- pubmed.ncbi.nlm.nih.gov - The diagnosis and management of shoulder pain. Gina M Allen
Shoulder Pain: Symptoms, Treatment

Shoulder joint pain is a common musculoskeletal problem that can complicate even the most mundane daily activities. What is behind the development of shoulder pain?
The shoulder joint is one of the most complex joints of the human body, in the vicinity of which a large number of muscles are located. Its pain can be caused by overload, injury, instability, injury, disease and many other factors.
What are the possible causes of shoulder pain, how the diagnosis proceeds and much more you will learn by continuing in the article.
Anatomy of the shoulder joint at a glance
To understand the primary issue of shoulder pain, it is helpful to know at least the anatomical basics.
The shoulder joint is composed of three bones: the humerus, the scapula and the clavicle. The humerus has a spherical shape at its end - the capitulum, which fits into the recess of the prominence on the scapula.
The posterior ridge called the spina scapulae, the anterior coracoid process, and the suprascapular acromion process arise from the scapula and are significant in the development of shoulder disorders.
Around the shoulder joint are a number of ligaments that ensure the stability of the area.
The sinuous soft structures found between the individual structures, the bursae (small fluid-filled sacs), aid in the natural gliding and movement between the different components of the shoulder.
The shoulder joint involves a large number of muscles from the cervical-thoracic spine, the chest and the upper limb itself (biceps, triceps...)
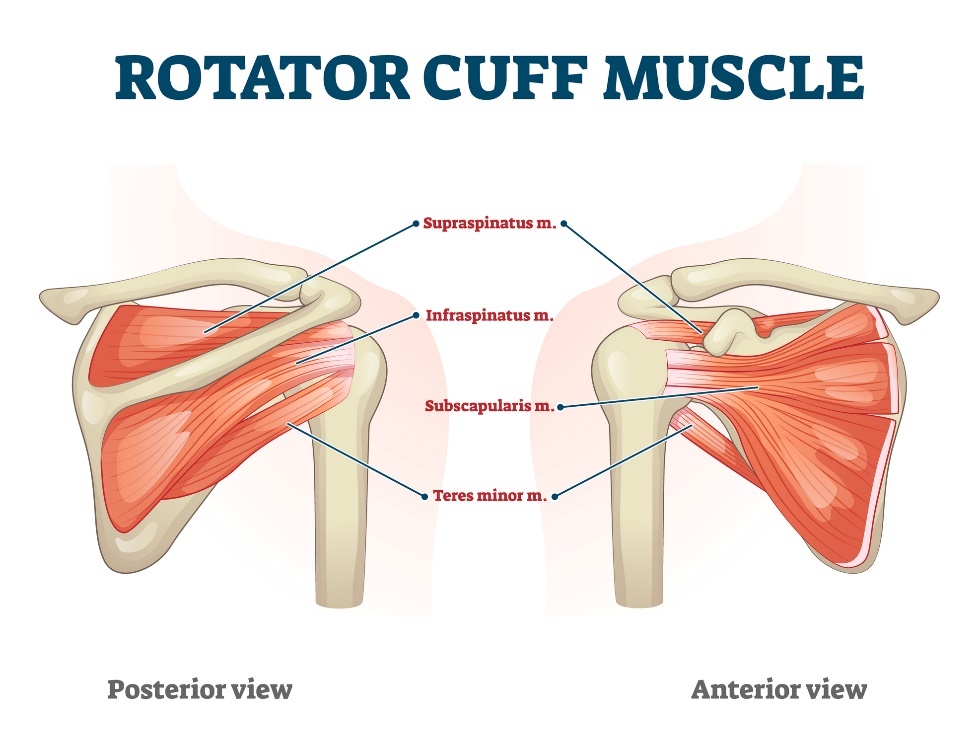
The muscles of the shoulder are mainly made up of a group of muscles called the rotator cuff. It is formed by the musculus supraspinatus. mus. infraspinatus, mus. subscapularis and musculus terres minor.
Anatomically, they cover the largest part of the shoulder joint and play a significant role in most shoulder movements.
Etiology of the onset of shoulder pain
Due to the anatomical complexity of the shoulder joint and the multitude of muscle groups involved in shoulder function, the aetiology of pain is varied and multifactorial.
Shoulder disorders can be divided into functional disorders and structural (organic). In the case of functional, it is mainly a disorder of stability and function due to changes in soft structures (muscles, fascia, ligaments...).
Structural disorders are in turn caused by some organic pathological finding in the sense of a degenerative process of arthrosis, a fracture or a nervous disorder.
Functional impairment may progress to structural impairment.
Functional disorders of the shoulder
Since the functional disorders are related to soft structures, their number is really extensive. The most common disorders and diagnoses related to the shoulder are listed below.
Muscle imbalance
Muscle imbalance means an imbalance in the state of the muscles. One muscle group is weakened, while the other nearby muscle group is in turn overloaded and possibly shortened with the occurrence of spasms (stiff muscle fibres).
Weakening of the interosseous muscles together with overloaded shortened upper trapezius fibers and shortened pectoral musculature cause a muscular imbalance in the brachial plexus called upper crossed syndrome.
Muscle imbalances creating a forward posture of the head and shoulders negatively affect the dynamics of the cervical spine, the shoulder joint and the position of the scapula itself.
Muscle shortening
Muscle shortening is a condition in which the elastic component of the muscle, called the ligaments, shortens for a variety of reasons.
However, the most common cause is frequent overloading of the muscle with exercise without sufficient compensation, whereby it reflexively shortens.
After shortening, the muscle does not allow the joint its full physiological range of motion. Shortening of a muscle or muscle group can cause muscle imbalance, excessive stretching, instability and pain.
Hypermobility and hypomobility
Increased range of motion above the physiological rate in both active and passive movement is referred to as hypermobility.
With local hypomobility of a particular segment, a compensatory mechanism often occurs to compensate for the lack of movement in another segment by hypermobility. Too much ligament laxity can cause a reduction in the stability of the area.
Restriction of the range of motion (hypomobility) in the joint occurs most often on the basis of four causes: structural disorders in the joint, retraction of the joint capsule (long-term immobilization, capsulitis, etc.), pathological changes in the muscles (weakening, muscle shortening) or functional disorders of the joint (joint blockages).
Scapula alata - winged scapula
The inner edge of the bone of the scapula is laid parallel to the course of the spine. The mus. serratus anterior muscle works in clamping the shoulder and fixes the scapula to the posterior thorax. When it is weakened or dysfunctional, the medial edge of the scapula deviates from the posterior chest wall.
This condition is known in Latin as scapula alata, or winged scapula. There is a change in the stability and mobility of the scapula that affects the shoulder joint.
Frozen shoulder syndrome
Frozen shoulder syndrome, professionally called adhesive capsulitis, is a shoulder joint disorder characterized by stiffness and restricted movement. It typically develops gradually during conditions where shoulder movement is restricted for prolonged periods of time.
The cause may also be spasm of the mus.subscapularis muscle, which restricts the movement of the shoulder and arm. As a consequence of stiffening and thickening of the joint capsule, there is a restriction of mobility in the joint in question.
In the vicinity of tendons and tendon attachments, calcium salts gradually migrate and deposits may form.
Structural disorders of the shoulder
The aetiology of structural organic diseases of the shoulder joint includes mainly mechanical damage (fractures, luxations), inflammatory processes, nervous disorders and degenerative diseases (arthrosis).
Arthrosis of the shoulder joint
Progressive degenerative changes in the cartilage of the bones of the shoulder joint can also be the cause of shoulder pain and reduced mobility.
The most common is arthrosis (osteoarthritis), whereby there is a narrowing and weakening of cartilage tissue with the eventual formation of osteophytes (bone deformities). The disease is associated with older age and wear and tear of the joints.
The manifestation of arthrosis is mainly pain in the joint and a feeling of stiffness.
Luxation, subluxation and fracture
A fracture or dislocation causes instability and pain in the shoulder joint. The most common cause of fracture and dislocation is a fall and severe impact. Common fractures are fractures of the clavicle and humerus.
Shoulder dislocation, luxation, is a condition where the head of the humerus leaves the joint socket and remains in the wrong position. If the head is partially displaced out of the socket and then returned to the joint, it is a subluxation (partial dislocation).
Fracture and dislocation of the shoulder can injure the soft tissues near the shoulder joint, causing associated complications.
Impingement syndrome
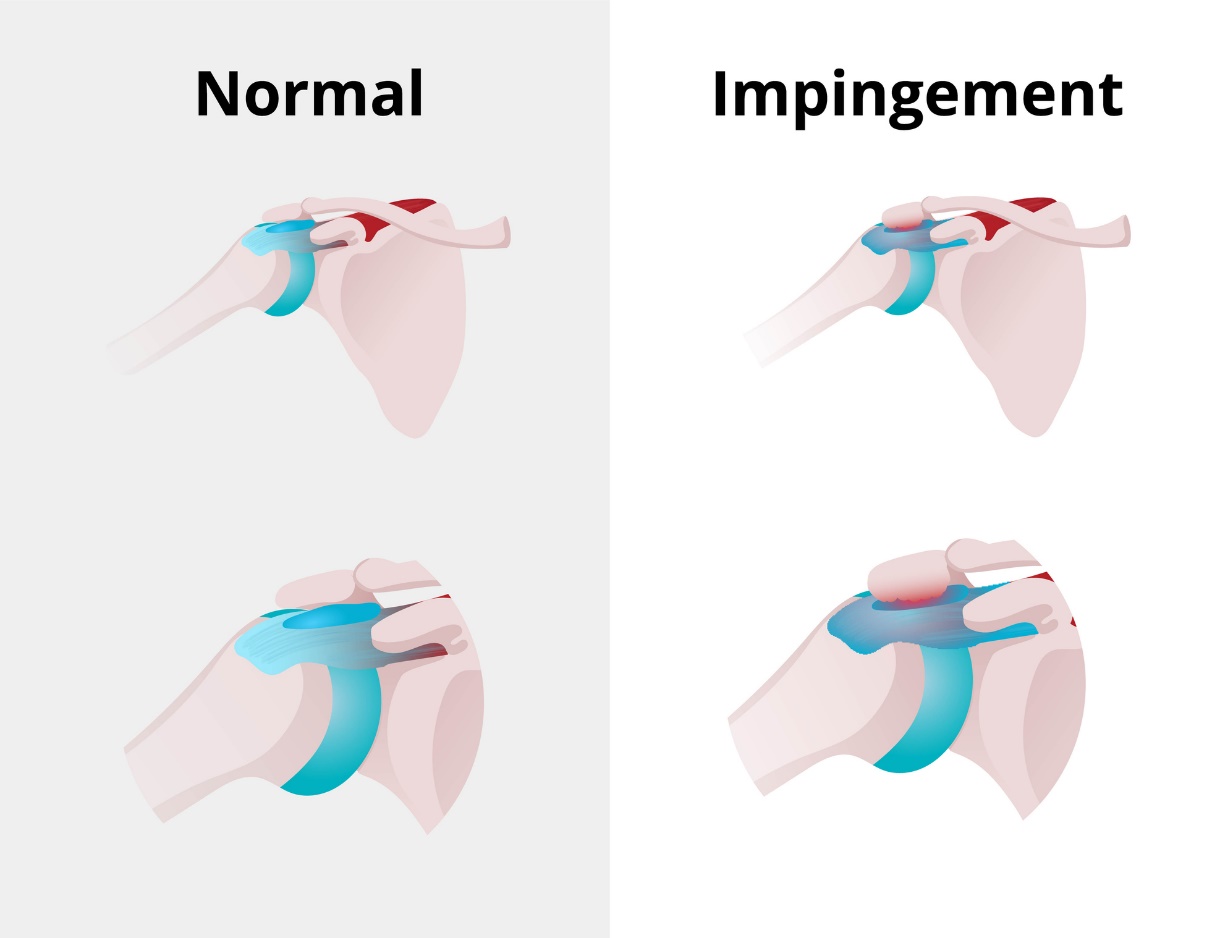
Impingement syndrome is a painful condition of the shoulder joint caused by irritation and inflammatory reaction of the synovial sac (bursa) below the scapular prominence of the acromion.
If there is a gradual narrowing of the space between the bone acromion and the head of the humerus, pain arises. Impingement syndrome is commonly referred to as swimmer's shoulder and thrower's shoulder.
Pain occurs both when moving and at rest. Nocturnal pain and inability to sleep on the affected tent is a frequent concomitant of impingement syndrome.
Functional disorders leading to strait syndrome are muscle imbalance, shoulder protraction, biceps head spasm, and impaired muscle coordination.
Among the causes of anatomical nature are mainly hook-shaped protrusion of the acromion and degenerative changes on the rotator cuff.
Tendinitis
Inflammation of the tendons (ligamentous attachments) of the muscles is professionally called tendonitis.
Within the shoulder joint, calcium salts are deposited in the rotator cuff area, where chronic compression prevents blood flow and blood supply to the area.
The clinical picture resembles impigement syndrome. There is restriction of active movement and pain in the shoulder joint.
Bursitis
A relatively common cause of pain in the shoulder joint is inflammation of the synovial sebaceous sac (bursa). When overloading the muscles and tendons due to repetition of movements and overload, an inflammatory process of the synovial bursae can occur. Impact is also a possible cause.
Bursitis is manifested mainly by swelling, an increase in local temperature, joint stiffness and pain on movement.
Damage to the rotator cuff muscles
The most common cause of shoulder pain is inflammation or tears in the rotator cuff muscles of the shoulder joint. The tear and damage to the muscle fibers is manifested by pain, limited mobility to loss of muscle strength.
The cause of its occurrence is closely related to impingement syndrome, degeneration of the tendon tendon, frequent overloading of the musculature, resulting in chronic rupture. Acute rupture of the muscle occurs mainly with injuries and mechanical damage.
Damage to the head of the biceps
Tendinosis, or inflammation of the tendon of the long head of the biceps, exhibits tenderness on flexion at the shoulder and flexion at the elbow. On ultrasound, swelling and synovitis of the tendon tendon of the biceps tendon is visible.
The disability arises most often with excessive overloading (sports, work), when the position of the upper limb is in the forearm shoulder joint and simultaneous flexion at the elbow joint.
Rupture of the biceps occurs mainly when lifting heavy loads, causing damage and tearing of the tendon attachments from the shoulder joint. The muscle is often chronically overloaded and degenerated prior to the injury.
The biceps muscle can become damaged both at the site of the attachment and in the medial part of the fibers. There is a weakening of muscle strength, pain and swelling of the affected area.
Nerve disorder - nerve compression
With age, degenerative process or injury, the vertebrae and intervertebral discs in the cervical segment can become disrupted. The consequence of which can be compression on the cervical nerves directed to the shoulder and the entire upper limb.
With nerve oppression, a person feels muscle weakness, numbness or tingling in the shoulder and limb, and shooting pain into the arm.
Diagnosis of shoulder joint disorder
Diagnosis of the shoulder joint consists mainly in a comprehensive examination by an orthopaedic surgeon, physiologist or neurologist. The physician's goal is to find the cause of the pain and rule out/confirm a structural problem.
The doctor will examine the shoulder joint by sight, palpation and test the stability and mobility of the shoulder joint in all directions.
The examining physician tests the range of motion of the joint in both passive and active motion and uses resistance testing to determine any painfulness in the execution of the movement.
In most cases, the patient is indicated for an imaging examination, which serves to show the internal structures of the affected area in detail.
Ultrasound is mainly used for more complex disorders of soft structures. X-ray examination is mainly used to examine and image the condition of bone tissue.
Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) are used to image the soft structures of the body - muscles, nerves, ligaments.
Another possible diagnostic procedure is EMG, or electromyograph), which is used to examine the musculature, peripheral nerves and assess neuromuscular coordination.
Infrared thermography captures radiation from the surface of an organism in the form of an image. It helps to more accurately determine the type of pain information and the localization of the inflammatory process.
Arthroscopy is a surgical and diagnostic procedure in which a thin optical instrument (arthroscope) is inserted into the joint. This allows the doctor to view the internal structures of the shoulder on a monitor in detailed resolution.
Treatment options for the shoulder joint
The exact type of pain treatment depends entirely on the determined cause.
Treatment of the shoulder joint can be conservative treatment in the form of physiotherapy, rehabilitation and ergonomics of movement.
Pharmacological treatment consists mainly in the application of analgesics, chondroprotectants and anti-inflammatory drugs.
Surgical treatment is also an option, which is indicated especially for injuries, structural damage and ineffectiveness of conservative or pharmacological treatment.
Conservative treatment
The primary component is rehabilitation in the form of exercise with a physiotherapist, ergonomics of everyday movement and the application of physical methods.
Within the physical methods of the shoulder joint, ultrasound, electrotherapy, laser, shock wave, hydrotherapy or thermotherapy can be applied. The choice depends on the specific disorder and the goal of treatment (pain, inflammation, healing...).
Within the framework of domestic physical methods, the application of hot or cold compresses is common. Warm compresses are used in the treatment of chronic conditions. They have a myorelaxing effect - they relax the muscles, relieve stiffness and reflex pain.
Conversely, ice packs are used to reduce swelling and pain in the context of acute inflammation and congestion, or as a prevention against the onset of inflammation. However, consultation with a physician is advisable.
Physiotherapy aims to eliminate muscle imbalances, strengthen weakened and relieve overloaded shortened muscles, improve stability and mobility of the shoulder and modify the functional disorder itself.
The rehab professional uses various therapeutic methods, e.g. kinesiotaping, also called elastic therapeutic tape, kinesiology tape, kinesiology therapeutic tape, Kinesio tape, or k-tape for the damaged area with a therapeutic functional tape in order to stabilise or relax the soft structures of the segment - is often used in the shoulder.

Pharmacological treatment
For pain in the shoulder, medications are usually taken to relieve pain, swelling and inflammation. These may be total oral medications or topical creams for inflammation of tendons, muscles and joints.
Local application of anti-inflammatory drugs (for example, corticosteroids) in the form of an injection is possible.
In degenerative diseases, the injection of chondroprotective agents (substances that support and nourish cartilage) directly into the joint is also an option. In painful conditions, treatment with local anaesthetics in combination with an anti-inflammatory agent may be prescribed.
In addition to classical medical treatment, patients with degenerative joint disease can try a method using local application of stem cells. Stem cells are part of the body's own body and have regenerative and healing effects for the joint.
Surgical treatment
The surgical intervention chosen is based on the cause of the pain and dysfunction of the joint.
This can include shoulder stabilization, suturing muscle and ligament tears, releasing calcified components, decompression, replacement with an artificial joint (endoprosthesis), release of nerve structures, and many others.
Surgical treatment is indicated especially in case of injuries and fractures, high degrees of osteoarthritis, ruptures of soft structures or failure to improve the state of health by conservative and pharmacological treatment.
Recovery is individual to the specific type of procedure.
Prevention of shoulder joint pain
Prevention to healthy function of the shoulder joint consists mainly in regular appropriate movement with correct technique, regeneration and seeking professional help at the first signs of disorder or disease.
If you do not know the right exercises to choose, it is advisable to contact a physiotherapist, physiotherapist or certified trainer who will recommend the appropriate exercises for your health and physical condition.
Prevention of shoulder joint pain:
- Regular and compensatory physical activity.
- Stretching of shortened muscles.
- Correct posture and head posture.
- Sufficient regeneration.
- Sufficient intake of vitamins and minerals.
- Quality regular sleep.
- Not delaying the doctor in case of pain.
Interesting resources










