- solen.cz - Impetigo - diagnosis and treatment, MUDr. Táňa Pappová, PhD., MUDr. Andrea Kozárová, PhD., Department of Dermatovenerology, Comenius Medical Faculty in Martin, Comenius University in Bratislava and University Hospital Martin
- solen.cz - Impetigo vulgaris, MUDr. Stanislava Polášková Children's skin outpatient clinic, Dermatovenerology Clinic of the University Hospital of Veterinary and Pharmaceutical Sciences, Prague
- prolekare.cz - Infekce kůže a měkkých tkání, Autoři: R. Gürlich 1; V. Adámková 2; J. Ulrych 3; H. Brodská 4; V. Janík 5; J. Lindner 6; E. Havel 7, Působiště autorů: Chirurgická klinika FNKV a 3. LF Univerzity Karlovy přednosta: prof. MUDr. R. Gürlich, CSc. 1; Klinická mikrobiologie a ATB centrum VFN Praha a 1. LF Univerzity Karlovy primář: MUDr. V. Adámková 2; I. chirurgická klinika VFN a 1. LF Univerzity Karlovy přednosta: prof. MUDr. Z. Krška, CSc. 3; Ústav lékařské biochemie a laboratorní diagnostiky přednosta: prof. MUDr. T. Zima, DrSc. 4; Radiodiagnostická klinika FNKV a 3. LF Univerzity Karlovy zastupující přednosta: MUDr. L. Večeřová 5; II. chirurgická klinika kardiovaskulární chirurgie VFN v Praze a 1. LF Univerzity Karlovy přednosta: prof. MUDr. J. Lindner, CSc. 6; Chirurgická klinika FNHK a LF HK přednosta: MUDr. M. Leško, Ph. D 7
- prolekare.cz - Enzyme treatment of skin and soft tissue infections, Authors.
- praktickelekarenstvi.cz - The most common bacterial skin infections in children, Štěpánka Čapková, Department of Dermatology for Children, University Hospital in Motol, Prague
What is impetigo, what symptoms does it have? Infectivity and transmission in children
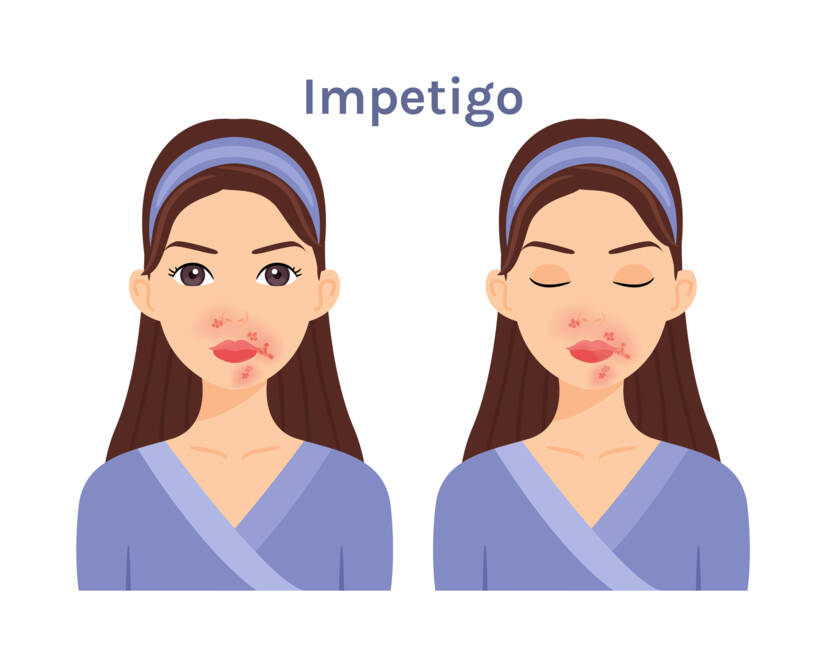
Photo source: Getty images
Most common symptoms
- Fever
- Ulcer
- Scars
- Wetting of the skin
- Blisters
- Buds
- Itchy skin
- Anxiety
- Reddened skin
- Enlarged lymph nodes
Show more symptoms ᐯ
Treatment of impetigo: Topical ointment, systemic drugs and antibiotics
Show moreImpetigo is treated by
Other names
Bacterial dermatitis, impetigo contagiosa, school sores












