- ncbi.nlm.nih.gov - Urinary Incontinence, Linh N. Tran; Yana Puckett
- ncbi.nlm.nih.gov - Urinary incontinence in women, Yoshitaka Aoki, Heidi W. Brown, Linda Brubaker, Jean Nicolas Cornu, J. Oliver Daly, Rufus Cartwright
- ncbi.nlm.nih.gov - Urge Incontinence, Shami Nandy; Sudha Ranganathan
- pubmed.ncbi.nlm.nih.gov - An overview of urinary incontinence, Alison Bardsley
- sciencedirect.com - Urinary Incontinence, Gretchen M.Irwin
- pubmed.ncbi.nlm.nih.gov - Management of urinary incontinence, Gemma Nightingale
- solen.sk - Urinary incontinence in a general practitioner's office, MUDr. Ľubomír Lachváč, PhD.
- solen.sk - Urinary Incontinence - Diagnosis and Treatment, Marek Vargovčák
- unilabs.sk - MOUTH INCONTINENCE, prof. MUDr. JÁN ŠVIHRA, PhD.
- health.gov.sk - Clinical standard for physiotherapy of overactive bladder (OAB ) and urge urinary incontinence in women
- health.gov.sk - Clinical standard for physiotherapy of stress urinary incontinence in women
Urinary incontinence: what is it and why does it occur + Types and symptoms

Globally, incontinence is one of the most taboo health complications. Due to its high prevalence in both female and male populations, it is currently a serious economic, social and medical problem. What is incontinence, how to recognize it and when is the right time to consult a doctor?
Most common symptoms
- Urethral pain
- Lower Abdominal Pain
- Painful urination
- Frequent urination
- Frequent urge to urinate
- Increased body temperature
- Proteinuria
- Blood in the power
- Depression - depressed mood
- Fever
- Assisting
- Anxiety
- Reddened skin
- Cloudy urine
Characteristics
Urinary leakage can affect both women and men. However, it is much more common in women.
At the same time, it is a serious social and hygienic problem for each patient.
Urinary incontinence is not considered a separate disease. Rather, we are talking about a symptom that indicates the presence of a functional disease of the lower urinary tract.
The International Continence Society (ICS) currently defines incontinence as a symptom of any involuntary leakage of urine.
Anatomy of the lower urinary tract
To properly understand incontinence, it is important to know the anatomy and function of the lower urinary tract.
The key parts of this system include the bladder, urethra and sphincters.
The wall of the bladder consists of a layer of muscles and an inner lining. The thick layer of muscles is made up of smooth muscles embedded in a tangle of collagen fibres. Collectively, it is called the detrusor. The bladder muscles are not controlled by a person's will.
The inner lining of the bladder is made up of an epithelium called the urothelium.
The bladder is elastic. This allows urine to accumulate in the bladder without creating significant pressure inside the bladder.
When the bladder is empty, the wall is thick and the inner lining lined. When the bladder fills up, the wall is thinner and the inside is smooth.
The volume of the bladder ranges from 250-300 ml. In some cases, however, the inside of the bladder has the ability to expand up to 1500 ml.
With increasing age, the capacity of the bladder decreases.
The normal number of urinations during the day is considered to be 7-8. During one urination, a person excretes approximately 250-300 ml of urine. This volume is usually higher during the first morning urination.
The first feeling of the need to urinate comes when the bladder is filled to about 200-250 ml.
The bladder itself does not have a sphincter. The urethral sphincter is responsible for keeping the urine inside the bladder and is connected to the bladder from the bottom of the bladder. The sphincter is made up of striated muscles and is controlled by our will.
The elasticity of the urethral mucosa, the ability of the urethral muscles to contract, the position of the bladder neck, the degree of support of the surrounding tissues, and the functioning of the nerves located in the pelvic area are also important factors in the retention of urine.
The lower urinary tract performs two basic functions:
- Storage, in which the bladder muscles are relaxed and the sphincters are contracted. This allows urine to accumulate in the bladder.
- Emptying, in which the sphincters are relaxed and the bladder muscles contracted. This allows urine to be expelled out of the bladder.
These two functions are controlled by the nervous system and are activated in accordance with the needs of the body.
Unwanted leakage of urine (incontinence) can occur when the structure or function of individual components of the lower urinary tract is disturbed.
Some of the factors contributing to the development of incontinence include:
- Damage to the connective tissue that fixes pelvic structures to the pelvic walls
- Damage to the pelvic floor muscles that support the urethra
- Reduced function of the transverse striated muscles of the urethral sphincter
- Changes in elasticity and nerve supply to the detrusor
- Changes in the inner lining of the bladder (urothelium)
- Changes in the composition of the urine
- Changes in the central nervous system
Causes
We distinguish:
- Stress incontinence
- Urge incontinence
- Mixed incontinence
- Reflex incontinence
- Incontinence from racing
- Functional incontinence
The most common types of incontinence are stress, urge and mixed incontinence.
Stress incontinence
Stress incontinence is the involuntary leakage of urine occurring during physical exertion and exercise (running, jumping, lifting heavy objects) or conditions such as laughing, coughing or sneezing.
The primary reason for urine leakage is weakening of the bladder closure.
During these activities, increased pressure is generated in the abdominal area. The pressure generated by the impact overcomes the barrier mechanism of the weakened bladder closure, and urine leakage occurs.
Stress incontinence is very often misunderstood as leakage of urine due to a psychological change or state of mind. However, it is leakage of urine solely due to pressure.
The closure of the bladder can be weakened for two reasons. Due to impaired urethral sphincter function or due to hypermobility of the urethra.
Impaired sphincter function can occur after repeated operations in the pelvic region (urological, gynecological, surgical), after injuries to the pelvis or urinary tract, with nervous diseases, with advanced age, as well as with the occurrence of tumors.
In men, it occurs very often after surgical removal of the prostate.
Urethral hypermobility occurs only in women, and only in conditions such as obesity, chronic cough and constipation, childbirth, aging or menopause.
It is related to a weakening of the connective tissues and muscles in the pelvis that serve as support for the urethra and lower bladder.
These tissues are partly involved in the contraction of the urethra. When weakened, they fail to provide sufficient support. As a result, the urethra becomes more mobile and sags under load.
The drop causes a decrease in pressure. The urethra is thus unable to contract and subsequently leaks urine.
Stress incontinence is the most common type of incontinence of all. It is more common in women, especially in middle age (45-55 years).
Urge incontinence
Urge incontinence is understood as involuntary leakage of urine preceded by a sudden and strong urge to urinate. This urge cannot be suppressed.
The cause of this type of incontinence is the lack of a mechanism to dampen the contractions of the bladder muscles, resulting in overactivity of the bladder.
Thus, the problem is exclusive to the bladder. It may be either overactivity of the detrusor, poor detrusor compliance, or over-sensitivity of the bladder.
Urge incontinence as a symptom is part of a larger complex of symptoms that are characteristic of an overactive bladder.
Excessive and uncontrolled bladder activity may result from damage to the central nervous system (stroke, spinal cord injury), multiple sclerosis, infections, inflammation, or tumors of the lower urinary tract.
Mixed incontinence
Mixed incontinence is caused by a combination of stress and urge incontinence. It is more common than urge incontinence alone.
Other types of incontinence
Reflex incontinence is the unwanted leakage of urine due to nerve damage, nerve disease or congenital abnormality.
The result is the inability of the bladder to hold urine and empty itself.
This type of incontinence is associated with urge to urinate, sudden leakage of urine, frequent urination, incomplete bladder emptying, urinary tract infections or loss of bladder volume capacity.
Overflow incontinence is urinary leakage resulting from impaired bladder contractility or bladder outlet blockage.
This results in impaired emptying of the bladder and overfilling. Urine leaks frequently or continuously.
The cause may be nerve damage in the pelvic area (due to disease or after surgery), prostate disease (enlargement, tumor), medications affecting the lower urinary tract, urethral disease (narrowing, tumor), or increased pressure in the pelvic area.
Functional incontinence is urinary leakage occurring in people whose psychological condition, inability to move or other health or environmental problem prevents them from visiting the toilet independently.
These patients have no pathological cause of incontinence related to nerve or urinary tract damage.
A rarer form of incontinence is nocturnal enuresis, in which urine leakage occurs during sleep. The patient does not perceive the leakage and usually wakes up only with the passage of time to the sensation of wetness.
Rare types of incontinence include postural incontinence, where urine leaks when changing position (standing up, bending over), and urine leakage during sexual intercourse.
In all these cases, it is a urethral type of incontinence, i.e. urine leaks through the urethra.
However, we can also mention a specific type of urinary incontinence, namely extraurethral incontinence (extra - outside, urethra - urethra).
This is not incontinence in the true sense of the word, because it is caused by a malfunctioning of the urinary tract. Urine flows out through a pathological route.
As an example, we can mention the outflow of urine through the vagina, due to a tear in the tissue between the urethra and the vagina.
Determining the specific type of incontinence and its cause is crucial for choosing appropriate and effective therapy.
In addition to the individual types, there are several grades of incontinence that are used to assess the severity of incontinence in clinical practice.
- Grade I - This is intermittent leakage of urine drop by drop, with a frequency of no more than 2 times a day.
- Grade II - This is frequent leakage of urine in larger quantities, with a frequency of several times a day.
- Grade III - This is a persistent leakage of urine, with a frequency of several times a day and even at night while lying down. It may also be associated with fecal incontinence.
Prevalence and risk factors for incontinence
Incontinence generally affects women more than men. While women have some type of incontinence in 10-30% of the total, the prevalence in men is less than 10%.
The incidence of incontinence also increases with increasing age. The proportion of women with stress incontinence decreases with increasing age and the proportion of men and women with urge and mixed incontinence increases.
At the same time, women with urge or mixed incontinence report a poorer quality of life compared to women with stress urinary incontinence.
Accurate data on the prevalence of incontinence are relatively difficult to obtain, mainly because of the very nature of this health problem, which causes the patients concerned not to admit to it.
Tabular overview of incontinence figures
|
|
|
|
|
|
|
|
|
Quite a number of factors are involved in the development of urinary incontinence.
The most important and best-studied factors that we consider to be risk factors for the development of this problem include:
- increasing age
- urinary incontinence affects women more often
- family predisposition
- white race
- pregnancy
- childbirth, method and number of births
- menopause
- urinary tract infections
- pelvic floor disease (pelvic organ prolapse)
- operations in the pelvic area which may have damaged the pelvic floor structures
- bronchial and lung disease (a common symptom is coughing, which increases pressure in the abdominal area)
- diseases of the nervous system affecting the spinal cord (e.g. stroke, multiple sclerosis, Parkinson's disease)
- overweight or obesity (higher weight increases pressure in the abdominal area, causing strain and weakening of the pelvic floor structures)
- diabetes
- chronic constipation
- prostate disease and surgery in men
- physical disabilities in which mobility and dexterity are limited
- radiotherapy
- excessive alcohol or caffeine intake
- insufficient fluid intake resulting in high urine concentration and bladder irritation
- smoking (the risk of incontinence is 2.3 times higher in smokers than in non-smokers)
- for example, hormone replacement therapy, certain drugs for heart disease and to lower blood pressure, drugs to increase urine production and excretion, lithium, strong painkillers (opioids), sleeping or tranquillising drugs, antidepressants
Stress urinary incontinence can occur in pregnancy, especially in women. It affects 8-85% of women and will improve after childbirth in most women.
However, women who have experienced incontinence during pregnancy are at increased risk of recurrence five or more years after vaginal delivery (compared with women who have not experienced incontinence during pregnancy).
Symptoms
Incontinence as a hidden but serious problem
In addition to being a health and hygiene problem, urinary incontinence is serious in many other ways.
Urinary incontinence is closely linked to the development of skin problems. When urine comes into contact with the skin, especially with prolonged or repeated contact, the skin is damaged.
Typical symptoms of damage are redness, irritation, pinching, pain, the appearance of rashes or skin infections at the site of contact.
Furthermore, incontinence has a negative effect on the patient's psyche, self-esteem and social ranking. The patient feels ashamed, embarrassed, secretive and refuses to accept incontinence as a problem. This leads to late or no seeking of medical help.
Patients affected by incontinence have significantly increased rates of depression and social isolation. They avoid social events, travel, physical activities, even everyday activities.
The sexual aspect of patients' lives is also significantly affected.
Although urinary incontinence is not life-threatening, it significantly affects and interferes with quality of life.
Incontinence is even an economic problem.
Despite the fact that the number of cases of incontinence is relatively high and increasing steadily, awareness of the problem and seeking professional help are still far behind.
Incontinence is simply still a taboo subject.
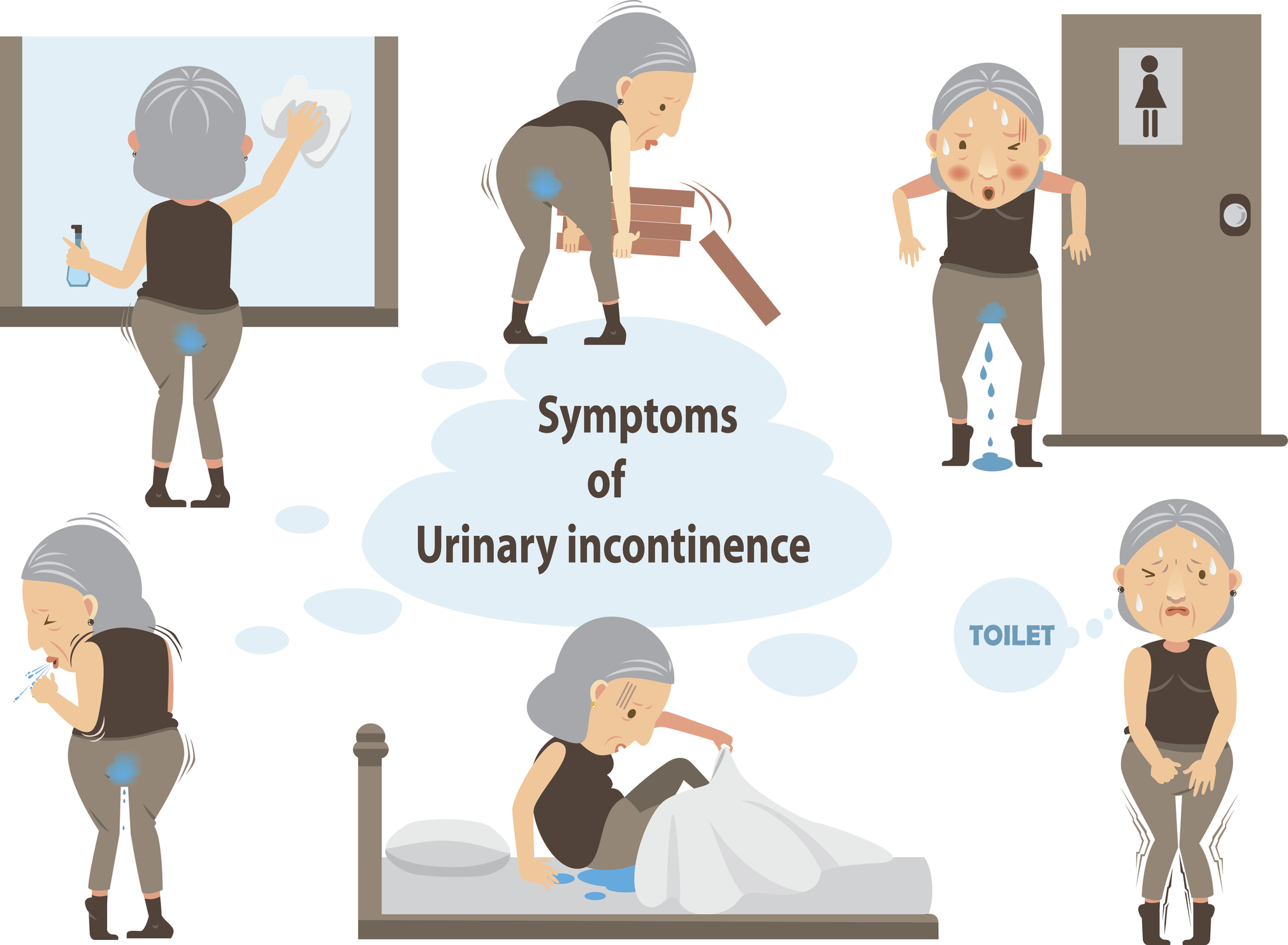
What are the symptoms of urinary incontinence?
It is important to understand that incontinence itself is a symptom. It is a temporary or permanent symptom that tells of some change or health problem.
Urinary leakage as a symptom can vary in nature. There are differences in the volume of urine leaked (by drops or stream), the frequency of leakage (once a day or several times a day, possibly at night), or the situation or conditions in which the leakage occurs.
The nature of the leakage is then indicative of the specific type of incontinence.
It may therefore be closely related to incontinence:
- Leakage of urine during normal activities or during exercise
- Sudden and uncontrollable urge to urinate
- Frequent urination
- Leakage of urine without any previous sensation, urge or stimulus
- Frequent waking at night because of the need to urinate
- Bedwetting at night
- Pain in the abdomen (especially when there is disease or infection in the pelvic floor area)
Diagnostics
The presence of urine leakage alone cannot always be used as a relevant basis for learning the type and cause of incontinence.
Additionally, other aspects such as the presence of factors aggravating incontinence or the overall impact on the patient's quality of life are also assessed.
The general practitioner is the first point of contact for patients with incontinence. His/her role is primarily to identify patients affected by incontinence and to carry out a basic examination.
The aim of the basic examination is to confirm that the patient has a leakage problem, define the causes of the leakage, determine the specific type of incontinence and, if necessary, start initial treatment.
If further investigations are needed, the patient may be referred to a specialist doctor who already has a specialised examination of the patient in question. This is most often a urologist, urogynaecologist or neurologist.
In most patients, the type and cause of incontinence can be determined by a standard diagnostic examination. This consists of the following steps:
- Clinical examination
- Measurement of residual urine
- Laboratory examination of urine
Clinical examination
The first and most crucial step in the diagnostic process is the clinical examination.
It starts with a medical history. This includes obtaining information about the patient's current and previous health, including the presence of nervous diseases and diseases of the genitourinary system.
It details the symptoms experienced by the patient (their nature, duration, frequency of occurrence, amount of urine leaked, use of protective equipment if necessary), the circumstances of the leakage (when and during what activities the leakage occurs), as well as the degree of impact on the patient's quality of life.
This step also assesses the risk factors that influence the development or worsening of incontinence. The physician becomes familiar with all the medications the patient has taken or is currently taking.
Obtaining the patient's medical history helps to further define the urinary leakage problem. It is also a precursor to choosing the most appropriate treatment option.
One way of obtaining information from the patient and at the same time processing and evaluating this information in a relevant way is to use questionnaire methods.
In this respect, a short version of the questionnaire validated by the International Consultation on Incontinence (ICIQ) has been in practice for several years.
It contains questions targeting the frequency and quantity of urine leakage, but also the extent to which it affects the patient's quality of life.
Table: International Consultation on Incontinence Questionnaire
| How often do you leak urine? | |||||||||||
| Never (0) | About once a day (3) | ||||||||||
| about once a week or less (1) | many times a day (4) | ||||||||||
| 2 or 3 times a week (2) | continuously (5) | ||||||||||
| We would like to know what amount of urine you think you leak. What amount of urine do you usually leak (whether you wear protection or not)? | |||||||||||
| None (0) | medium amount (4) | ||||||||||
| small amount (2) | large amount (6) | ||||||||||
| Overall, how much does urine leakage interfere with your daily life? Please mark a number between 0 (not at all) and 10 (very much). | |||||||||||
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
A total score of 0-7 corresponds to stage 1, a score of 8-14 corresponds to stage 2 and a score of 15-21 corresponds to stage 3 incontinence.
The anamnestic examination should be supplemented by a micturition diary.
Micturition = urination.
This is a detailed written record in which the patient writes down the time and volume of each urination, as well as each episode of urge to urinate or leakage of urine over a 24-hour period.
Based on the micturition diary, the doctor assesses the number and time of urination, the volume of urine and the number of leaks, and this greatly assists him in making a diagnosis.
After obtaining the patient's medical history, the next examination is a physical examination. This consists first of assessing the patient's general appearance, i.e. mental status, mobility, hygiene or body mass index.
This is followed by several other physical examinations:
- Examination of the abdominal area by palpation, which detects abnormalities of the abdominal cavity.
- Vaginal examination in women, which mainly examines the vaginal entrance, wall and urethra
- Examination to detect pelvic organ prolapse
- Valsalva manoeuvre
- Rectal examination of the prostate in men
- The presence of swelling is observed, which may be related to frequent nocturnal urination or nocturnal leakage of urine
- Neurological examination to assess anal sphincter sensitivity and tension.
In addition, incontinence tests - Marshall test and pad test - are used as part of the clinical examination.
The Marshall test is a stress test that directly observes the leakage of urine and the intensity of leakage during deliberate coughing. It is performed in the supine or standing position and with a full bladder, but not with a strong urge to urinate.
The pad test involves weighing protective incontinence devices - pads or nappies.
At the beginning of the test, the specific incontinence device is weighed.
The patient drinks 500 ml of fluid over the next 15 minutes and performs standard exercises or activities (walking, running in place, climbing stairs, coughing, getting up from a sitting position, lifting objects, etc.) for 45 minutes.
The incontinence aid is weighed again. A weight gain of more than 2 g (approximately 2 ml of urine) is considered a positive finding. A weight gain of up to 10 g indicates first degree, up to 20 g second degree and more than 20 g is third degree incontinence.
The insert test provides an objective assessment of the amount of urine leakage, as the patient's own estimate may be inaccurate.
Measurement of residual urine
This method of assessment consists of determining the volume of urine remaining in the bladder immediately after urination. We are talking about post void residual urine.
The aim is to assess the degree of bladder emptying. The volume of residual urine is monitored and measured by ultrasonography, scanner or catheter.
Inadequate bladder emptying is defined as a residual measurement of >100 ml, which is approximately one third of the bladder capacity.
Laboratory examination of urine
Urinary laboratory tests are used to assess several parameters such as urine pH, presence of protein and glucose, presence of blood, or specific gravity is also determined.
Urinalysis is recommended as a tool to detect other related conditions besides urinary incontinence evaluation - infections, kidney disease, diabetes or tumors.

After these diagnostic tests have been performed, treatment for incontinence is usually started. Treatment begins in patients who have no other medical problems and no further tests are needed.
These are, for example, patients diagnosed with stress, urge or mixed incontinence. In this case, we are talking about uncomplicated forms of incontinence.
In the case of patients for whom it is not possible to start initial treatment or initial treatment is not effective, further specialised investigations are undertaken.
The reason for not being able to start treatment is the presence of one or more complicating factors. We therefore speak of complicated forms of incontinence.
These complicating factors include:
- Pain
- Presence of blood in the urine
- Recurrent urinary tract infections
- Significant pelvic organ prolapse
- Surgical treatment in the pelvic area
- Previous surgery for urinary incontinence
- Neurological diseases.
Among the specialized examinations, cystometry (which determines bladder capacity, bladder muscle function, changes in pressure inside the bladder, etc.), urethral examination, monitoring of the pelvic floor muscles, or special urodynamic tests are used in practice.
Course
Initially, leakages of urine may be very rare and in negligible volumes, and thus unnoticed by the patient.
Gradually, the frequency and quantity of urine leakage usually increases, especially if the cause of incontinence is not addressed and treatment is not taken.
Incontinence should be seen as a signal to look for the cause and another problem in the body.
It is also important to distinguish between temporary and permanent incontinence.
Incontinence as a temporary problem can occur with urinary and vaginal infections, constipation, in pregnancy, when taking certain medications or foods and drinks.
We can mention alcohol, caffeine, artificial sweeteners, excessively pungent or spicy foods, high doses of vitamin C and so on.
Once the triggering factor is removed, temporary incontinence usually subsides.
Another case is permanent incontinence, in which urine leaks are caused by a physiological change or a medical problem. These leaks persist and are long-lasting.
When is it important to see a doctor?
Although the debate about incontinence is uncomfortable for most affected patients, it is important to talk about it.
And especially in cases where urine leaks:
- They negatively affect the patient's quality of life
- Limit the patient's daily activities and social interactions
- They pose a risk of falls and other injuries when suddenly needing to use the toilet. This is particularly relevant for older patients
- Indicate another, more serious health problem
- As with other health problems, prevention can play an important role in urinary incontinence
Although some types of incontinence cannot be prevented, there are several approaches that can reduce the risk of developing it.
Examples include maintaining a reasonable body weight, limiting smoking, strengthening and exercising pelvic floor structures, avoiding foods and drinks that trigger unwanted urine leakage, avoiding urinary tract infections or constipation, or regular check-ups with a doctor (especially for at-risk patients).
How it is treated: Incontinence - urine leakage
Treatment of urinary incontinence: what drugs will help? + other options
Show moreIncontinence - leakage of urine is treated by
Other names
Interesting resources










