- ČÁP, Petr and Ondřej RYBNÍČEK. Allergology in your pocket. Prague: Mladá fronta, 2019. Aeskulap. ISBN 978-80-204-5255-9
- solen.cz - Lactose intolerance - a practical approach. Solen. MUDr. Kateřina Bajerová, Ph.D.
- solen.sk - Food allergy. Solen. Hana Kayserová
- healthline.com - Dairy Allergy vs. Lactose Intolerance: What's the Difference? Healthline. Ariane Lang, BSc, MBA
Milk allergy and lactose intolerance: difference and symptoms

Consuming milk and lactose can cause health problems, especially digestive problems. What is the difference between milk allergy and lactose intolerance? What are the symptoms of dairy intolerance?
Characteristics
The causes of intolerance, symptoms, manifestations, the difference between allergy and intolerance, treatment options and much more can be found in the article.
What is milk and lactose?
Milk is a white opaque liquid that comes from the mammary glands of mammals. It is an important source of necessary nutrients for newborns. In adulthood, milk from animals, especially cows, is often consumed.
Milk is made up of water, fat, protein, vitamins, minerals and lactose. Lactose is the technical name for milk sugar, which is a natural component of milk. It is the main source of carbohydrates in the fluid of milk.
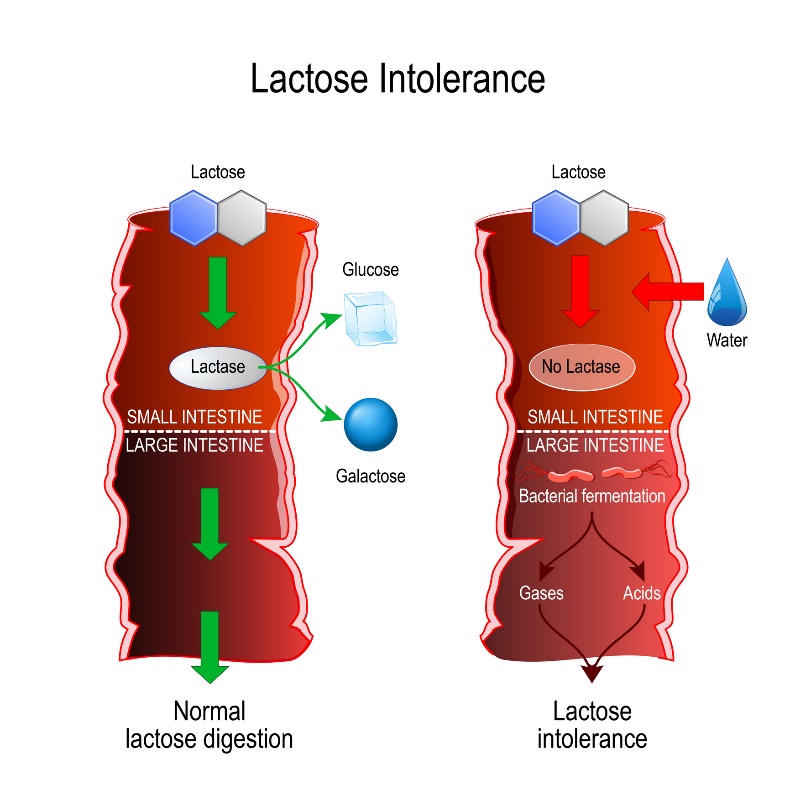
Lactose is broken down in the human small intestine by the enzyme lactase into the individual monosaccharides glucose and galactose.
Causes
Allergy to milk protein
An allergy to milk protein (in most cases to cow's milk protein) is an adverse reaction of the immune system. The allergy is therefore related to the consumption of milk protein and not lactose (milk sugar).
However, this food allergy is not only related to cow's milk. It can also involve other types of milk (sheep, soy...).
However, cow's milk contains a protein called casein, which in most cases is behind the allergic reaction. That is why this allergy is also known as cow's milk protein allergy.
Milk food allergy affects approximately 2% of young children at the level of infants and toddlers. In most cases, the medical condition gradually adjusts to physiology.
Infants do not have a sufficiently developed mucosal barrier at this time of development, which also accounts for the increased permeability to the allergen in its basic form.
On the other hand, in adults, this food allergy is more rare and lasts for the rest of life, as do other types of allergy.
The main symptoms of cow's milk protein allergy are digestive problems such as abdominal pain, bloating, defecation (diarrhoea/constipation), nausea or vomiting.
As this is an allergy, skin symptoms in the form of eczema, rashes, dermatitis, inflammation of the oral cavity, etc. are also possible. Sneezing (runny nose), itchy nose and eyes are also common symptoms.
Adverse allergic symptoms appear relatively quickly after consuming a dairy product.
Lactose intolerance
Lactose intolerance is not an allergy to milk, despite similar symptoms after consuming it. It is an impaired ability of the digestive tract to break down and process milk sugar - lactose.
Individuals with intolerance therefore have a problem with the digestive enzyme lactase.
Poorly processed or unsplit lactose passes from the small intestine into the large intestine. Fermentation then occurs in the large intestine, which promotes intestinal bacteria, fatty acid and gas production.
The increased osmotic pressure increases water retention in the intestine. Lactose is thus fermented by intestinal bacteria to form gases (hydrogen, carbon dioxide) and short-chain fatty acids.
The main symptoms are abdominal pain, abdominal cramps, bloating, flatulence, nausea, problems with defecation (diarrhea), etc.
Lactose intolerance is divided into:
- Congenital/developmental
- Primary
- Secondary (associated)
The congenital form of lactose intolerance is rare and occurs as early as neonatal age. The function of the lactase enzyme is impaired by a genetic factor and persists for the rest of the individual's life.
The symptom is poor tolerance of breast milk and associated digestive disorders. If the condition is not recognised in time, it can be dangerous for the baby. Thus, malnutrition from lack of fluid and nutrient intake is imminent.
Developmental intolerance occurs especially in some cases of premature newborns who do not have a sufficiently developed intestinal mucosa. Physiologically, they begin to form lactose only after the 34th week of a woman's pregnancy.
Secondary associated lactose intolerance is associated with certain disorders and diseases of the individual's digestive system. These are mainly inflammatory diseases of the digestive tract such as celiac disease, Crohn's disease, ulcerative colitis, gastroenteritis and others.
Most secondary intolerances are caused by damaged cells in the small intestine. Health problems with lactose processing can sometimes arise from surgery or trauma to the intestinal tract.
Sometimes the intolerance is triggered by an acute infection, but in this case it usually returns to normal after the cause is removed.
Primary milk intolerance is reported to be the most common form of intolerance. It is a consequence of ageing. As a person gets older, his lactase activity decreases.
This type of intolerance is particularly common in individuals with Asian, African or Hispanic roots and is also due to the evolutionary development of the diet in those regions.
Symptoms
Summary of symptoms in lactose intolerance:
- Bloating, flatulence
- Pain in the abdomen
- Feeling of fullness
- Cramps in the abdomen
- Difficulty defecating (diarrhea/constipation)
- Nausea
- Feeling like vomiting
- Vomiting
Diagnostics
The diagnosis of food allergy to milk consists mainly of taking a blood sample from the patient and laboratory testing to detect specific IgE antibodies against cow's milk protein.
An integral part of the diagnosis is the elimination of the potential food component causing the adverse symptoms. In the context of milk allergy, this includes all dairy products (yoghurt, cottage cheese, ice cream, flavourings and many other "hidden" dairy foods).
If the negative symptoms gradually disappear during a food elimination test and, on the contrary, reappear after the introduction of dairy products, the diagnosis is confirmed.
Unlike milk protein allergy, milk intolerance does not require such a strict diet with complete exclusion of milk from the diet.
In most cases, individuals with lactose intolerance can tolerate small amounts of certain specific dairy products without consequences. However, it should be noted that each person has an individual perception of lactose tolerance.
Currently, the market offers a number of lactose-free dairy products, referred to as 'lacto-free' or labelled with a crossed-out milk symbol.
Lactose intolerance can also be detected by a hydrogen breath test. This is an analysis of the breath after consuming lactose.
The digestion and fermentation of lactose (milk sugar) produces hydrogen, which is absorbed by the intestinal tract and then exhaled through the lungs - the mouth. However, the test is more time-consuming and may be distorted by certain drug treatments given to the patient.
Another diagnostic option is to determine the pH acidity of the patient's stool sample. The amount of undigested lactose is examined in the laboratory. A more invasive method is histochemical examination of lactase enzyme activity in a sample of the intestinal mucosa.
How it is treated: Lactose intolerance
Treatment of lactose intolerance: medication or diet?
Show moreLactose intolerance is treated by
Other names
Interesting resources










