- Waiting for a baby: 2nd, updated edition - Gregora Martin, Velemínský Jr. Miloš
- digilib.k.utb.cz
- uesa.sav.sk
- portal.jfmed.uniba.sk
- Mayoclinic.org - Placenta: How it works, whats normal
- pregnancybirthbaby.org.au - What is the placenta?
- Theplacenta: What is it and how it works
What is the placenta, when is it formed and what is its function during pregnancy?

The placenta (amniotic sac) has a great influence on the course of the whole pregnancy. During pregnancy, it nourishes your baby so that it can grow nicely. It protects it, breathes for it and replaces all the organs that develop during intrauterine development. It is the link between mother and baby.
Article content
- When and how is the placenta formed?
- What is the purpose of the placenta?
- What does the placenta look like and what is its shape?
- Does the placenta change size during pregnancy?
- What is the function of the placenta?
- What is the importance of the placenta to the fetus and pregnancy?
- How is the placenta examined?
- The placenta in the 2nd and 3rd stage of labour
- What can be the irregularities of the placenta?
- Irregular placement of the placenta
- Placental irregularities
- Premature placental abruption
- Placenta after childbirth and its use
- Culture and rituals after placenta delivery
When and how is the placenta formed and what is its purpose?
What does it look like, what shape does it take and how does it change size during pregnancy?
What is its function and its importance to the fetus and pregnancy and in the 2nd and 3rd stage of labour?
What can be its irregularities?
The placenta after birth, its uses and cultural customs and rituals after birth.
When and how is the placenta formed?
The cells of the embryo divide into an embryoblast and a trophoblast before the embryo has nested, around day 4. The trophoblast develops into the placenta, umbilical cord and amniotic sac. By day 7, the trophoblast is fully adherent to the uterine wall and begins to produce hCG (human chorionic gonadotropin).
Read also.
After nesting, it attaches to the mother and thus blood exchange takes place between her and the fetus. Gradually, it inserts more into the uterine lining and nourishes the fetus. From the 12th week of pregnancy, it is already fully functional.
The placenta develops in advance in the first weeks to prepare everything needed for the rapidly developing fetus.
What is the purpose of the placenta?
It forms a kind of barrier, which protects the fetus from harmful influences and the penetration of harmful substances. However, not all harmful substances can stop it and some penetrate the fetus.
Therefore, the mother-to-be should beware of drugs, alcohol, caffeine, cigarettes and other harmful substances. Nicotine is very harmful and can cause growth disorders in the fetus. Mothers who smoke often give birth to small babies with low birth weight.
There is a space between the maternal and fetal parts of the placenta where maternal blood with oxygen and nutrients is brought in and washes the chorionic villi. In this way, nutrients and gases are exchanged. There is a mixed blood flow in the fetal blood vessels. It is not divided into oxygenated and deoxygenated blood as in a born human.
Maternal and fetal blood never mix.
The placenta is an organ formed only during pregnancy. It connects the fetus to the mother's body by attaching itself to the uterine wall. Through it, nutrients pass from the mother's blood to the fetus' blood, removing waste substances and allowing gas exchange.
What does the placenta look like and what is its shape?
It is made up of chorionic villi.
There are two sides to the placenta.
The inner (amniotic) side of the placenta is shiny, covered with amniotic membranes. The umbilical cord protrudes from the inner side.
The other side (maternal) is attached to the wall of the uterus.
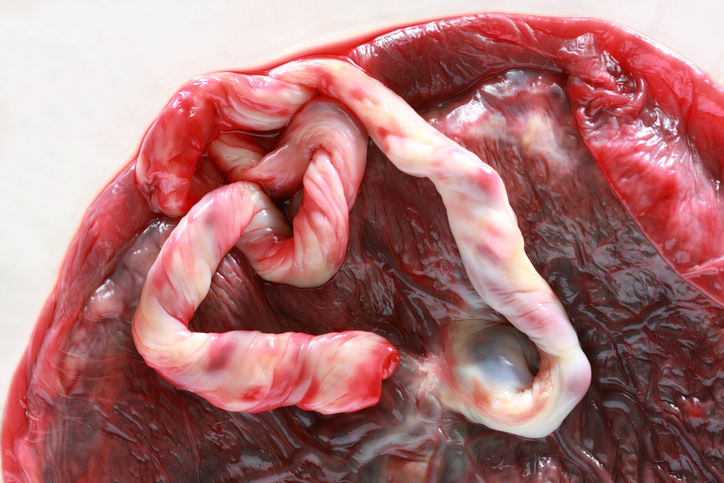
It is flat and round in shape, in the form of a disc, although the size and shape varies for each. It is usually attached in the upper, lateral, anterior or posterior part of the uterus. In rare cases, it is deposited in the lower part of the uterus.
It has an approximate diameter of 22 cm and a thickness of 2-2.5 cm.
It weighs approximately 500-600 g.
The colour of the placenta is dark reddish blue or has a purplish colour. It is connected to the fetus by an umbilical cord, which usually measures 55-60 cm. It is composed of arteries and veins through which blood exchange between the mother and the fetus takes place. The artery carries deoxygenated blood, waste substances from the fetal body to the placenta. The umbilical vein supplies the fetus with oxygenated blood and nutrients.
The placenta is thickest at the junction with the umbilical cord, most often in the middle.
Does the placenta change size during pregnancy?
The placenta grows along with the fetus and occupies approximately 15-30% of the surface of the uterus. During pregnancy, it increases in size until 26-38 weeks and changes in thickness. It thickens until about 8 months of pregnancy and begins to thin out before delivery.
You can read more about pregnancy and fetal development in the article.
What is the function of the placenta?
- Protective - protects the fetus from pollutants, chemicals, drugs and infections
- Nourishing - ensures the exchange of gases and nutrients between mother and fetus
- Secretory - by producing hormones
What is the importance of the placenta to the fetus and pregnancy?
It is important not only in the transport function between the mother and the fetus, where gases and nutrients are exchanged, but also in a number of other functions. It ensures proper fetal development and the progress of a normal pregnancy.
It also has an endocrine function aimed at hormone production, immunological, protective and thermoregulatory functions.
The table lists the female hormones and hormones produced by the placenta
| hCG |
|
| Lactogen |
|
| Estrogen |
|
| Progesterone |
|
Adjustment of the mother's immune system is very important during pregnancy so that the mother's body can tolerate the pregnancy and the fetus can develop.
The placenta and the fetus must be accepted, tolerated and treated as sufficiently their own. However, they must still be treated as distinct to some extent to ensure protection against attack on the fetus by the mother's immune system.
How is the placenta examined?
Examination is done by ultrasound. Its fit, shape and function are observed. The blood supply to the placenta between the fetuses is very important. It is monitored on sonographic examination where disturbances in blood flow can be detected. When blood flow decreases, the fetus tries to equalize the blood supply to other parts of the placenta.
The placenta in the 2nd and 3rd stage of labour
During a normal pregnancy, it is deposited in the front, sides or back of the uterus.
In the second stage of labour, it has a large role as it has to oxygenate the baby during contractions and expulsion of the fetus from the uterus.
In the third period of labour, the placenta is delivered, expelled from the uterus. Normally, it may take several tens of minutes. The uterus shrinks after the birth of the newborn. Contractions are still taking place, but they are no longer painful. This is followed by the gradual detachment of the placenta from the uterine wall and after the last push of the mother, it comes out of the uterus together with the amniotic sacs.
This is also known as placenta delivery. It is not painful and many women do not even feel its expulsion.
After delivery of the placenta, the obstetrician will examine it thoroughly. He will make sure that there are no unbroken pieces left sticking to the uterine wall. If the obstetrician suspects that there is a piece left in the uterus, a cleaning, curettage under general anaesthesia is done.
During the fourth 2 hours of labour, the parturient is monitored for uterine bleeding and her general condition. She is then transferred to the antenatal ward.
Another interesting article.
What can be the irregularities of the placenta?
Irregularities in the development of the placenta can be related to size, shape, structure or function. It can have different shapes such as a heart, a horseshoe or consist of multiple lobes - placenta biloba (two lobes), triloba (three lobes), multilobed (multiple lobes).
In the case of completely separate parts of the placenta, two, three placentas, it is a bipartite placenta (two-part placenta), tripartite (three-part placenta).
The other placenta, which is smaller, is called the placenta succenturiata.
The two are connected by blood vessels.
A problem can arise at birth when the main placenta is expelled and the other part remains in the uterus.
Placental infarction - small pieces of dead tissue are seen on the placenta as pale spots, sometimes as red spots. Placental infarctions in small amounts in the last trimester are normal. They are common in gestosis, high blood pressure or diabetes. If they are in larger amounts, they can cause deterioration in its function. This results in a hypotrophic fetus or even fetal necrosis.
Therefore, checks in the gynaecological outpatient clinic and monitoring of fetal development and blood flow are very important.
Irregular placement of the placenta
Placenta praevia (incestuous fetal bed) is an abnormal location and nesting of the egg. It does not appear immediately in the first trimester, but as a complication in the 2nd-3rd trimester of pregnancy. In this case, the placenta is located above the cervix, in the immediate vicinity of the cervix or in the lower part of the uterus.
It is one of the most serious bleeding in the 2nd-3rd trimester. There is an increased risk of fetal and maternal death due to bleeding. It is more common in women over 30 years of age.
Placenta praevia is divided into 4 grades as shown in the table
| 1. | Central placenta praevia |
|
| 2. | Partial placenta praevia |
|
| 3. | Marginal placenta praevia |
|
| 4. | Low-set placenta |
|
Placenta praevia occurs in 5 out of 1000 births. Babies born with this placenta placement are more likely to be born with a lower birth weight.
The manifestation is vaginal bleeding, which occurs suddenly, without symptoms, in the second to third trimester, most often in the 27th to 32nd week of pregnancy. The blood tends to be bright red. The onset of bleeding is not significant and does not threaten the life of the mother or the fetus. It usually stops spontaneously.
Severe bleeding occurs with repeated bleeding.
Therefore, it is always necessary to inform the gynaecologist if bleeding from the genitals is observed. Expectant mothers must be closely monitored and supervised by medical care.
Examination for placenta praevia bleeding is never done vaginally or rectally.
Examination is done in the operating theatre, where immediate caesarean section procedure is provided.
Nowadays, when placenta praevia is confirmed and complications have already begun, hospitalization of the pregnant woman is recommended. This is for better control and to avoid complications. Treatment consists of medication, bed rest and waiting until the fetus is viable. Hospitalization is important for immediate intervention and to eliminate the risks associated with death.
Women at home with a diagnosis of placenta praevia should avoid sexual intercourse.
Placental irregularities
The placenta adherens is a more firmly attached placenta to the uterus. It is more difficult to detach during labour. Sometimes manual lysis (removal by hand) is necessary.
Placenta accreta (conjoined placenta) means a deep ingrowth into the uterus, from a lighter ingrowth to a general ingrowth into the uterine musculature to the surrounding organs. It does not present any difficulties during pregnancy.
However, if the placenta is accreta, women are at risk of bleeding during its removal. It is more difficult to detach, which may take more than 30 minutes. In cases of mildly ingrown placenta, manual detachment, manual lysis of the placenta from the uterine wall, is performed. In cases of severe ingrown placenta, surgery is performed to stop the bleeding. If it is completely ingrown, a hysterectomy (removal of the uterus) is necessary.
During pregnancy, placenta accreta is more difficult to diagnose. If it is already confirmed to be overgrown, a caesarean section is planned.
Premature placental abruption
Ablatio, abruptio placentae praecox, is the premature detachment of the placenta before birth. It occurs in 1% of births. It can be caused by gestosis with heart and kidney disease, high blood pressure or trauma in the abdomen. During labour, it can be triggered by a too-short umbilical cord and, with subsequent traction, begins to detach.
The separation may be partial or even complete. In mild separation and subsequent bleeding, there may be no symptoms in either the mother or the fetus. In severe forms, most often after trauma, there are signs of shock such as pallor, thread-like pulse or low blood pressure. The uterus is painful and tense. Treatment is based on the size of the placental separation, and is treated with medication, bed rest, ice on the abdomen, which stops the bleeding. In more severe forms, a caesarean section is performed.
Insufficiency of the placenta means that the placenta has a reduced function, insufficient activity and is not able to adequately supply the fetus. It occurs in late gestosis, fetal transfer, diabetes mellitus, in violation of its part. It is manifested by a change in the fetal heart sounds, increased fetal movements. On examination of the amniotic fluid, the water is greenish, turbid.
Placenta after childbirth and its use
Nowadays, the action of placental stem cells and their effect on the treatment of cancer, damaged organs and their wide use for their healing effect is still being studied. There are several ways to process the placenta. Nowadays, it is possible to make tablets that contain nutritious substances.
The aim is to relieve postpartum depression and improve milk production.
Some mothers even eat their placenta. They prepare dishes from it, use the dried placenta for example in soups as broth or make a placenta cocktail. Various tinctures or essences for mother and baby are also produced.
The cosmetics industry is also aware of its beneficial effects. It uses placenta for various skin preparations and creams for a more youthful appearance of the skin, which has incredible effects for its regenerative abilities. It is also used for the production of anti-hair loss products and lip balms.
Culture and rituals after placenta delivery
In different cultures, it has been treated according to rituals or superstitions.
In some folk cultures, the placenta was also considered a healing agent, especially for the first-born. It was rubbed on the birthmarks of newborns to make them pale, and women used it as a beautifying agent. It was also customary to bury it in the garden or bury it in the dunghill. Sometimes it was burned in a white cloth to protect it from anything bad.
The Maya thought of the placenta as the younger sibling of the newborn. Therefore, they wrapped it in banana leaves and went early in the morning to bury it in the jungle in a secret place known only to the man. He dug a pit in which to place it, covered it with ashes and placed corn kernels on top. Then he buried the pit with dirt. The Maya performed this ritual so that the god of death would not eat the child's soul and harm the parents.
Orthodox Jews did not have special rituals associated with the birth of a child. Their beliefs could not use parts of human tissue, so the placenta was not allowed to be used for anything. It was only used in the death of a newborn, when it was buried with the baby.
In Tibet, the placenta with the umbilical cord was an important part of the ritual. It was first examined by an astrologer to determine the appropriate day to bury it. It was wrapped in cloth and buried deep in the ground in a place designated by the father of the newborn so that animals would not dig it up. This ritual was an expression of respect for the entire family.
Interesting resources
Related










