- solen.sk - CERVICOGENIC VERTEBROGENIC SYNDROMS IN NEUROLOGICAL PRACTICE, Miloslav Dvořák, Andrea Hlubeková, Vlastimil Horný, Neurological Department of Spišská Nová Ves Hospital, Spišská Nová Ves, a.s., Spišská Nová Ves
- solen.sk - Lower back and pelvic pain in pregnancy, doc. Blanka Adamová, M.D., Ph.D. Department of Neurology, Faculty of Medicine, Masaryk University, Brno, CEITEC - Central European Institute of Technology, Masaryk University, Brno.
- parenting.firstcry.com - Neck pain in pregnancy - causes, remedies and prevention
- chirodenton.com - Neck pain: relief from neck and shoulder pain in pregnancy
- postpartumtrainer.com - Neck pain in pregnancy: [5 things you can do for relief].
Cervical spine pain in pregnancy? Why is it so common and how to learn to manage it?

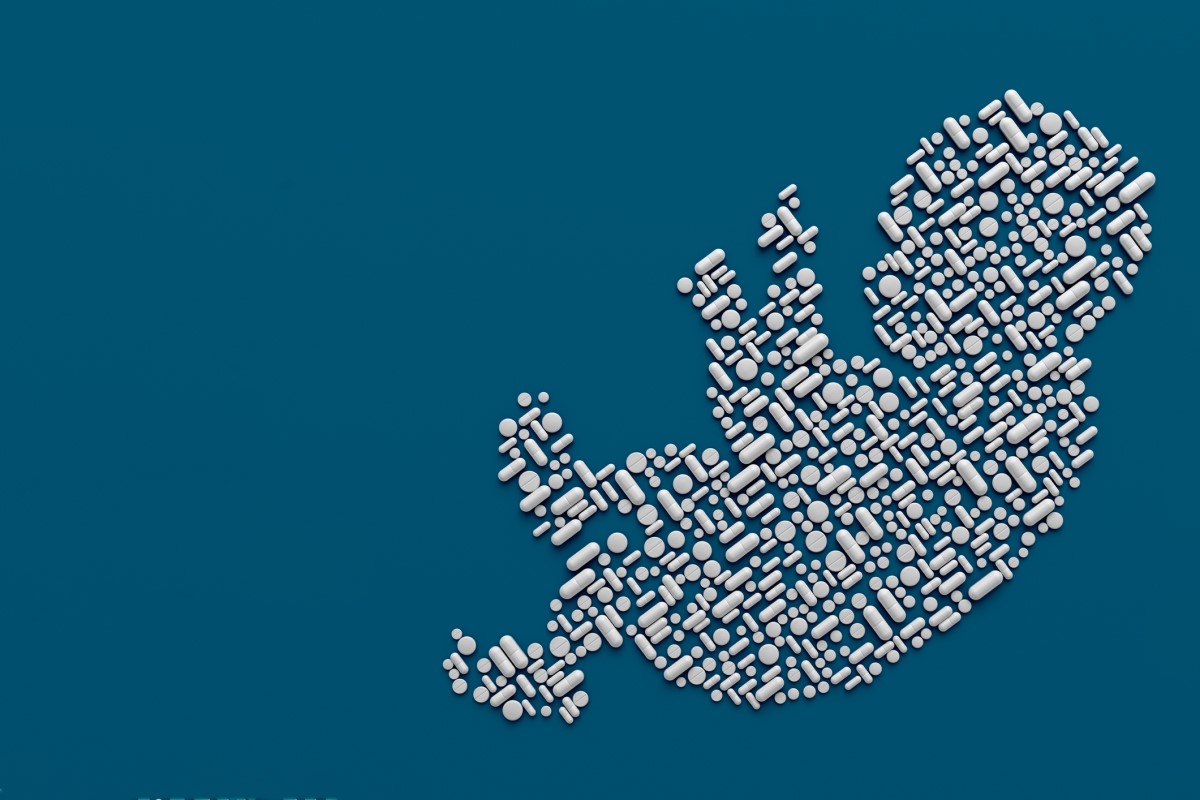
Pregnancy is a several-month process of major changes in a woman's body. Some changes bring unpleasant sensations and pain, but with proper preparation they can be at least partially avoided.
Article content
One of the most common problems that mothers-to-be experience before the joyful arrival of the baby is spinal pain. Most often it occurs in the cervical or sacral spine and pelvis.
The most common predisposing factors for the development of vertebrogenic pain are difficulties that arose before the pregnancy itself. These include obesity, high physical stress, congenital predispositions and poor posture.
When is the cervical spine involved?
If your pain is most often localized to the neck and back of the neck, is asymmetrical and unilateral, radiates to the scalp, behind the ears and into the temples, you are probably suffering from a condition called cervicocranial syndrome.
The discomfort is usually episodic, aggravated by overloading the cervical spine, such as working on a computer for several hours, looking at a mobile phone, sleeping in the wrong position or using the wrong pillow. You may feel hard lumps in the head that are painful when squeezed. These are trigger points, which are caused by reflex muscle stiffening.
Massaging these points brings relief.

A very unpleasant symptom of cervicocranial syndrome is dizziness, which occurs when changing the position of the head or moving the neck. This is not rotational vertigo as in vertigo, but rather a feeling of loss of balance and instability of the body.
The "ship-like" sensations are usually accompanied by loss of appetite and nausea. Patients may be so dizzy that they are afraid to take a step for fear of falling and do not want to let go of the support.
Pain that radiates sharply from below the shoulder blade may spread to the entire upper limb, often radiating towards the elbow. It is accompanied by pain and tingling in the fingers, which become numb and clumsy.
The limb cannot be manipulated as before, it is painful and weak.
These symptoms belong to the cervicobrachial syndrome. Trigger points are located under the shoulder blades, in the trapezius and other back muscles.
Unilateral reflex muscle stiffening causes asymmetry of the shoulders. One shoulder is positioned higher and more forward than the other. This asymmetrical posture leads to shortening of other muscles such as the pectoral muscles of the chest wall, malalignment of the thoracic spine, and asymmetrical posture of the pelvis and hips.
This creates a vicious cycle of pain that can spread unilaterally from head to toe. This condition is called myofascial syndrome.
Why did pregnancy start the problem?
You ask:
But why do women who were perfectly healthy before start suffering such difficulties?
Up to 12% of pregnant women have back pain.
Why did pregnancy start it?
These 4 main causes are to blame:
1. A change in the body's centre of gravity
As the uterus grows and the abdomen contracts, more of the body bends forward.
The back begins to arch, accentuating what is called hyperlordosis or extreme flexion of the sacral spine. The chin subconsciously drops down and the cervical spine flexes as well.
Full and heavy breasts under the influence of turbulent hormonal changes pull the chest down, the shoulders move forward. Such a spine resembles a paragraph rather than a nice physiological S. Not surprisingly, the pain does not wait long.
2. Hormonal changes
During pregnancy, the body produces a number of hormones. They prepare the woman for a rapid increase in size and also for childbirth, during which the newborn's body passes through the lower pelvic opening.
These hormones, specifically estrogen, progesterone and relaxin, cause the ligaments to loosen, soften and become pliable.
In a growing baby who needs space in the tummy, this is welcome. However, such soft dorsal ligaments allow the spine to sag into non-physiological positions.
3. Lack of movement
Rapid weight gain, large abdomen, aching joints, shortness of breath and fatigue.
With such a body, regular movement is naturally strenuous. Muscles that do not move quickly become cold and stiff.
During normal daily activities, the back sweats quickly. Even with the slightest chill, the back gets cold quickly. Therefore, expectant mothers should take care to do regular relaxation exercises in the form of stretching the muscles and practicing proper breathing. With these exercises, we keep the muscles warm and relaxed.
4. Sleep on one side of the body
It is recommended to sleep on the left side. However, after sleeping in one position for several months, the cervical spine is unnaturally stretched with one-sided stretching of the ligaments and muscles.
An even greater problem arises when a woman has been used to sleeping on her stomach and cannot find a suitable position for undisturbed sleep in a new situation.
The correct solution need not be a puzzle
If the pain comes unexpectedly and acutely, the expectant mother often does not know how to react. She is afraid to use commonly available painkillers so as not to hurt the baby.

Massages and relaxing warm spa treatments are forbidden in pregnancy.
If she wants to see a doctor, she does not know whether the problem is neurological or gynaecological. Finally, she does not want to stress, even though the pain may be unbearable and make normal daily activities impossible.
What about the pharmacy?
When it comes to analgesics, i.e. painkillers, paracetamol is suitable. It is safe in pregnancy in each trimester and also during lactation (breastfeeding).
Another tablet that is found quite often in the home pharmacy is acetylsalicylic acid, known as aspirin.
This is not recommended in the last, third trimester. Otherwise, it should be safe in small doses.
Consult your doctor for any new pain treatment, especially if it is to last for several days.
Your gynaecologist will have a slightly better understanding of the limitations of medication in pregnancy than your neurologist. Therefore, direct this question to him.
For information on medication in pregnancy, see also the article:
Painis not a disease, but a manifestation of a disease. Can we manage it without a doctor?
Heat is important
Try applying dry heat to sore muscles.
Blow-drying, applying a blanket, ironed towel, plasters or warm natural ointments should help.
Like a cotton ball
Get pillows for your bed. Lots of pillows.
Pillows support your body while you sleep.
Put one behind your back and one between your knees to cushion your hip joints. Put another between your feet to keep your legs from swelling. Use a small pillow to support your abdomen. If you sleep on your left side, put a pillow under your right arm to cushion your right shoulder and neck muscles.
Light stretching exercises
Have you heard of so-called post-isometric relaxation?
This is a relaxation exercise where you stretch your neck muscles while breathing properly. This maximum stretch will warm up and relax the muscles.
Another exercise that is advisable to practice from the beginning of pregnancy is the contraction of the pelvic and abdominal muscles.
This way you will relieve your spine considerably. A firm abdominal wall will come in handy during childbirth.
You can train or consciously practice pelvic tilts and abdominal muscle contractions anytime and anywhere. At first you will have to think about it, but after a while this body position will become automatic.
Rotational movements, on the other hand, should be limited. Relaxed ligaments allow the spine, especially in the later stages of pregnancy, greater "excursion". This means a greater than physiologically safe range of motion by which a pregnant woman can inadvertently injure herself.
Suitable sports for cervical spine pain are swimming and water sports or water aerobics. Water is naturally supportive, so movements will be a little easier in the later stages of pregnancy.
However, be sure to dry off quickly after swimming and also take extra care with hygiene.
Simple massages at home
Try taking the help of a tennis ball that you place between your back and the wall. Move from side to side, rolling the ball across your back and applying pressure to achieve a massaging effect.
You can guide your partner to feel for painful lumps (trigger points) on the back, for example under the shoulder blades or in the nape of the neck. He or she can massage them with gentle pressure and circular movements.
Perform any home massage sitting or standing, applying gentle pressure to the back muscles.
The prone position is not recommended, especially in high pregnancy.

Do not delay a visit to the doctor for too long
If the pain persists despite your best efforts, you should see a doctor for a professional assessment.
There are several signs that warn that there could be another, more serious cause of the pain.
These are warning signs, or red flags, that indicate, for example, an inflammatory, traumatic, tumor or metabolic cause of the pain.
These warning signs include:
- the presence of a history of spinal injury
- weight loss
- the presence of a malignant tumour
- use of corticosteroids for other chronic conditions
- substance dependence
- hot flashes
- immunodeficiency diseases such as HIV infection
- intense night pain that wakes you from sleep and responds poorly to analgesics
- night sweats

The neurologist will perform an objective examination to determine whether a neurological deficit is present. He or she will focus in particular on limb paresis (weakness, limited active limb mobility) or sphincter disorders (inability to urinate, absence of sensation of a full bladder, loss of urge to urinate or, conversely, involuntary leakage of urine or stool).
If the diagnosis requires it, an imaging examination is carried out.
X-ray, CT scanning and imaging methods that require the administration of a contrast agent into a vein are completely contraindicated in pregnancy.
Magnetic resonance imaging (MRI), which does not expose the fetus to ionising radiation, is safe. However, the contrast agent gadolinium, which is administered in certain cases during MRI examinations, should not be routinely administered in pregnancy. The risk-benefit ratio, i.e. the benefit of the examination in pregnancy, should always be considered.
Interesting resources










