- solen.sk - Polyneuropathy, doc. MUDr. Edvard Ehler, CSc., Neurological Clinic of PKN, a.s., and Faculty of Medicine, University of Pardubice
- medicalnewstoday.com - What to know about polyneuropathy
- healthline.com - What is polyneuropathy?
- ncbi.nlm.nih.gov - Polyneuropathy
- ncbi.nlm.nih.gov - Peripheral diabetic neuropathy, Bodman MA, Varacallo M.
- mayoclinic.org - Diabetic neuropathy
- ncbi.nlm.nih.gov - Diabetic neuropathy: Clinical manifestations and current treatment.
What is polyneuropathy and what are its symptoms + diagnosis and course
Polyneuropathy mainly affects the nerves of the extremities. Why does nerve damage occur and how does it manifest itself?
Most common symptoms
- Loss of pubic hair
- Limb pain
- Nerve pain
- Leg Pain
- Indigestion
- Swollen fingers
- Tingling
- Slow nail growth
- Erectile dysfunction
- Muscle weakness
- Constipation
Characteristics
Polyneuropathy is a neurological disease that occurs when nerve fibers are damaged due to chronic diseases, toxic exposure or vitamin deficiency. Most often, nerves in the lower limbs and feet are affected.
However, all nerves can be damaged, e.g. nerves controlling the digestive tract, bladder, blood pressure, blood vessels and heart. These form the so-called autonomic nervous system.
Treatment so far has been symptomatic, aimed at relieving pain or alleviating discomfort.
In particular, prevention of nerve damage, which includes careful treatment of existing chronic diseases and a healthy lifestyle, plays an important role.
Peripheral polyneuropathy is a neurological disease. It is caused by damage to the peripheral nerves, those that innervate our body in addition to the brain and spinal cord. The damage is either localised or diffuse.
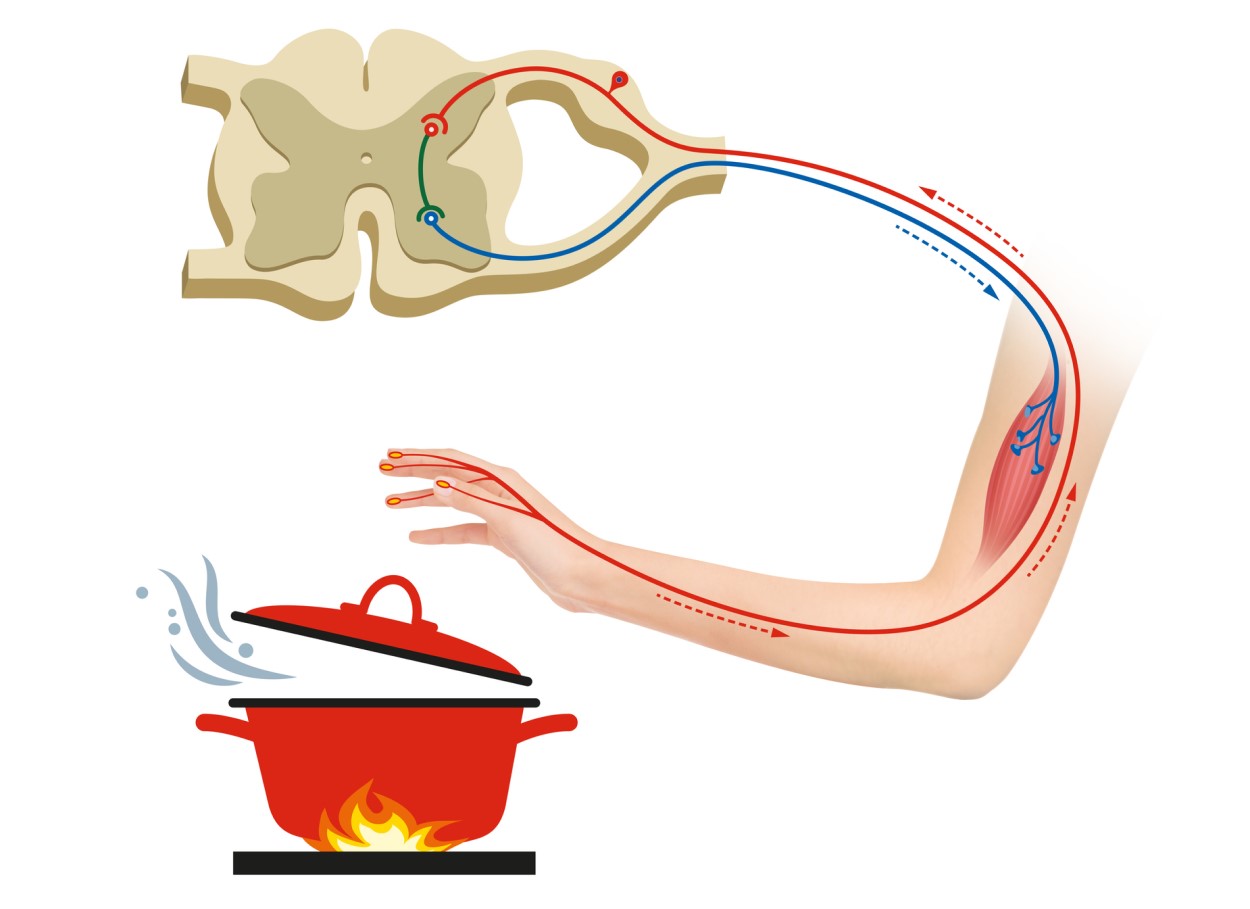
The peripheral nervous system sends information about sensory and motor sensations from the whole body to the brain and spinal cord (central nervous system). There, this information is evaluated, a response is prepared, which is then sent to its place of action, again by way of the peripheral nerves.
This is how, for example, the reflex arc is created.
This is why your hand reflexively pulls away when you touch a hot pot.
The peripheral nerves also send sensory information to the central nervous system, visual and auditory sensations or sensations from within the organs.
Nerves that are responsible for sensory perception, motor skills or internal body processes (called autonomic nerves) can be affected by neuropathy.
The most common symptoms are therefore weakness, numbness or pain, characteristically in the hands and feet. The involvement is always bilateral and almost always symmetrical.
Organ functions, including digestion, urination and circulation, may also be affected.
Causes
Peripheral neuropathy can have multiple causes, most often due to traumatic injury, infections, metabolic diseases, hereditary diseases or toxic damage. The most common cause is diabetes, for example.
However, approximately ⅓ of cases of polyneuropathy fail to elucidate its cause.
According to the type of anatomical structure that is damaged, neuropathies can be divided into:
- Axonal - This type of damage occurs in diabetes, amyloidosis, leprosy, as a result of exposure to toxic substances, or as part of a disease called hereditary axonal polyneuropathy.
- Demyelinating - Very common in autoimmune diseases, in paraproteinemic polyneuropathy or in hereditary demyelinating neuropathy.
- Mixed - In diabetes (diabetes mellitus)
According to the type of damaged nerve fiber, neuropathies are divided into:
- motor lesions
- sensory lesions
- autonomic lesions
- combined lesions
The most common causes of neuropathies include the following disease states:
- Sjogren's syndrome, lupus, rheumatoid arthritis, Guillain-Barré syndrome, chronic inflammatory demyelinating polyneuropathy and vasculitis.
- Diabetes mellitus (diabetes) is the most common cause of polyneuropathy. The incidence of diabetic neuropathy depends on the duration and compensation of diabetes. It is estimated that at the time of diagnosis of diabetes, up to 10% of patients already have some pathological changes in nerve fibres. With a diabetes duration of 25 years, up to half of patients have diabetic neuropathy.
- Infections - Triggers of neuropathy include viral or bacterial infections, including Lyme disease, shingles (herpes zoster virus), Epstein-Barr virus (infectious mononucleosis), hepatitis B and C, leprosy, diphtheria, and HIV.
- Hereditary diseases - Polyneuropathy occurs, for example, in hereditary Charcot-Marie-Tooth syndrome and other congenital syndromes.
- Cancer - The growth of a malignant or benign tumor near a nerve can cause oppression of the nerve, which is damaged by chronic physical irritation and inadequate nutrient supply. Polyneuropathy occurs in some malignant diseases in which a specific immune response is triggered in the body. This syndrome is called paraneoplastic and can also be the very first sign of cancer.
- Bone marrow diseases - These are mainly conditions where an abnormal protein is present in the blood. These diseases are called monoclonal gammopathies. Polyneuropathy also occurs in malignant myeloma, lymphoma and in a relatively rare disease, amyloidosis.
- Other chronic diseases - This group includes kidney and liver diseases, connective tissue disorders and endocrinological diseases such as hypothyroidism.
Causes of neuropathy depending on lifestyle:
- Excessive alcohol use in persons suffering from addiction
- Malnutrition in people suffering from alcoholism leads to vitamin deficiency (avitaminosis)
- Exposure to toxic substances such as industrial chemicals and heavy metals such as lead and mercury
- Use of certain drugs, e.g. chemotherapy to treat cancer or radiation, can cause peripheral neuropathy
- Accidents and injuries, such as car or motor vehicle accidents, falls or sports injuries, can cause severe nerve damage or severance. Wearing a cast or using crutches for a long time causes nerve compression and the development of neuropathy
- Deficiency of B vitamins such as B1, B6 and B12, or hypovitaminosis of vitamin E and niacin, which are crucial for proper nerve function and regeneration
Risk factors:
- Diabetes mellitus is a risk disease for neuropathy, especially if sugar levels are inadequately controlled or untreated
- Intake of large amounts of alcohol, alcoholism
- Chronic vitamin deficiency - hypovitaminosis, especially B vitamins
- Infection with neurotropic viruses and bacteria such as Lyme disease, shingles, Epstein-Barr virus or hepatitis B and C or HIV
- Autoimmune diseases such as rheumatoid arthritis and lupus, in which the immune system attacks its own tissues
- Diseases with reduced kidney, liver or thyroid function
- Toxic chemicals at work or at home
- Occurrence of neuropathy in relatives, e.g. mother or siblings
Symptoms
Nerves in the human body control and regulate all functions. They are generally divided into three types, namely sensory, motor and autonomic nerve fibres.
Sensory nerves receive sensations from the surface of the body, but also from organs. They allow us to perceive sensations such as temperature, pain, vibration or touch.
Motor nerves control the action of muscles and allow movement of the limbs and walking.
Autonomic nerves work independently, without our will. They regulate blood pressure, sweating, heart rate, digestion, gastric and bowel emptying, genital function, and proper eye and bladder function.
Any nerve fibre can be affected by neuropathy. Depending on which of these three types of nerves is damaged, the clinical symptoms of the disease vary.
Symptoms of polyneuropathy include:
- Gradual onset of numbness beginning in the fingers and toes, prickling or tingling in the feet or hands that may spread further throughout the upper and lower extremities
- Sharp, burning, stabbing, throbbing or stinging pain
- Extreme sensitivity to touch, where gentle touches are perceived as unpleasant, e.g. touching a sheet or duvet as burning
- Pain at rest, e.g. pain in the legs, even if they have not been subjected to exertion
- Difficulty with balance, uncoordinated walking, frequent falls
- Muscle weakness in limbs
- Feeling of stretched gloves or socks on limbs
If the autonomic nerves are damaged, symptoms include in particular the following difficulties:
- A constant feeling of cold, thin, dry and cracked skin when sweating breaks down
- Loss of body hair, impaired nail growth, swollen fingers
- Impaired perception of one's own hypoglycemia, which is very dangerous because profound hypoglycemia is a life-threatening condition
- Impaired proper emptying of the bladder or bowel, causing urinary retention and constipation
- Incomplete and slow gastric emptying (gastroparesis) associated with nausea, vomiting and inappetence
- Poor adaptation of the eyes to changes in light (constriction and dilation of the pupil)
- Sexual dysfunction, e.g. erectile dysfunction
- Cardiac arrhythmias
Diagnostics
Peripheral polyneuropathy can have many symptoms and possible causes. For this reason, its diagnosis will also require a wide range of investigations:
A detailed personal history.
The doctor will ask about the medical history including the characteristics of symptoms, lifestyle, possible influence of toxins, drugs, alcohol. From the family history he will be interested in the occurrence of hereditary, oncological and neurological diseases.
Physical neurological examination
Includes a comprehensive examination of the nervous system of the whole body, such as tendon-bone reflexes, muscle strength and tone, sensitivity to certain sensations such as touch or vibration, and the ability to maintain balance and coordination.
Biochemical blood tests and blood counts
Blood is taken by routine venepuncture, i.e. by drawing blood from a peripheral vein. The blood is then examined for vitamin, sugar and waste substances. The blood count may reveal anaemia, inflammatory disease or abnormal immune function.
Imaging examination
A CT (computed tomography) or MRI (magnetic resonance imaging) scan can show displaced discs in the cervical or sacral spine that are pressing on and damaging nerve roots, explaining pain and reduced sensation in the limbs.
Other possible findings may be so-called isthmic syndromes (compressed nerves), tumours or other structural disorders of the nerves or blood vessels.
Electromyography (EMG)
Of the ancillary examinations, the most useful is the EMG examination, i.e. electrophysiological tests. The EMG examination records the electrical activity and conduction velocity of the nerves in the muscles.
Pathological waveforms and blocks in conduction are signs of nerve damage. It is either examined with an electrode from the surface of the skin, or a thin needle (electrode) is inserted into the muscle, which then measures the electrical activity as the muscle contracts.
Skin biopsy
This is one of the more invasive examinations. It is mainly used to diagnose the painful form of diabetic polyneuropathy. A reduction in the density of intraepidermal nerve fibres is monitored in the skin sample taken.
There are also various patches that are applied to the foot. If they change colour during wear, this indicates the presence of nerve fibre damage.
Course
The course of polyneuropathy depends on the cause that triggered the nerve damage.
The thin nerve endings are most susceptible to damage. Therefore, polyneuropathy is localized to the acral parts of the limbs at the onset of the disease. In the most common diabetic polyneuropathy, these are the fingers.
If left untreated, the damage continues and the polyneuropathy progresses. Pain and sensory disturbances rise higher up, to the ankles and calves of the lower limbs.
Over time, all the symptoms of the disease worsen and the patient's discomfort is accentuated.
If medical attention is delayed, the damage to the nerve tissue is at an advanced stage where regeneration is no longer possible. In this case, treatment is limited to symptomatic treatment, i.e. treatment that relieves the symptoms and does not treat the direct cause of the disease.
Prevention
Proper treatment of existing diagnoses
The best way to prevent the development of peripheral neuropathy and polyneuropathy is to conscientiously treat diseases that are at risk of nerve damage, such as diabetes, alcoholism, rheumatoid arthritis, high blood pressure, cancer and others.
Healthy lifestyle
A balanced diet is also important for this disease and its prevention. As the saying goes, we are what we eat. Therefore, try to eat a diet rich in fruits, vegetables, whole grains, lean meats and legumes as a source of protein.
Vitamin B12 deficiency can be prevented by eating meat, fish, eggs, low-fat dairy products and fortified cereals.
Vegetarians or vegans will supplement vitamin B12 mainly with cereals. As they are more prone to hypovitaminosis, they should also take vitamin B12 in supplements, e.g. capsules.
Physical activity is the best medicine. Try to exercise at least three times a week for at least 30 minutes. Targeted physiotherapy and rehabilitation led by a specialist is also excellent.
Try to avoid factors that cause nerve damage. These risk factors include repetitive movements and forced body positions that cause nerve compression, toxic influences such as chemicals at work or in the home environment, smoking and excessive drinking of alcohol.
How it is treated: Polyneuropathy
Treatment of polyneuropathy: Drugs to relieve symptoms and progression
Show morePolyneuropathy is treated by
Interesting resources










