- Diseases in pregnancy: and management of selected serious peripartum conditions: Binder Tomáš, collective
- Risk and pathological pregnancy: Hájek Zdeněk, et al.
- Modern Obstetrics: Roztočil Aleš, et al.
- Selected Chapters in Intensive Care: Bartůněk Petr, Jurásková Dana, Heczková Jana, Nalos Danie
- solen.cz - Hypertension in Pregnancy
- mayoclinic.org - Preeclampsia
- nhs.uk - Causes, Pre-eclampsia
- medicalnewstoday.com - Everything you need to know about preeclampsia
What is preeclampsia? Is it a risk for pregnancy? Symptoms up to eclampsia

Pre-eclampsia is a serious disease occurring only during pregnancy. It is manifested by high blood pressure, oedema and proteinuria (excessive protein excretion in the urine). It occurs after the 20th week of pregnancy, very rarely earlier. It is a very serious complication of pregnancy and childbirth, which threatens the life of both the fetus and the mother.
Most common symptoms
- Malaise
- Chest pain
- Abdominal Pain
- Headache
- Spirituality
- Cramps in the abdomen
- Nausea
- Head spinning
- Proteinuria
- Double vision
- Tinnitus
- Bleeding gums
- Bleeding
- Gaining weight
- Blue leather
- Indigestion
- Swelling of the limbs
- The Island
- Swollen fingers
- Tremor
- Muscle weakness
- Muscle cramps
- Fatigue
- Anxiety
- Vomiting
- High blood pressure
- Deterioration of vision
- Confusion
- Accelerated heart rate
- Liver enlargement
Characteristics
It is one of the most common causes of premature births with possible consequences for the health of the newborn, as well as maternal and neonatal deaths.
It can develop from full health or build on pregnancy hypertension, but also on previous hypertension developed before pregnancy.
Pre-eclampsia is divided into mild and severe.
It is divided into three forms according to the time of onset of symptoms:
- Early form - symptoms that appeared before the 34th week of pregnancy.
- Moderate form - symptoms appearing after the 34th week to the 37th week of pregnancy
- Late form - symptoms appearing after the 37th week of pregnancy
The early form before the 34th week of pregnancy is usually associated with a malfunction of the placenta and internal organs of the fetus, the function of the adrenal glands and the fetal liver.
The middle and late forms are associated with maladaptation of the maternal cardiovascular system.
Mild pre-eclampsia (late) does not develop from a placental disorder. It is manifested by increased maternal blood pressure at rest, above 140/90 mmHg, swelling of the lower limbs and increased urinary protein excretion.
Severe pre-eclampsia is associated with early and intermediate forms after the 20th week of pregnancy. It is manifested by high blood pressure above 160/110 mmHg, large urinary protein excretion, oedema and rapid progression with complications, even possible fetal death.
Pregnant women who have suffered from high blood pressure before pregnancy also develop pre-eclampsia in some cases. Then we speak of superimposed pre-eclampsia.
Rarely, preeclampsia develops after childbirth, which is referred to as postpartum preeclampsia.
Causes
In the early stages of pregnancy, the fertilized egg implants in the uterus and nestles with the help of villi that help to anchor it in the uterus. While anchored in the uterus during a healthy pregnancy, the fetus receives nutrients and oxygen through the spiral arteries of the uterus.
To accommodate the increased nutrition to the fetus, the arteries undergo remodelling, which begins in the first trimester and ends at 18-20 weeks of pregnancy.
It is believed that in pre-eclampsia, the developing embryos in the uterus are not allowed to properly remodel the spiral arteries in the placental circulation. This causes insufficient blood supply and oxygenation of the placenta. This disrupts the placenta early in pregnancy.
Consequently, the inadequate oxygenation of the placental tissue and its lack of blood supply means that it is unable to provide sufficient nutrients and oxygen for the fetus. The fetus thus fights for its life and begins to produce substances that increase the mother's blood pressure.
These substances in the mother's body lead to inflammatory processes and impaired function of the mother's organs. These are the liver, kidneys, brain. Changes occur in the coagulation system, increased bleeding, narrowing of blood vessels, breakdown of red blood cells. This results in the excretion of protein in the urine, which is a characteristic feature of pre-eclampsia.
In first-time mothers, pre-eclampsia is associated with the immune response of the mother. Pregnancy is something new for her, which increases the risk.
It occurs more often in young women in their first pregnancy, but in older women the risk increases, putting the fetus and mother at risk of life-threatening harm.
Pre-eclampsia in a previous pregnancy is risky in every subsequent pregnancy. If women have experienced a severe form of pre-eclampsia, the next pregnancy is risky and must be carried out under close medical supervision.
Women suffering from hypertension before pregnancy are also at increased risk of pre-eclampsia, as are women suffering from diabetes.
Risk factors are:
- first-time mothers
- longer interval between births, more than 10 years
- premature birth in a previous pregnancy
- kidney disease
- obesity
- higher parental age around 40, when the risk is up to twice as high as for younger women
- associated risk in male foetal pregnancy, due to increased testosterone levels
The woman who has not yet given birth is at greatest risk.
Another risk factor is family history associated with genetics. Others are certain diseases such as diabetes, autoimmune diseases, chronic kidney disease, multiple pregnancies, thyroid disease, epilepsy and migraine conditions.
A reduced risk is after a previous miscarriage or a previous healthy pregnancy with the same partner. Changing partners changes this.
Symptoms
The most common symptom is elevated blood pressure in a pregnant woman. Initially, it manifests itself as normal hypertension, which can make diagnosis difficult.
High blood pressure may develop slowly or have a sudden onset.
More than 50% of women also develop headache with visual disturbances, temporary loss of vision, blurred vision, pain in the epigastrium, fatigue and sometimes nausea and vomiting, which are associated with elevated blood pressure.
Read more about headache in pregnancy in the article .

The main symptoms for confirming pre-eclampsia are (table)
| Hypertension | High blood pressure above 140/90 mmHg |
| Proteinuria | Urinary protein excretion above 300 mg in 24 hours |
| Hyperuricaemia | Increased production and subsequently increased concentration of uric acid in the blood Decreased urinary excretion resulting from impaired renal function |
| Swelling and fluid retention in the body | Manifested by a rapid increase in the weight of a pregnant woman above 500 g per week Swelling most commonly occurs in the lower limbs, but can also occur in the hands, face and with swelling of the whole body |
| Thrombocytopenia | A condition in which there are not enough platelets in the blood Causes increased bleeding |
It is the lack of platelets that can signal HELLP syndrome, associated with a severe form of pre-eclampsia. HELLP syndrome is a label for severe liver damage and breakdown of red blood cells. It occurs in 4-12% of women with pre-eclampsia. It is manifested by nausea, vomiting, upper abdominal pain and headache.
It is a serious life-threatening complication of pregnancy.
Do you suspect that you too may be suffering from pre-eclampsia?
To help you spot the symptoms, also read this article:
How to spot pre-eclampsia and its symptoms in pregnancy? Know the risks
Another serious complication is DIC (disseminated intravascular coagulopathy). It is caused by inflammatory processes in the mother's body, damaging the liver. It is characterized by impaired blood clotting, increased bleeding and the formation of small blood clots that prevent blood flow to the organs. Subsequently, their damage occurs.
You can read more about high blood pressure, its effects on the body and possible complications in our article.
Diagnostics
When certain symptoms such as headaches, vision problems are suspected or present in a pregnant woman, the focus of the examination is to measure blood pressure, perform blood tests and also test for protein in the urine.
It is important to know your blood pressure for pregnancy.
Pathological values during pregnancy are considered to be a pressure of 140/90 mmHg. If a woman has suffered from elevated pressure before pregnancy, further examinations are carried out to catch possible pre-eclampsia early.
A 30 mmHg increase in pressure compared to normal pressure measured at rest twice consecutively, at least 6 hours apart, is considered risky.
When possible pre-eclampsia is suspected, a roll-over pregnancy test is performed between 28 and 32 weeks of pregnancy.
The pregnant woman is placed on her left side. Her blood pressure is measured three times consecutively at 5-minute intervals until a normal blood pressure value is reached. She is then placed on her back and the pressure is measured again at 5-minute intervals. If the lower pressure (diastole) increases by more than 20 mmHg, she is likely to develop pre-eclampsia during pregnancy.
Diagnostic tests after a period of time may show protein in the urine. If protein excretion in the urine is increased, urinary tract inflammation and urinary fluoride testing must be ruled out in the first instance.
Laboratory blood tests. The possible presence of anaemia and the breakdown of red blood cells are investigated. Liver tests are also carried out.
What laboratory values are indicative of the development of pre-eclampsia?
Liver values are elevated on blood examination. Uric acid values exceed the upper limit and proteinuria (protein in urine) is more than 300mg/24 hours.
Physical and palpation examination of the abdominal region and sonography of the fetus are also performed to verify that the condition has not affected its nutrition.
The function of the fetoplacental unit (nourishment of the placenta, fetus and its organs) in a woman suffering from high blood pressure is monitored by various examinations during pregnancy.
Examination of the function of the fetoplacental unit (table)
| Ultrasound biometry | It allows the early detection of the onset of fetal hypotrophy. Ultrasound is used to monitor the growth of the fetus, whether it is growing in proportion to its gestational week and whether it is lagging behind |
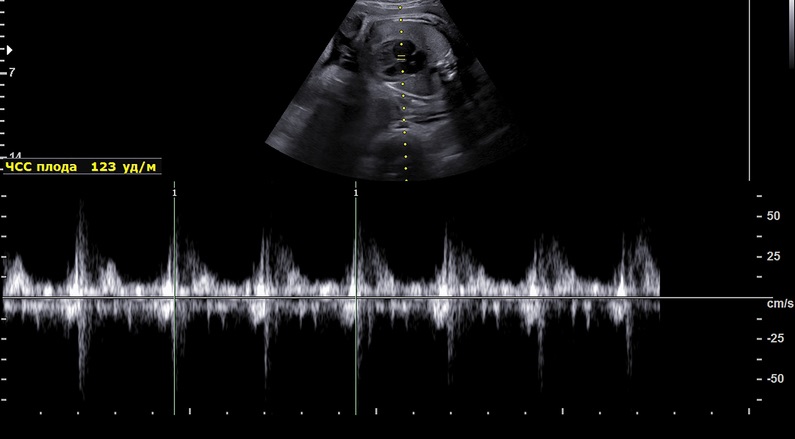
| Doppler flowmetry | Monitoring the flow through the umbilical cord will demonstrate blood flow disturbances |
| Cardiotocography | Reveals the development of inadequate fetal oxygenation |
| Nonstress test | Demonstrates inadequate fetal oxygenation |
| Oxytocin stress test | Performed from the 37th week of pregnancy |
A fetal biophysical examination based on the nonstress test detects inadequate fetal oxygenation and nutrition. It is performed after the 27th week of pregnancy. The examination monitors the natural activity of the fetus, its heart rate during sleep and when awake. It is evaluated based on its movements.
Normally, his heart rate increases with movement.
The oxytocin stress test checks the fetal heart rate using a CTG (cardiotocograph) after administration of an infusion of oxytocin solution. The administration of the solution induces a stress similar to uterine contractions. It determines whether the baby is ready for birth.
Course
The more severe your pre-eclampsia and the earlier in pregnancy it appears, the greater the risks to you and your baby.
First of all, there is a malfunction in the placenta, which is both poorly blooded and nourished. This also causes a malfunction in the nourishment of the fetus.
The fetus fights back and its protective mechanism begins to secrete substances to flow more blood under greater pressure from the blood vessels into the placenta needed for its nourishment. These substances pass through the placenta into the mother's bloodstream and increase her blood pressure.
As a consequence, symptoms and complications occur. In particular, abdominal pain, higher blood pressure, damage to the kidneys, liver, brain, and other vital organs occur due to changes in the inner lining of the blood vessels affected by the increased blood pressure.
If the symptoms persist over a period of time, in addition to abdominal pain, abdominal cramps occur, possibly in the form of twitching. If the disease is not treated, blood vessels in the brain are also disrupted, resulting in disturbances in blood supply and oxygenation to the brain. This very often leads to convulsions throughout the body and disturbances in consciousness. It is common to fall unconscious for short periods of time, suddenly without warning.
Complications of pre-eclampsia are rare, but can cause premature placental abruption, necrosis of the adrenal cortex, liver rupture, cerebral haemorrhage, brain swelling, bleeding disorders and HELLP syndrome.
A direct consequence of untreated pre-eclampsia is eclamptic seizure.
Preeclampsia that is left untreated can lead to serious or even fatal complications for you and your baby.
Complications for the fetus
The most common complication from inadequate placental function and the resulting impaired flow through the placenta to the fetus is growth restriction. In more severe cases, there can be varying degrees of growth retardation that can lead to fetal death.
If the placenta is not adequately nourished, it does not supply the fetus with enough blood, oxygen and nutrients. As a consequence, growth retardation occurs.
Complications also include premature termination of pregnancy and delivery of a premature newborn who is at risk of death.
Preeclampsia and eclampsia
A brief breakdown of the symptoms of pre-eclampsia and eclampsia in the table
| Pre-eclampsia | Eclampsia |
|
|
Pre-eclampsia is one of the late forms of gestosis. It is characterised by high blood pressure, proteinuria, oedema and associated subsequent nausea, visual disturbances and malaise. In some cases it may progress to eclampsia.
Eclampsia is the culmination of pre-eclampsia. It is the most severe form of late gestosis. It is associated with convulsive seizures, loss of consciousness during pregnancy or childbirth and subsequent memory loss.
It occurs mostly in first-born mothers, but it is also possible in repeat births. It is accompanied by hypertensive crisis, decreased urination and excessive protein excretion in the urine. It is a life-threatening condition from which the expectant mother may die.
Read more in the article:
Hypertensive crisis: how is it manifested and treated? High pressure, what threatens health?
This condition is more common in multiple pregnancies.
Before the onset of eclampsia, there is usually severe headache, fogginess and double vision with urge to vomit. Subsequently, tonic-clonic convulsions similar to an epileptic seizure occur.
If a woman develops eclampsia, she should be admitted immediately to the intensive care unit. If complications arise, she may even stop breathing or go blind.
The treatment of eclampsia consists of interrupting the seizure by administering sedatives, magnesium and oxygen. It is necessary to lower blood pressure and ensure sufficient fluid intake, which is especially necessary in severe conditions.
This disease is associated with increased maternal and neonatal mortality. It is therefore recommended to terminate the pregnancy as soon as the woman is stable, either vaginally or surgically by caesarean section.
Preeclampsia and second pregnancy
Pre-eclampsia most often occurs in the second half of pregnancy, sometimes even at the end of the third trimester. It is true that pre-eclampsia is most common in the first pregnancy, but the second pregnancy can also be prone to pre-eclampsia under certain circumstances.
This is when there is a large age gap from the first pregnancy, for example 10 years. If pre-eclampsia occurred in the first pregnancy or if the woman's mother or sister suffered from it, the risk of occurrence is also increased in the second pregnancy.
In this case, it is better to undergo regular preventive check-ups at a pregnancy clinic. During the second pregnancy, preventive use of acetylsalicylic acid derivatives is recommended to inhibit platelet clumping and thus prevent thrombus formation.
How it is treated: Preeclampsia
Treatment of pre-eclampsia: Hospitalization and its goals
Show moreZaujímavé video o preeklampsii
Gallery


Preeclampsia is treated by
Preeclampsia is examined by
Interesting resources
Related










