- Milo R, Kahana E (March 2010). "Multiple sclerosis: geoepidemiology, genetics and the environment". Autoimmunity Reviews. 9 (5): A387-94.
- "NINDS Multiple Sclerosis Information Page". National Institute of Neurological Disorders and Stroke.
- Nakahara J, Maeda M, Aiso S, Suzuki N (February 2012). "Current concepts in multiple sclerosis: autoimmunity versus oligodendrogliopathy". Clinical Reviews in Allergy & Immunology. 42 (1): 26–34.
- Tsang BK, Macdonell R (December 2011). "Multiple sclerosis- diagnosis, management and prognosis". Australian Family Physician. 40 (12): 948–55.
- McGinley MP, Goldschmidt CH, Rae-Grant AD (February 2021). "Diagnosis and Treatment of Multiple Sclerosis: A Review". JAMA. 325 (8): 765–779. .
- Lane J, Ng HS, Poyser C, Lucas RM, Tremlett H (July 2022). "Multiple sclerosis incidence: A systematic review of change over time by geographical region". Mult Scler Relat Disord. 63: 103932.
- Leray E, Moreau T, Fromont A, Edan G (January 2016). "Epidemiology of multiple sclerosis". Revue Neurologique. 172 (1): 3–13.
- Compston A, Coles A (April 2002). "Multiple sclerosis". Lancet. 359 (9313): 1221–1231.
- Murray ED, Buttner EA, Price BH (2012). "Depression and Psychosis in Neurological Practice". In Daroff R, Fenichel G, Jankovic J, Mazziotta J (eds.). Bradley's neurology in clinical practice (6th ed.). Philadelphia, PA: Elsevier/Saunders.
- Piryonesi SM, Rostampour S, Piryonesi SA (April 2021). "Predicting falls and injuries in people with multiple sclerosis using machine learning algorithms". Multiple Sclerosis and Related Disorders. 49: 102740.
- Mazumder R, Murchison C, Bourdette D, Cameron M (25 September 2014). "Falls in people with multiple sclerosis compared with falls in healthy controls". PLOS ONE. 9 (9): e107620.
- Baecher-Allan C, Kaskow BJ, Weiner HL (February 2018). "Multiple Sclerosis: Mechanisms and Immunotherapy". Neuron. 97 (4): 742–768.
- Lublin FD, Reingold SC (April 1996). "Defining the clinical course of multiple sclerosis: results of an international survey. National Multiple Sclerosis Society (USA) Advisory Committee on Clinical Trials of New Agents in Multiple Sclerosis". Neurology. 46 (4): 907–911.
- Aloisi F, Cross AH (October 2022). "MINI-review of Epstein-Barr virus involvement in multiple sclerosis etiology and pathogenesis". J Neuroimmunol. 371: 577935.
- Ascherio A, Munger KL (April 2007). "Environmental risk factors for multiple sclerosis. Part I: the role of infection". Annals of Neurology. 61 (4): 288–99.
- Huntley A (January 2006). "A review of the evidence for efficacy of complementary and alternative medicines in MS". International MS Journal. 13 (1): 5–12, 4.
- Weinshenker BG (1994). "Natural history of multiple sclerosis". Annals of Neurology. 36 (Suppl): S6-11.
- Berer K, Krishnamoorthy G (November 2014). "Microbial view of central nervous system autoimmunity". FEBS Letters. 588 (22): 4207–13.
Multiple sclerosis: Symptoms, Causes

Multiple sclerosis, or multiple sclerosis is a chronic disease of the central nervous system. It is the most common inflammatory-degenerative disease of the nervous system. It affects approximately 2.5 million people worldwide.
Most common symptoms
- Malaise
- Speech disorders
- Eye Pain
- Frequent urge to urinate
- Depression - depressed mood
- Double vision
- Muscle stiffness
- Defence
- Tingling
- Erectile dysfunction
- Concentration disorders
- Memory disorders
- Swallowing disorders
- Mood disorders
- Muscle weakness
- Muscle cramps
- Itchy skin
- Head spinning
- Tremor
- Fatigue
- Anxiety
- Loss of field of vision
- Constipation
- Blurred vision
- Deterioration of vision
- Decrease in libido
Characteristics
Multiple sclerosis, also called disseminated sclerosis, is a chronic disease of the central nervous system, that is, it affects nerve fibers in the brain and in the spinal cord.
It is the most common inflammatory-degenerative disease of the nervous system and in developed countries it is one of the most common causes of premature disability in the predominantly young population.
It affects approximately 2.5 million people worldwide.
Multiple sclerosis = MS (abbreviation).
Multiple sclerosis is the most common immune-mediated disorder affecting the central nervous system. There are nearly one million people with MS in the United States in 2022, and in 2020, about 2.8 million people were affected globally, with rates varying widely in different regions and among different populations (source: Multiple sclerosis - Wikipedia).
SM has a specific geographical distribution. It is most abundant in the Nordic population, the so-called Caucasian race. On the contrary, it is very rare in the southern areas around the equator and in the black population.
The current migration of populations around the world has produced interesting information when a person moves from his or her original place of residence. Moving out before the age of 15 carries with it the risk of the country in which the person grew up. If the eviction occurred after the age of 15, the risk of SM reflects the country to which the person has emigrated.
Causes
The direct cause that would completely clarify the reasons for the onset of multiple sclerosis is still unclear. The problem is thought to be due to immune system dysfunction caused by multiple triggers, both genetic and environmental.
Environmental factors include, for example:
- geographical latitude,
- untreated and recurrent infections (most commonly Ebstein-Barr virus, causing infectious mononucleosis),
- stress,
- vitamin D deficiency,
- smoking,
- s change in sex hormone levels, especially in the postpartum period, which could explain the higher prevalence in females.
MS is not a congenital disease, and no gene has been proven to transmit the disease. However, genetics does play a role.
Evidence is the increased prevalence in families with MS.
Among first-degree relatives, the risk of being diagnosed with MS is 10 to 50 times higher than in families without the disease.
If one of the identical twins is diagnosed with multiple sclerosis, the risk of the other twin getting the disease is up to 30%.
In order to further discuss the nature of this disease, we should explain a few unfamiliar terms.
Lymphocytes
There are two types.
Types of lymphocytes:
- T-lymphocytes
- B- lymphocytes
T-lymphocytes are white blood cells that are found in the thymus, blood and lymph nodes.
Based on certain recognition signs, they can identify the pest and attack it. They also summon other inflammatory cells to help. This is how inflammation occurs.
B-lymphocytes are formed in the bone marrow. Upon encountering a pathogen, they become plasma cells that form antibodies. These can effectively neutralize it.
Both types of lymphocytes play a role in MS.
Autoimmune disease
The essence of these diseases is that lymphocytes recognize their own tissues as foreign and launch an attack against them.
During the development of an individual, it is ensured that most of the lymphocytes that our own tissue would recognize as foreign are destroyed in time before they travel to the lymph nodes and blood.
Those lymphocytes that have not been strictly selected are put to sleep so that they cannot proliferate. Yet under certain circumstances, their activation occurs.
They can be activated by the various environmental factors mentioned above.
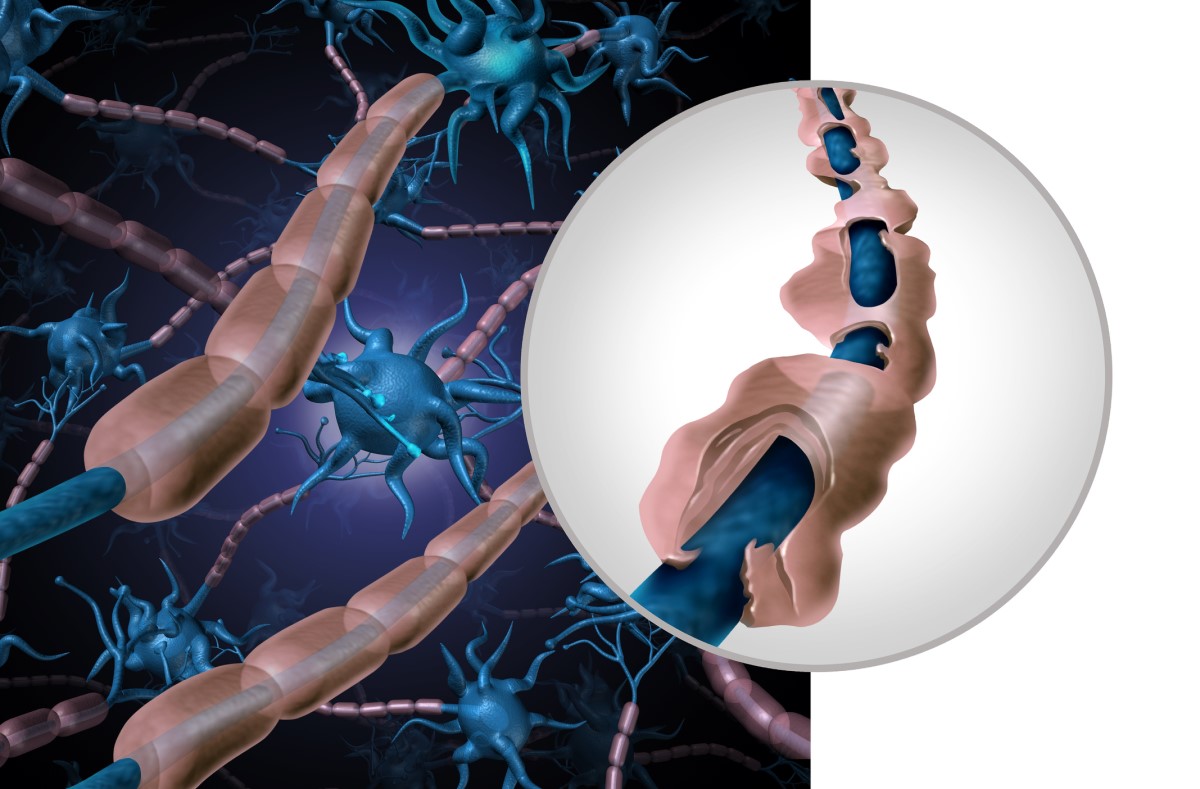
Myelin
Lipoprotein, simply put, the fatty covering of the nerve.
This sheath covers nerve fibres in both the central and peripheral nervous system.
It is a very useful wrapper because, in addition to protection, it also allows for rapid conduction of information in the nerve. With the loss of this sheath, the function of the nerve is also lost.
Nerves in the periphery, for example in the hands and feet, are covered by so-called Schwann cells, in the spinal cord and in the brain myelin is formed by cells - oligodendrocytes.
The path of lymphocytes to the brain and spinal cord
The central nervous system is separated from the rest of the body by the blood-brain barrier (HB), which you can think of as a sieve with very small meshes that allows almost no molecules to pass through.
Such protection ensures that the brain, as one of the most important and sensitive organs, is not penetrated by foreign substances, toxic elements, many drugs, as well as unnecessary inflammatory reactions.
Activated lymphocytes produce inflammatory substances called cytokines, namely IL-2, INF-γ,TNF-α.
These cytokines cause a change in the endothelium of the blood vessels, which becomes "stickier" and so the lymphocytes penetrate the blood vessels more easily. These start to produce proteolytic enzymes that etch the blood-brain barrier, breaking its protective function and entering brain and spinal cord tissue.
Here they trigger an inflammatory reaction.
Subsequently, non-specific T and B lymphocytes penetrate the disrupted HB and can settle there and produce antibodies. Inflammation thus begins to develop.
The role of T-lymphocytes
T-lymphocyte activation takes place in the lymph nodes. Here, the T-lymphocyte encounters the cells that present the pathogen to it. The T-lymphocyte's receptor recognises it, which activates it, and is ready to launch an attack.
Such a triggered T-lymphocyte travels to the central nervous system (CNS), where it causes an inflammatory reaction. The target of autoreactive T-lymphocytes is the myelin sheath of nerve fibres, produced by oligodendrocytes.
The main building block of myelin is myelin basic protein (MBP). Activated T-lymphocytes are directed against it. MBP is similar in structure to EBV, HHV-6, HBV, etc.
Therefore, once lymphocytes in the body have already been activated and directed against these viruses, it is highly likely that the T-lymphocyte will mistake the MBR for a virus and begin to destroy it.
The cytokines summoned to help produce toxic mediators that damage myelin. More and more toxic substances begin to be released from the damaged myelin, promoting inflammation and destroying its surroundings.
The vicious circle of spreading inflammation continues.
The role of B-lymphocytes in the pathogenesis of MS
Their role in the pathogenesis of SM is diverse. They produce antibodies (intracerebral IgG, which are typically oligoclonal), cytokines (pro-inflammatory - TNFα and IL-6 and anti-inflammatory IL-10) and are effective antigen-presenting cells.
Formation of an inflammatory deposit
As the inflammatory reaction is directed against myelin, its destruction occurs in the inflammatory focus.
The inflammatory reaction varies in extent, is usually circumscribed, and there is also damage to nerve fibres and their disintegration.
The mechanism of nerve fiber degeneration, specifically the axon, is not clear.
However, we know that a demyelinated nerve fibre loses its ability to conduct electrical current. The damaged nerve fibre is recognised by lymphocytes, which are able to sever the fibre using so-called perforins.
The amount and distribution of inflammatory deposits, called plaques, is individual.
Typical of MS is the distribution around the cerebral ventricles, i.e. periventricular, where they organize into the characteristic pattern of so-called Dawson's fingers.
Further, they form just below the cerebral cortex - juxtracortical, under the tentorium in the lower regions of the brain or in the region of the cervical spinal cord.
Regeneration of the damaged nerve fibre in the CNS is unfortunately not possible.
There is a lack of growth factors and a rapidly forming scar. The loss of fibres is thus irreversible.
Repair of damaged myelin is only possible in the early stages of the disease. However, the newly formed myelin is thinner and shorter. Repeated inflammatory reactions and destructive processes in the myelin damage the oligodendrocytes, whereby the regenerative capacity of the cell is completely lost over time.
This process leads to permanent disability of the patient.
Symptoms
The acute onset of neurological symptoms is dependent on the site of the lesion at which the demyelination of the neural pathways has occurred and thus determines the corresponding clinical picture.
Visual disturbances as the first symptom of MS
The most common first symptom of SM is optic neuritis.
It is usually manifested by unilateral visual impairment, which may be accompanied by pain behind the eye, or pain when moving the eyes sideways. There are two types of optic neuritis, namely extraocular and intraocular.
Since it is a retrobulbar nerve involvement, i.e. the inflamed and demyelinated nerve is behind the retina, there is a discrepancy between the ophthalmological findings and the patient's discomfort. The patient complains of disturbances in the field of vision, sometimes a feeling of foggy vision or even loss of vision.
However, the ophthalmologist does not see any obvious impairment in the function of the eye during the ophthalmoscope examination.
If demyelination of other cranial nerves, such as those innervating the oculomotor muscles, is ongoing, patients may present with double vision, i.e. diplopia.
Dizziness, balance disturbances, tremors of the limbs, speech disturbances
Involvement of the cerebellum is manifested by impaired coordination of movements.
Also, tremors of the limbs may occur, which patients notice as an inability to perform more delicate movements.
Damage in other parts of the cerebellum, the so-called developmentally older parts, in turn leads to feelings of insecurity in space and problems in maintaining balance.
Patients suffer from dysmetria, which manifests itself by overshooting when aiming, such as the inability to hit the keyhole, when reaching for objects, hitting the eye when touching the face, etc.
Speech disorders include so-called scanning speech, also called explosive or atactic speech, a form of dysarthria, i.e. unintelligible speech.
Weakness and numbness of the limbs, or frequent stumbling
Other symptoms of MS include sensory disturbances and central paresis, or weakness of the limbs associated with spasticity. The pareses can vary in degree from mild weakness on exertion, which you may notice as stumbling when walking for long periods, to not being able to handle normal routes in hiking or sports.
The most severe degree is complete limb paralisis.
Urinary disorders and difficulties in sexual life
For the patient, disorders of sphincter functions are particularly unpleasant.
They don't spontaneously mention them, and many doctors are wary of asking tricky questions that would put a young patient on the spot. Most often this manifests in a urination disorder. These include so-called imperative micturition, that is, sudden urge to urinate with fear of wetting, inability to urinate, frequent and recurrent urinary infections, or urinary incontinence.
Up to 60% of men suffer from erectile dysfunction.
It is the urological-neurological disorders that are among the most serious factors of reduced quality of life in patients with chronic neurological disease.
Gastrointestinal disorders
Serious symptoms include difficulty swallowing, or dysphagia, in which there is a risk of aspiration of the contents of the oral cavity (liquids, food) into the lungs.
Further, patients often suffer from vague sensations in the abdomen, accompanied by cramps or pain. They are associated with impaired bowel function and motility. Obstipation (constipation), diarrhea, fecal incontinence or incomplete defecation are rather common.
About mental healthy and emotional stress in MS
Once diagnosed with Multiple Sclerosis, patients are put into shock.
The doctor cannot explain to them exactly how they got the disease, what they did wrong in their lives, they did not inherit the disease or become infected with it.
Despite this, they are aware of the rapid progression and the need for long-term treatment, which does not cure the disease completely and only slows its progression.
Very often they surf internet portals where they read stories of young people who were confined to a wheelchair shortly after being diagnosed.
At first glance, an unsolvable situation brings anxiety, depression, emotional fluctuations.
In the later stages of the disease, cognitive impairment, difficulties with thinking, memory and behaviour progress.
The situation is aggravated by pathological fatigue, which patients suffer from since the beginning of the disease.
Typical of SM is that fatigue is exacerbated in the heat and, in general, elevated environmental temperature is very difficult for patients to tolerate.
To more effectively monitor disease progression and quantify the disability and severity of SM symptoms, the so-called Kurtzke Expanded Disability Status Scale (EDSS - Expanded Disability Status Scale) was developed.
This scale assesses impairment in seven functional neurological systems.
These are:
- eyesight,
- motor skills,
- cells,
- cerebellar function,
- sphincters,
- sensory difficulties,
- cognitive function
- and fatigue
According to the EDSS number, the doctor decides what type of treatment to choose and monitors how stable the disease is or, on the contrary, whether it is progressing despite treatment.
Diagnostics
The basis of early diagnosis of MS is the early detection of a patient with characteristic symptoms, scheduling the necessary examinations and dispensing the patient in one of the specialised centres for demyelinating diseases.

Magnetic resonance imaging
Magnetic resonance imaging (MRI) of the brain and spinal cord is one of the most telling tests.
This imaging test will show demyelinating lesions called plaques.
The finding is quite typical and includes multiple hyperintense (luminous) foci in typical areas of the brain, most often around the ventricles, under the cerebral cortex, in the brainstem, in the cerebellum, on the optic nerves or in the spinal cord.
It is important to monitor the desaturation of lesions after administration of the contrast agent gadolinium. This so-called enhancement of the lesion is indicative of a fresh lesion, thus demonstrating the acuteness of the disease or attack.
Lumbar puncture
Cerebrospinal fluid examination is an indispensable part of the diagnostic process.
The collection is carried out by lumbar puncture.
Especially young patients are most afraid of this particular procedure. However, its refusal slows down and prevents further diagnosis and, ultimately, treatment.
It is a relatively simple invasive procedure performed by experienced neurologists.
It takes approximately 5-10 minutes and can be performed in the patient's room or in the examination room.
After the procedure, it is important to follow a post-lumbar regimen, which includes 24 hours of bed rest in a horizontal body position, plenty of fluids, and intake of caffeinated beverages or tablets.
In addition to the basic biochemical and cytological picture, laboratory evaluation of the lysate provides evidence of intrathecal synthesis of immunoglobulins (IgG) with isoelectric focusing (IEF). This test, although non-specific, achieves positivity in more than 90% of patients with SM.
An essential factor is the presence of at least two oligoclonal IgG bands, which are present only in the liquor and absent in the serum. This indicates increased lymphocyte activity in the CNS.
A definitive diagnosis of SM must meet the so-called McDonald criteria.
These have been repeatedly revised, most recently in 2017. They describe the so-called dissemination in space and time that marks the progression of the disease.
Dissemination in space means that new demyelinating lesions are present in well-defined locations on MRI images.
Dissemination over time refers to a situation where new demyelinating lesions are present, but in addition are also inflammationally active.
The new definition of the McDonald criteria includes a positive liquor finding, i.e. a demonstrated oligoclonal component or intrathecal synthesis of immunoglobulin type G (IgG), in the dissemination over time. This finding is also suggestive of inflammatory activity present in the CNS.
According to these criteria, a diagnosis of SM can be made at the first magnetic resonance imaging (MRI) scan. On the other hand, it should be noted that there is no 100% reliable test to confirm or exclude the diagnosis of MS.
Examination of evoked potentials
It is an objective and non-invasive diagnostic method used to detect clinically silent CNS lesions.
Evoked potentials are the response of the CNS to a well-defined stimulus in the periphery.
They reflect the quality of the propagation of excitement and information through the neural pathway.
Categorization:
- visual (VEP),
- somatosensory (SEP),
- brainstem auditory evoked potential (BAEP),
- motor-evoked potential (MEP)
In SM, the finding is a slowing of conduction, or a complete block in the transmission of excitement through the nerve pathway, a change in the shape or absence of the typical wave.
Differential diagnosis of MS
There are many non-MS diseases with demyelinating brain changes that can resemble and mimic MS in course and symptoms.
A proper diagnostic conclusion of MS includes the exclusion of these most common diseases:
- Paraneoplastic syndromes,
- tumours of the brain or spinal cord,
- CNS lymphoma
- Discopathy with cervical or thoracic spinal cord compression
- Arteriovenous vascular malformation
- Neuroborreliosis
- Vasculitis of the CNS
- Rheumatoid arthritis
- Hereditary spinal/spinocerebellar ataxias
- Leukodystrophies with adult onset
- Mitochondrial diseases
- Stroke
- Vitamin B12 and folate deficiency
- Celiac Disease
- Hepatitis B
- Fabry disease
- Tyreopatie
- Haematological diseases (thrombophilia, monoclonal gammopathies, antiphospholipid syndrome)
- Post-traumatic demyelination

Course
In the clinical course of SM, the so-called clinically isolated syndrome and definite sclerosis multiplex are distinguished.
Clinical isolated syndrome (CIS) is the very first attack, the first episode of neurological symptoms. It is caused by a demyelinating CNS lesion affecting centres in the brain and spinal cord at the site attributable to the disorder.
These first symptoms must last at least 24 hours.
In most cases, a definitive form of MS develops in the following period, most often a relapsing-remitting form of MS. It is very important to recognize CIS early and, if possible, to start treatment as soon as possible.
According to the course, definitive MS is divided into several forms
1. Relapsing-remitting MS (RRSM)
It occurs in about 85% of cases.
It is characterised by so-called attacks of the disease. After the symptoms subside with acute treatment (most often corticotherapy), the patient's clinical condition is completely or sufficiently corrected. This is followed by a period of varying length without symptoms, called remission.
This phase of alternating attacks with a period of remission lasts about 10 to 15 years.
That can develop into Secondary progressive MS (SPMS).
2. Secondary progressive MS (SPMS)
After each attack, there is only an incomplete recovery, the clinical condition gradually worsens, the impairment of individual neurological areas deepens, and the patient's incapacitation (EDSS number increases) becomes more pronounced.
The diagnosis of SPSM is made retrospectively, based on the presence of progressive worsening after the initial RRSM course.
3. Active primary progressive MS (PPMS)
Approximately 10% of patients experience a steady worsening of their clinical condition since the onset of the disease.
The course goes without attacks, that is, without a period of aggravation and subsequent calm.
Multiple sclerosis (MS) and pregnancy
MS mostly affects young women who are at the peak of the reproductive period. Therefore, it is natural that patients are interested in the course of pregnancy, how the disease affects pregnancy, six months or lactation.
One of the main issues is the compatibility of pregnancy with MS treatment and the feasibility of delivering a healthy newborn.
MS disease alone does not increase the risk of complications during pregnancy.
Ongoing treatment may pose a risk, so any patient with disease-modifying therapy (DMT) should prefer a planned pregnancy and consult her neurologist beforehand.
In the past, pregnancy was not recommended for MS patients because of the increased risk of relapse.
Currently, according to some authors, pregnancy is considered more of a protective factor for disease progression. This is explained by the so-called fetomaternal immune tolerance.
The activity of pro-inflammatory Th1 lymphocytes and the activity of anti-inflammatory Th2 lymphocytes is attenuated.
There were no significant differences in pregnancy duration, fetal thriving, or newborn birth weight in pregnant women with MS. The actual type of delivery, whether natural or cesarean, depends on the neurological and gynecological findings of each patient.
The use of epidural anesthesia is not contraindicated.
The riskiest period for relapse occurs 3-6 months after delivery.
As high levels of prolactin, which has a pro-inflammatory effect and increases the risk of relapse, are persistent during this period, breastfeeding for more than 4 months is not recommended.
From the 6th month postpartum, the woman should restart DMT she was taking before pregnancy.

MS and vaccination
Vaccination is an important milestone in human history and has an irreplaceable place in the prevention of communicable infectious diseases. Therefore, the question of the appropriateness of its use in diseases with autoimmune features, such as MS, arises.
Weighing risk versus benefit comes first.
Vaccination with vaccines that contain non-viable strains does not pose a high risk of adverse effects. In contrast, vaccines with live attenuated (weakened) microorganisms may carry the potential for infection in people with weakened immune systems.
DMT drugs used in the treatment of MS may reduce the effectiveness of the vaccine or may increase the risk of infectious complications.
Therefore, vaccination should be approached with caution, individually assessing the patient's condition, immune profile and disease activity. If vaccination is necessary, the use of non-live vaccines is recommended.
If a severe relapse occurs, it is necessary to wait at least 4-6 weeks for a period of remission.
How it is treated: Multiple sclerosis
How is multiple sclerosis treated? The sooner the better...
Show moreMayo Clinic Explains Multiple Sclerosis
Multiple sclerosis is treated by
Other names
Interesting resources
Related










