- ROZTOČIL, Aleš and Pavel BARTOŠ. Modern gynaecology. Prague: ISBN 978-80-247-2832-2.
- internimedicina.cz - Vulvovaginitis - inflammation of the vulva and vagina. MUDr. Zuzana Dostálová, Ph.D., MUDr. Romana Gerychová
- solen.sk - Vulvovaginal infection. Solen. Emil Havranek
- verywellhealth.com - Vulvitis Symptoms, causes, diagnosis, treatment and prevention. VerywellHealth. Tracee Cornfoth
Vulvitis: inflammation of the external genital organs of a woman. Causes, symptoms

Almost every woman will encounter some type of vulvar inflammation during her lifetime. Yet this topic is often taboo. How does vulvitis manifest itself and what are its possible causes?
Most common symptoms
- Malaise
- Vaginal Discharge
- Urethral pain
- Lower Abdominal Pain
- Painful urination
- Frequent urge to urinate
- Fever
- Proteinuria
- Blood in the power
- Bleeding after sexual intercourse
- The Island
- Smelly discharge from the vagina
- Itching of the rectum
- Itchy skin
- Itching of the vagina
- Fatigue
- Vaginal discharge
- Reddened skin
Characteristics
Inflammation of the external genital organs of a woman is called vulvitis or vaginitis. It arises from various causes and is a common problem of women of different ages. What are the typical symptoms of vulvitis, treatment options and prevention, you will learn in the article.
External genital organs and vaginal microflora
The external organs of the female genital tract include the labia minora and labia majora, the clitoris and the vaginal entrance (anus).
The outer and inner labia and the clitoris together form the vulva, which is internally connected to the vagina - the vaginal tube. The vagina is no longer anatomically classified as an external organ, but is a link to the internal organs. Its physiological state is therefore very important.
The vagina forms a complex ecosystem that serves to protect against the ingress of infection. The vaginal microflora is an environment in which microorganisms, mainly lactobacilli, are found.
The stability of the acidic environment is ensured by the breakdown of glycogen into lactic acid. In the vaginal area there are different species of bacteria that are in balance with each other.
The state of this ecosystem is individual due to a number of factors such as hormonal changes, age, sexual activity, health status and others.
What is vulvitis?
Vulvitis is an inflammatory disease of the vulva, the external genital area of a woman. Vaginitis, otherwise known as colpitis, is an inflammation in the area of the vagina - the vaginal tube.
Vulvovaginitis occurs when the balance of the vaginal ecosystem is disrupted.
Vulvovaginitis occurs mainly due to an overgrowth of bacteria or yeast, viral and bacterial infections.
In some cases, inflammation is caused by clothing, inappropriate cosmetic products, mechanical irritation or poor intimate hygiene.
The basic manifestation of vulvitis is redness, itching and burning of the area. In most cases, pathological vaginal discharge is also present.
If a woman seeks medical help in time, vulvitis is not a serious disease. However, if the inflammatory process is left untreated, the infection can spread to the uterus and nearby internal organs. This can subsequently cause more serious health complications.
With any symptoms in the external genital area, a gynaecological examination and expert treatment is necessary.
Causes
The causes of vulvovaginitis are diverse.
The etiology of inflammation of the vulva or vagina starts from irritation with an inappropriate cosmetic product, poor intimate hygiene, hormonal changes, disruption of the vaginal microflora (vaginosis), mycosis, up to infection with an infectious sexually transmitted disease.
Inappropriate cosmetic product
Irritation of the intimate area can be caused by a reaction to a strongly perfumed product such as shower gel, bath foam, body lotion, fabric softener or perfumed toilet paper. Irritation can be caused by chemically bleached and perfumed menstrual products.
It is advisable to reach for more natural hypoallergenic products without perfumes suitable for sensitive skin. For intimate hygiene, it is advisable to use intimate shower gels designed to promote vaginal balance.
Improper intimate hygiene
Improper intimate hygiene can lead to an overgrowth of certain microorganisms in the vaginal environment.
The vulva may react to improper intimate soap, inappropriate menstrual hygiene products or contamination from nearby urinary and anal orifices.
Irritation of the vulva can also be caused by overly synthetic, tight clothing and underwear. In combination with sweating and physical activity, the skin reaction may be aggravated. It is advisable that clothing adjacent to the vulva be airy, natural and comfortable to the touch.
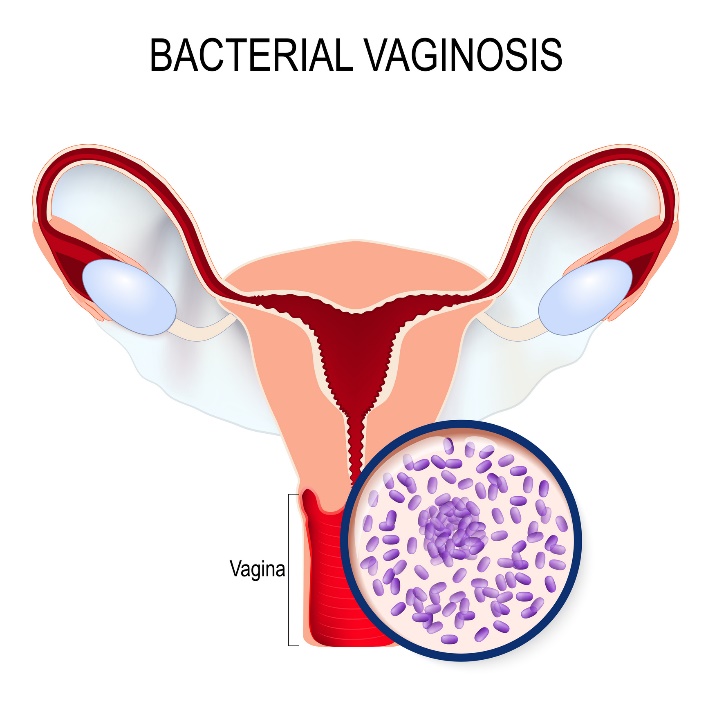
Bacterial anareobic vaginosis
This is a disturbance in the balance of the vaginal ecosystem where there is a decrease in aerobic lactobacilli and an increase in anareobic lactobacilli such as Gardnerella vaginalis.
A transparent to grey discharge with a typical fishy smell is characteristic.
Bacterial aerobic vaginosis
Myco, Escherichia coli, streptococci and staphylococci are common bacteria causing vulvitis and vaginitis.
The characteristic feature is a change in the ratio of aerobic (oxygen-dependent) to anaerobic (non-oxygen-dependent) bacteria, with aerobic bacteria predominating. The main symptom is a thick, yellowish-coloured discharge with a putrid smell.
Fungal infection - mycosis
This is a common infectious agent. In most cases it is a species of Candida albicans, a yeast-like fungus. Women with diabetes are particularly susceptible to fungal infections. So are women who consume excessive amounts of carbohydrates.
Mycosis is caused by an overgrowth of yeast. Its symptoms are a curd-like discharge, a yeasty smell, redness and burning of the vulvar area. On the other hand, a good preventive fighter is the intake of foods with antibacterial effects, such as garlic or propolis.
Although not classified as sexually transmitted diseases, vaginosis and mycosis can be transmitted through sexual contact.
Home treatment of yeast infection of the vagina: How to get rid of mycoses naturally?
Lactobacillosis
Lactobacillosis is a non-inflammatory disorder of the balance of the vaginal environment caused by an overgrowth of certain forms of lactobacilli. Clinically, it is similar to mycosis - a thicker white creamy discharge, burning of the mucous membrane and pain during sexual intercourse.
Frequent urination and difficulty passing urine are also common.
Sexually transmitted diseases
Trichomoniasis and its parasite Trichomonas vaginalis often cause an inflammatory process, abundant thin and foamy vaginal discharge and pain in the lower abdomen. However, often the disease proceeds without symptoms.
Herpes simplex virus is one of the most common viral diseases, causing redness, burning and the formation of small blisters around the vulva.
There are a large number of sexually transmitted diseases (STDs) that cause discomfort and inflammation of the external genitalia of a woman.
Read also:
What are the dangers of changing sexual partners? STDs
How is gonorrhoea transmitted? Symptoms differ between men and women
Risk factors for vulvovaginitis:
- Improper intimate hygiene
- Inappropriate underwear material
- Active sex life
- Unprotected sexual intercourse
- Unhygienic sexual habits
- Hormonal contraceptives
- Weakened immune system
- Treatment with antibiotics/corticosteroids
- Diabetes mellitus (diabetes)
- Excessive carbohydrate consumption
- Menopause and hormonal changes
- Visiting public swimming pools and wellness facilities
Symptoms
The specific clinical symptoms of vulvovaginitis depend on the cause of the disease and the origin of the inflammation. The general manifestation is mainly redness of the vulva and vagina, itching and burning sensation. There is swelling and slight swelling of the external genital organs.
A frequent signal is discomfort and pain during sexual intercourse, dyspareunia. Due to the proximity of the urethra, problems during urination are frequent.
Pathological vaginal discharge is also possible. Its character depends on the cause of its occurrence (bacteria, yeast, virus...).
Frequent manifestations of vulvovaginitis:
- Vulvovaginal discomfort
- Redness of the vulvar area
- Slight swelling of the labia minora
- Itching and burning sensation
- Pathological vaginal discharge
- Pain during intercourse
- Difficulty urinating
Diagnostics
Diagnosis of vulvovaginitis consists in a gynecological outpatient examination.
This procedure is always necessary. External and mild inflammation of the vulva can, without treatment, pass into the internal genital system and cause more serious health complications.
The doctor examines the patient by inspection (looking) and palpation (touching) per vaginam. A superficial or intravaginal ultrasound is also commonly performed to view the internal structures.
In some cases, an examination of the pH level of the vaginal environment or an amine test is performed to detect the presence of bacteria. A urine sample may also be taken or a visit to a urologist may be recommended.
The gynecologist will assess the presence of vaginal discharge, swab the vaginal area and send a sample for culture.
The laboratory will determine the exact causative agent of the disease, and according to the result, a specific course of treatment will be determined. It is necessary to exclude both chlamydial and herpetic infections and other sexually transmitted diseases.
Prevention of vulvar disease
Vulvovaginitis is one of the most common diseases in gynaecological practice. The basis of prevention is the observance of intimate and menstrual hygiene, regular preventive examinations and an urgent visit to a gynaecologist when the problem arises.
Intimate hygiene is the key to the balance of the vaginal environment.
- Wearing airy underwear
- Not sharing underwear with another person
- Using intimate soap
- Limiting perfumed soaps
- Consistent sexual hygiene
- Changing menstrual products frequently
- Avoiding visits to swimming pools and wellness facilities
- Always wipe from front to back
A strong immune system is important for internal balance. Adequate intake of vitamins and minerals, especially vitamins B, C, D and E, folic acid, zinc, magnesium and iron.
It is advisable to limit excessive consumption of saturated fats, simple sugars, caffeine and alcohol.
Natural herbs can be used to prevent genital health. Female herbs harmonize the cycle, promote menstrual comfort and also help with gynecological discharges and inflammation.
Examples include the common borage, white horehound or yarrow. Consumption is possible in the form of herbal teas, tinctures, external compresses and sitz baths. However, consultation with a gynaecologist is recommended.
A sea salt bath is also a good choice, especially for chronic urogynaecological inflammation. It is useful in the treatment of haemorrhoids, skin diseases and also gynaecological problems. Beware of perfumed chemical bath foams and bath bombs.
Herbal tea
Pour 1 cup of boiling water over two small teaspoons of the dried herb. Allow the tea to infuse for 15 minutes and drink twice a day.
Sitting herbal bath
Pour a large amount of lukewarm water over the herb so that it is submerged. Let it sit (infuse) for about 1 day. Boil, let infuse for 5 minutes before using and pour into the bath.
The entire pelvic area should be immersed. The sitz bath takes approximately 20 minutes.
How it is treated: Vulvitis - inflammation of the female organs
How is vulvovaginitis treated? Drugs, antibiotics, topical
Show moreVulvitide is treated by
Other names
Interesting resources










