- solen.cz - Basic principles of corticosteroid therapy in direct-immune neuromuscular diseases
- solen.sk - Systemic corticotherapy - specifics of glucocorticoid therapy
- solen.cz - Pitfalls of total and local corticosteroid therapy
- solen.sk - Corticoid-induced osteoporosis in children - pathogenesis and diagnostics
What are corticosteroids? When are they used and what are their side effects?
Do you know the side effects of corticosteroids? Which side effects do we need to be particularly careful of? Can children take corticosteroids?
Article content
The introduction of corticosteroids into clinical practice has been a major advance in medicine and has improved the quality of life and prognosis of many patients.
After the discovery of cortisol in 1948, there is even talk of a pre-cortisol and post-cortisol era.
For this unique scientific discovery, the Nobel Prize was awarded to T. Reichstein (for the discovery of cortisone), P. S. Hench and E. C. Kendall (for the introduction of glucocorticoids into practice).
Corticotherapy was first used in the treatment of rheumatoid arthritis.
Corticosteroid treatment brings relief to patients in many diseases.
Immunomodulatory agents, called immunomodulators, modify the immunological response of the body.
Corticosteroids have a wide range of uses in medicine.
They are often used primarily for their anti-inflammatory and immunosuppressive effect.
The list of all indications in which corticosteroids can be used in treatment is very extensive. They can act on various diseases of practically all organs of the organism.
Often the administration of corticosteroids is life-saving (e.g. allergic reactions).
The most common medical disciplines that use corticosteroids in treatment include gastroenterology, rheumatology, endocrinology, dermatovenerology, immunoallergy, pulmonology, etc.
When a patient receives treatment with corticosteroids, it has many benefits, improving the symptoms of the disease and relief.
Corticosteroids have their pitfalls when used for a long time. They can also have side effects.
Often there is no other option in the treatment of their underlying disease and patients are referred to long-term use of corticosteroids.
The effect of corticosteroids is exerted in the body by several mechanisms.
They represent an empirical, non-selective treatment. They act on the immune system as well as on other organs.
In long-term use, a certain balance must be sought between effective treatment and minimising side effects, which is very challenging.
What are their important effects?
The main beneficial effects of corticosteroids:
- Anti-inflammatory
- anti-allergic
- antiproliferative (prevents cell proliferation)
- reduction of permeability and stabilization of membranes
- analgesic (secondary)
Glucocorticoid production is regulated by the brain (hypothalamus-pituitary-pituitary axis) and the adrenal glands. Together they form the hypothalamus-pituitary-adrenal axis.
The highest levels of cortisol in humans occur in the morning and the lowest in the evening. Its level in the blood of a person is therefore subject to a daily rhythm. Its level is affected by stress, emotions, pain, illness, trauma, etc.
In common practice, we use synthetically prepared corticosteroids that suppress immunity at both the cellular and humoral (antibody) levels.
According to the duration of action glucocorticoids are distinguished:
- short biological half-life (up to 12 hours)
- medium-long biological half-life (12-36 hours)
- long biological half-life (over 36 h)
According to the duration of treatment we divide:
- short-term administration (up to 10 days)
- medium-term administration (10-30 days)
- long-term administration (over 30 days)
Corticosteroid dosage:
- one dose daily (in the morning)
- fractionated (2-4 times a day)
- alternate administration (2x daily dose at noon)
- administration in pulses of smaller (minipulses) or larger doses (pulse therapy)
Form of administration:
- Oral (by mouth)
- inhalation, intranasal
- intravenously (into a vein), so-called infusion
- topical (directly to the desired site)

Topical use is often encountered in dermatovenerology, where the corticosteroid is applied directly to the skin.
In orthopaedics, for example, direct injection into the joint (intra-articular) is used.
In neurology, it is often used for back pain in the form of 'sprays' which numb the nerves, reduce swelling and have an anti-inflammatory effect.
In pulmonary medicine, corticosteroids are used e.g. in inhaled sprays for asthma.

Topical use reduces the incidence of side effects compared to general use!
Selected corticosteroids that you may encounter most often:
Hydrocortisone, prednisone, prednisolone, methylprednisolone, dexamethasone, triamcinolone, betamethasone, fludrocortisone, etc.
What are the side effects with long-term treatment?
Side effects of long-term corticosteroid treatment:
- impaired glucose tolerance, diabetes mellitus (diabetes)
- disorder of lipid metabolism (fat metabolism)
- hypertension (high blood pressure)
- stomach ulcers
- acute pancreatitis (acute inflammation of the pancreas)
- muscle weakness (myopathy), fatigue
- osteoporosis (thinning of bones)
- psychological disorders (euphoria, depression)
- growth retardation (slowing of growth) in children
- increased susceptibility to infections
- glaucoma (high intraocular pressure)
- hypokalaemia (reduced potassium levels)
- increased/decreased white blood cells (leukocytosis, leukopenia)
- increased number of red blood cells (erythrocytes), called polyglobulie
- purple stretch marks on the skin, susceptibility to bruising
- increased risk of thromboembolic events
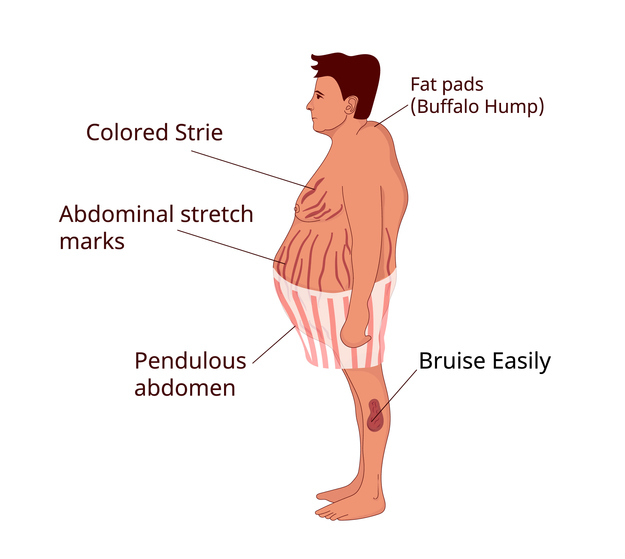
- iatrogenic Cushing's syndrome (crescent face, obesity - abdominal type, bull neck, purple striae, fatigue, depression, diabetes, hypertension, headaches, impaired wound healing, increased tendency to bruising, thinning of bones, etc.)
In the case of long-term corticosteroid treatment, it is recommended to introduce a so-called GK-treated patient card.
The patient's weight, blood pressure, incidence of peripheral oedema, cardiovascular status, lipidogram (lipid level), blood and urine glucose (sugar) concentration and intraocular pressure will be monitored and documented regularly.
Supplementation (repletion) of calcium and vitamin D is also recommended for long-term treatment.
Always consult a specialist!
Abrupt withdrawal of corticosteroids during long-term treatment will rapidly and significantly alter hormone levels. It may even endanger the patient's life.
Corticosteroid treatment in children
In the paediatric population, corticosteroid treatment is also used in several clinical fields. Its strong anti-inflammatory effect and immunosuppressive effect helps children in the treatment of a range of diseases, such as autoimmune diseases.
Clinical observational studies have repeatedly confirmed that it is essential to monitor bone metabolism in children during corticosteroid treatment. A detrimental effect on the growing skeleton and increased susceptibility to fractures have been described with long-term treatment.
Densitometric examination provides monitoring of the amount of bone mass. When monitoring a young patient, it is also important to check biochemical parameters and markers monitoring the turnover of bone metabolism.
In long-term treatment, patient management and careful dispensation by a specialist is essential. The aim is adequate follow-up, prevention of anticipated complications and minimization of risks.
Interesting resources










