- sgssls.sk - GASTROENTEROLOGY FOR PRACTICE
- emedicine.medscape.com - Chronic Pancreatitis
- healthline.com - Chronic Pancreatitis
- medicalnewstoday.com - What to know about chronic pancreatitis
- ncbi.nlm.nih.gov - Chronic Pancreatitis
- pmj.bmj.com - Diagnosis and management of chronic pancreatitis
Chronic pancreatitis: what are its symptoms, causes? What irritates the pancreas?

Chronic pancreatitis is a chronic inflammation of the pancreas that worsens over time. It causes permanent damage to the pancreas.
Most common symptoms
- Shoulder Blade Pain
- Pain under the left rib
- Stomach pain after a meal
- Abdominal Pain
- Pain under the right rib
- Frequent urination
- Nausea
- Diarrhoea
- Bloating - flatulence
- Indigestion
- The Island
- Fatigue
- Water in the abdomen
- Vomiting
- Yellowish skin
- Increased blood sugar levels
Characteristics
The patient experiences intermittent attacks of severe pain, often in the mid-abdomen or upper left abdomen. Sometimes they radiate in a band-like pattern. Sometimes they are localized to the mid-back.
The pain may occur either after a meal or independently of a meal. It is neither short-lived nor transient, but usually lasts at least several hours.
The pancreas - the forgotten organ in the abdomen?
Not at all.
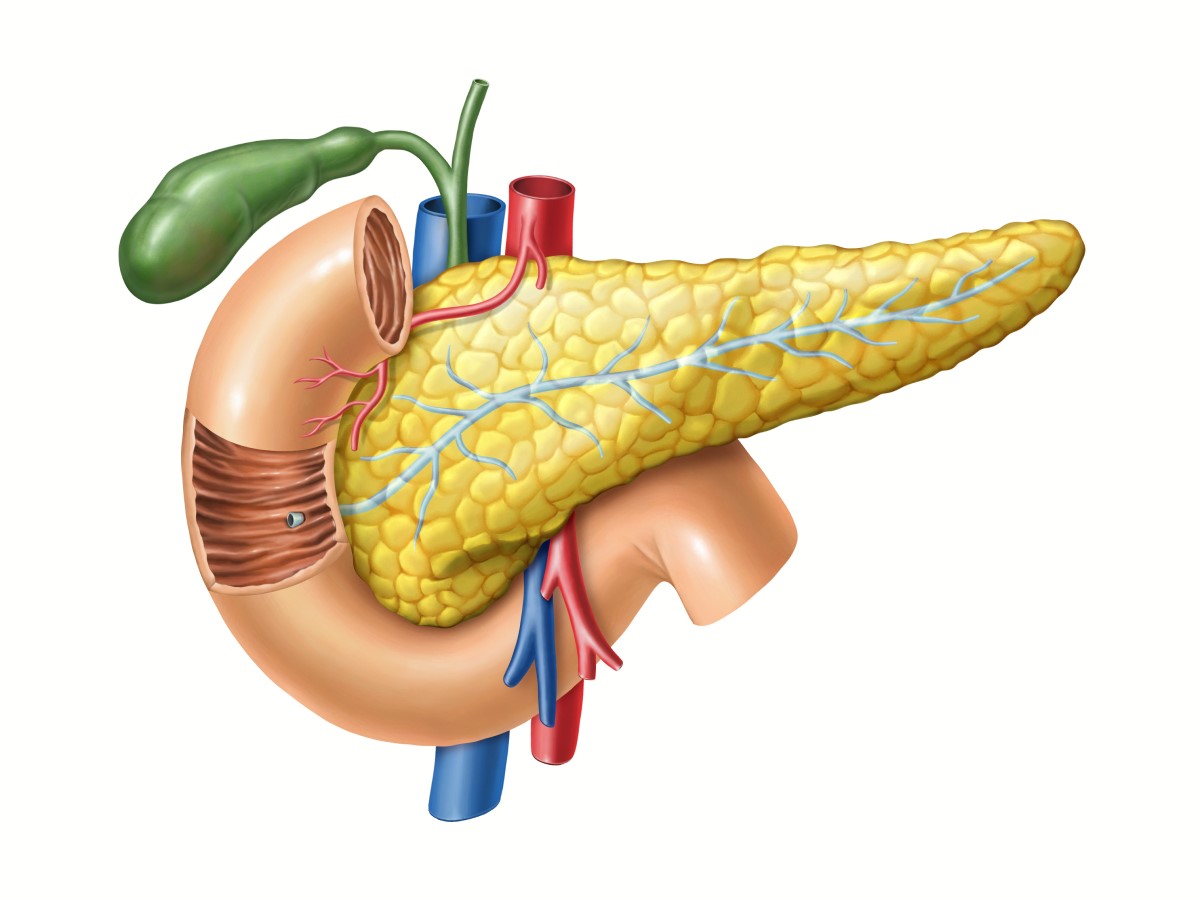
The pancreas is a gland about 15 cm long, located in the abdomen. It is shaped like a flat pear and is surrounded by the stomach, small intestine, liver, spleen and gallbladder.
The wide end of the pancreas on the right side of the body is called the head. The middle part is the body and the thin end of the pancreas on the left side of the body is called the tail.
The pancreas is both an exocrine gland (produces digestive enzymes needed to break down nutrients) and an endocrine gland (produces the hormones insulin and glucagon, which are needed to maintain proper sugar levels).
Causes
Alcoholism: a common problem in families? Causes, symptoms and stages
In children, the most common cause is cystic fibrosis.
Less common causes include:
- Smoking
- immune system attacking the pancreas (autoimmune chronic pancreatitis)
- an inherited defective gene that prevents the pancreas from functioning properly
- injury to the pancreas
- gallstones blocking the pancreatic ducts
- radiotherapy to the abdomen
- high levels of calcium in the blood, which is called hypercalcaemia
- high levels of triglyceride fats in the blood, which is called hypertriglyceridaemia
- medicines

In some cases, the cause cannot be identified. This is called idiopathic chronic pancreatitis.
Alcohol in chronic pancreatitis
Excessive alcohol use is the most common etiology associated with chronic pancreatitis. It accounts for approximately 65% of all cases.
It is most common in men in their fifth and sixth decades.
There is an association between alcohol consumption and pancreatitis, and a monotonically increasing relationship between dose and pancreatic damage has been found.
The relationship between alcohol dose and response in the form of chronic disease tends to vary by gender. Women have a higher risk at comparatively lower levels of intake.
The pathomechanism of alcohol-induced pancreatic damage is not fully understood. One theory suggests that oxidative stress induced by alcohol metabolites directly damages the gland.
There is a strong association between alcohol abuse and pancreatitis. However, a relatively small number of individuals who abuse alcohol develop chronic pancreatitis. This fact suggests that alcoholic pancreatitis is not caused by alcohol abuse alone.
A number of mechanisms by which ethanol and its metabolites damage pancreatic cells are currently debated. Several factors are thought to be involved in the pathogenesis, including genetic predisposition, high lipid diets, cigarette smoking and infectious agents.
Symptoms
It is perceived as a burning or shooting pain that comes and goes. But it can last for hours or days. Although the pain sometimes comes after eating, often food is not the trigger. Some people may feel sick and vomit.
As the condition progresses, painful episodes may become more frequent and severe. Eventually, constant dull pain may develop between episodes of severe pain.
This is most common in people who continue to drink alcohol after being diagnosed with chronic pancreatitis. After quitting drinking and smoking, the pain may ease.

Advanced chronic pancreatitis
Other symptoms develop when damage to the pancreas progresses. The pancreas is unable to produce digestive juices that help break down food.
The absence of digestive juices means that it is more difficult to break down fats and some proteins. This can make the stool very smelly and greasy and difficult to flush down the toilet.
The pancreas does not usually lose these functions until many years after the first symptoms appear.
Other symptoms of chronic pancreatitis:
- Weight loss
- loss of appetite
- yellowing of the skin and eyes (jaundice)
- symptoms of diabetes - such as feeling very thirsty, needing to urinate more often than usual and feeling very tired
- persistent nausea and vomiting, diarrhoea
- bloating
Diagnostics
- you have a history of acute pancreatitis that returns or does not improve
- you have symptoms of chronic pancreatitis
- your doctor examines your abdomen and asks about your history of alcohol consumption and any family history of pancreatic disease or cystic fibrosis
Blood tests
The blood is tested for levels of two pancreatic enzymes, amylase and lipase. However, these are not typically elevated in chronic pancreatitis, unlike acute pancreatitis. Other tests may show gallbladder damage.
Blood calcium and lipid levels are also investigated. If autoimmune pancreatitis is suspected, antibodies are tested in the blood. Genetic testing for cystic fibrosis should be performed in children.
The most sensitive parameter in the diagnosis of chronic pancreatitis is the examination of elastase in the stool.
CT scan
This test produces a 3D image of the pancreas using X-rays and a computer. The examination will describe in detail the size and structure of the pancreas and any morphological changes.
Ultrasound of the abdomen
This test uses sound waves to produce an image of the pancreas. It is always the standard test for diagnosing chronic pancreatitis, although it can pick up advanced chronic pancreatitis.
Endoscopic ultrasound
This test uses a long thin tube (endoscope) that is inserted through the mouth into the stomach and upper intestine.
Ultrasound at the end of the endoscope takes pictures of the pancreas and bile ducts. It is more sensitive than conventional abdominal ultrasound. It is one of the most specific tests for diagnosing chronic pancreatitis.
During the examination, it is also possible to take a sample of pancreatic tissue with a fine needle followed by histological examination to definitively confirm the diagnosis.
ERCP
Endoscopic retrograde cholangioscopy is an endoscopic examination in which the pancreatic and biliary ducts are visualized using a contrast agent and X-rays. It is used for diagnosis but also for therapeutic interventions.
MRCP
Magnetic resonance cholangiopancreatography. This examination takes images using radio waves, a strong magnet and a computer. Imaging of the biliary and pancreatic ducts occurs after injection of a contrast agent.
It is a very sensitive method for imaging the pancreas, pancreatic and biliary ducts.
Complications of chronic pancreatitis
Chronic pancreatitis damages the cells of the pancreas. It also affects those that produce insulin. It can cause the following complications:
- an acute flare-up of inflammation that keeps coming back
- long-term (chronic) pain that reduces the individual's quality of life
- stress, anxiety, depression
- diabetes mellitus (diabetes) - occurs when the cells that produce insulin are damaged
- calcification of the pancreas - this means that the pancreatic tissue hardens from deposits of calcium salts
- gallstones
- kidney failure
- accumulation of fluid and tissue debris (pseudocysts) in the pancreas
- pancreatic cancer - the likelihood of pancreatic cancer is higher in patients with chronic pancreatitis than in healthy individuals, but is still low
How can I prevent chronic pancreatitis?
The best way to prevent chronic pancreatitis is to drink alcohol in moderation or not at all.
Moderate drinking is considered to be no more than 1 alcoholic drink per day for women and 2 alcoholic drinks per day for men.
Quitting smoking is also very helpful.

Living with chronic pancreatitis
People with chronic pancreatitis should follow certain lifestyle changes:
- not drinking alcoholic beverages
- drink plenty of water
- not smoking
- avoid caffeine
- following a healthy, low-fat diet
- eating smaller meals more often - about 5 meals a day
How it is treated: Chronic pancreatitis - long-term inflammation of the pancreas
Treatment of chronic pancreatitis: drugs, diet or surgery and more
Show moreChronic pancreatitis is treated by
Other names
Interesting resources










