- healthline.com - Arthrosis vs. Arthritis: What’s the Difference?
- medicinenet.com - Medical Definition of Arthrosis
- biomag-medical.com - Arthrosis of the Knee
What is arthritis, what are its causes, symptoms and degrees? How to prevent it?

Osteoarthritis is a disease of the joints that is caused by several factors, known also as osteoarthritis. Genetics, age, and associated diseases play an important role. It is the most common joint disease and also a frequent cause of medical examinations.
Most common symptoms
- Headache
- Joint Pain
- Limb pain
- Leg Pain
- Heel Pain
- Shooting pain in fingers and toes
- Pain that Radiates into the Shoulder
- Groin Pain
- Pain under the Right Shoulder Blade
- Back Pain
- Bone Pain
- Swollen fingers
- Tingling
- Bone thinning
- Fatigue
Characteristics
Worldwide, 3.6% of the population suffers from this disease. For the ages of over 65, changes in X-ray examinations are present in up to 60 percent. The disease affects both men and women.
The World Health Organization states that arthritis is the 4th most common cause of incapacity for work in women and the 8th most common in men.
It was considered to be due to aging and degeneration due to joint wear and tear.
However, this statement is not accurate, because, several factors are involved in the development of the disease. These are, for example, genetic, metabolic, biochemical, biomechanical factors. As a result, there is an inflammatory process and a whole cascade of involvement of the joint and surrounding structures.
What is cartilage?
Cartilage is connective tissue, strong but flexible. It is composed of cells, that is, chondrocytes. Chondrocytes subsequently produce components of the intercellular mass. It is covered with perichondria, which is a thin fibrous sheath.
The perichondrium is supplied with blood vessels that supply nutrients. Otherwise, the cartilage itself does not contain blood vessels.
The internal structure of the cartilage is arranged in chondromas. Chondrone is made up of chondrocytes and around having intercellular fluid and tiny fibers that add strength.
Cartilage is either cellular, hyaline, elastic, or ligamentous. The hyaline type is represented in the joint. It serves as a shock absorber, which ensures its strength and flexibility. The surface of the cartilage is slippery, which has a positive effect on friction.
Osteoarthritis = cartilage damage
Osteoarthritis is characterized by cartilage damage, by decreasing its quality and narrowing it. Degradation in the form of erosion extends from the surface to deeper structures.
This disruption process results in the initiation of new formation processes as well as remodeling (shape change) of the peripheral part of the bone.
Subsequently, the joint surfaces and bone in the area under the cartilage are also affected. In addition, the damage also affects the ligaments, the overall joint capsule, and the surrounding muscles. Ultimately, these changes lead to joint damage.
Osteoarthritis damage affects:
- articular cartilage
- it is defibrated
- its diameter narrows
- na jej povrchu vznikajú trhliny
- bone
- formation of osteophytes, ie growths
- in the area under the cartilage, the subchondral part, subchondral sclerosis occurs
- articular capsule
- muscules
- ligaments
- the joint space narrows
- increased production of joint fluid (synovial fluid)
Osteoarthritis is divided into primary and secondary ones. In the case of primary osteoarthritis, the reason for the damage is not fully understood.
The secondary type has a known reason, it can be caused by internal factors but also by external ones. The onset of secondary osteoarthritis is therefore conditioned by another disease or injury or congenital malformations. Diseases that cause osteoarthritis include, for example, DNA, diabetes, and even arthritis.
TIP: Information on inflammatory joint damage in an article on arthritis.
The cartilage in the joint is not supplied with blood, but only from the surrounding fluid. This also affects its regeneration, which does not occur. That means that once the cartilage is damaged, it will no longer heal. When cartilage is damaged and lost, the bones on each other wear out.
The damage is subsequently the result of impaired joint function, ie restrictions on movement and pain. Osteoarthritis can affect the joint of a 30-year-old person, and it mainly damages the small joints and joints that are responsible for carrying bodyweight.
When designating a disability of a given joint, it is widely known as:
- coxarthrosis, which is a disorder of the hip joint
- gonarthrosis when osteoarthritis affects the knee
- nodal osteoarthritis - affects the small joints of the fingers
- spondylarthrosis in damage to the intervertebral joints, ie the spine
Osteoarthritis does not affect all joints at once.
It can affect only one joint. Some get small joints in their arms and legs, others, large joints, such as the knee or hip. In men, it is affected mostly in the knee whereas in women especially the hip joint. Eventually, it develops gradually over several joints.
According to the number of affected joints, it is also divided into:
- generalized - particular form, when it affects at least 3 joints or joint groups
- oligoarticular - in less than three
- monoarticular, localized if only one joint is affected.
Causes
Primary osteoarthritis has no fully elucidated cause.
The secondary is caused by a known cause.
It can be based on another disease, metabolic, endocrine, hormonal disorder, inflammation as well as injury. It can also be a result of incorrect anatomical position. As in the case of hypermobility of the joint, or even different lengths of the bones of the lower limbs, which causes problems especially when walking.

Among risk factors that affect the development of osteoarthritis belongs:
- old age
- genetic factors
- heredity
- gender, coxarthrosis mostly in women, gonarthrosis in men
- congenital malformations
- inflammatory diseases of the joints
- rheumatoid arthritis
- aseptic arthritis
- metabolic causes
- diabetes
- DNA
- endocrine diseases
- obesity
- hypertension
- hormonal factors
- in women also the number of pregnancies
- smoking
- injury
- anatomical position, the axial position of joints, hypermobility, shortening of one limb
- bad movement habit, biomechanical causes
- lack of exercise
- excessive workload, whether work or physical activity, sports
- muscle strength
A degenerative case, the result of which there is the gradual erosion of cartilage, disruption of the surface, and cracks in the structure. This results in impaired function of the cartilage as a damper and joint bearing.
This is associated with the formation of bone protrusions, increased formation of intra-articular fluid, and thus increased pressure inside the joint. Bone damage under the articular cartilage, disruption of the surrounding soft tissues, such as ligaments or muscles, results in joint dysfunction, pain, and other difficulties.
From the etiology (origin) point it is divided into::
- primary
- secondary
- metabolic diseases
- ochronosis, acromegaly, hemochromatosis
- Joints anatomical changes
- joint dysplasia, hypermobile syndrome, unequal limb length
- injuries - joint damage due to fractures and other traumas
- inflammatory arthropathy
- septic arthritis, rheumatic diseases
- metabolic diseases
Symptoms
In addition to these two main symptoms, there are other, associated difficulties. The movement disorder itself has its typical course. Joint hardening during inactivity is a common characteristic. This is the case especially in the morning, the stiffness of the joint can take 15-30 minutes to move.
Restriction of joint mobility is more serious.
Of course, it depends on the degree of degradation and the joint damage. Similarly, pain depends to such an extent. It can initially be effortless, as it starts, same as in the morning and after inactivity. Tender pain indicates severe joint damage.
At a later stage, various noises may be heard as you move. They come from the joint for increased friction of overlapping bones. The manifestation is a creaking or squeaking, reminiscent of sand in a joint.
New bone formation results in various bone protrusions and growths. They are technically referred to as osteophytes. These growths are long-term. They cause deterioration of the function of the affected joint, pain or numbness, and deformity of the joint.

Among symptoms of osteoarthritis belong:
- limitation of joint function, this can manifest as curvature
- joint stiffness after inactivity, especially in the morning after waking up
- restriction of movement to loss of joint mobility
- pain
- starting pain after inactivity
- exertional pain
- passive movement pain
- in late-stage also pain at rest, nocturnal pain
- the pain can also worsen due to the position of the limb, the weather
- torment
- crackling, creaking, as if there is sand in the joint
- joint deformation
- swelling in the joint area
- the local increase in skin temperature
- reddening of the skin at the joint
- at a late stage, the muscle is also affected, which secondarily contributes to the pain
- muscle weakness, muscle atrophy
- it's shortening
- shortening of the limb, followed by muscle damage
- joint instability
Diagnostics
A doctor, usually an orthopedist, evaluates during a clinical examination:
- functional condition of the joint
- range of motion
- stiffness
- soreness
- deformity
- swelling, temperature, and skin color
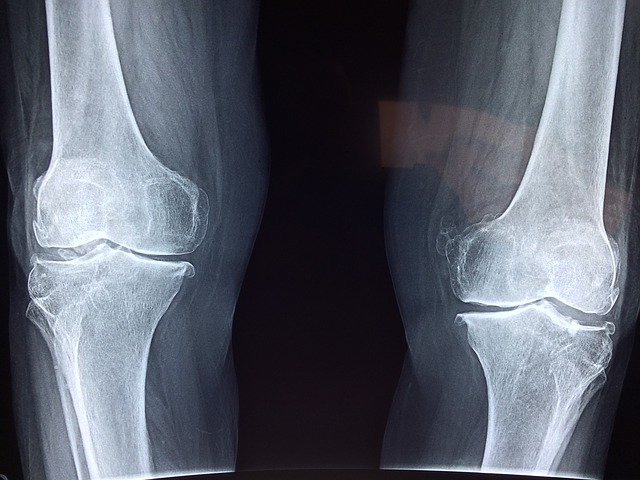
It is important the exclusion of rheumatoid arthritis and other diseases. Laboratory blood tests (rheumatic disease, psoriasis, DNA) may be chosen to rule out another diagnosis. Subsequently, imaging methods such as X-ray, USG, scintigraphy, CT, or MRI are important. The extent of osteoarthritis is divided into four stages after evaluation of the X-ray findings.
The table shows 4 stages according to the X-ray finding
| Stage | Description |
| 1. stage |
|
| 2. stage |
|
| 3. stage |
|
| 4. stage |
|
Arthroscopy may be indicated for another cause and a secondary finding may be found next to it, that damages the cartilage. As with any disease, early diagnosis is important for osteoarthritis. After early diagnosis, treatment is initiated to reduce the manifestations and complications of the disease.
Course
The first symptom is starting joint pain. The pain subsides after the movement, it even subsides completely. Exercise pain occurs later. The late stage is marked by pain at rest, especially nocturnal pain.
Pain is aggravated by exertion, inappropriate position of the limb. It can be significantly affected by the weather. Joint stiffness after inactivity is associated, especially in the morning. It usually lasts 10-15 minutes, even half an hour.
At a later stage, the shape of the joint changes, various deformations, and the position of the bones are present. The range of motion is reduced and the result is a reduction or even loss of the ability to move. In the last stage, squeaking and squeaking are audible. The people in question also describe it as if they were feeling sand in their joints.
Swelling, redness, and fever occur locally. The disease also affects muscle and other soft tissues. This results in instability in the joint. Muscles weaken, limbs can be shortened.
How it is treated: Arthritis
How is arthrosis treated? Can it be stopped? Medications and lifestyle modification
Show moreArthroses or Arthritis?
Arthritis is treated by
Other names
Interesting resources










