Spirituality
- Depression - depressed mood
- Blue leather
- Sweating
- Low blood pressure
- Swelling of the limbs
- Disorders of consciousness
- Bone thinning
- Slowed heartbeat
- Dry cough
- Fatigue
- Anxiety
- Damp cough
- Coughing up mucus
- High blood pressure
- Accelerated heart rate
Show more symptoms ᐯ
Treatment of chronic obstructive pulmonary disease
Show morePulmonary disease is treated by
Other names
CHOPCH










