- solen.cz - Toxoplasmosis, MUDr. Ladislav Machala, Infectious Diseases Clinic, FN Na Bulovce, Prague, RNDr. Petr Kodym, CSc., National Reference Laboratory for Toxoplasmosis CEM, SZÚ, Prague, MUDr. Rudolf Černý, CSc, Neurological Clinic, FN Motol, Prague
- solen.cz - TOXOPLASMOSIS IN CLINICAL PRACTICE - THREAT OR MYTH ?, Markéta Geleneky, MD, Clinic of Infectious, Tropical and Parasitic Diseases, FN Na Bulovce, Prague
- prolekare.cz - Issues of some infectious diseases of pregnant women in everyday practice Part I. Bacterial and parasitic diseases
- prolekare.cz - Laboratory diagnosis of toxoplasmosis
- klinickafarmakologie.cz - Malaria, its treatment and prophylaxis
- pediatriepropraxi.cz - Selected viral and bacterial perinatally transmitted infections - Part 3: Toxoplasmosis, doc. MUDr. RNDr. Vanda Boštíková, Ph.D., MUDr. Petr Prášil, Ph.D., doc. MUDr. MUDr. Miloslav Salavec, Ph.D.,prof. MUDr. Pavel Boštík, Ph.D.
Toxoplasmosis: What is it, symptoms and spread? What are its symptoms and how does it affect pregnancy?
Toxoplasmosis is considered one of the most common parasitic diseases in humans.
Most common symptoms
- Malaise
- Abdominal Pain
- Headache
- Eye Pain
- Muscle Pain
- Painful Lymph Nodes
- Fever
- Increased body temperature
- Rash
- Defence
- Disorders of consciousness
- Mood disorders
- Buds
- Squinting
- Muscle weakness
- Muscle cramps
- Fatigue
- Blurred vision
- Deterioration of vision
- Enlarged lymph nodes
- Liver enlargement
Characteristics
Other zoonoses include:
- Campylobacteriosis
- Lyme disease
- toxoplasmosis
- trichinosis
- listeriosis
- tularemia
- leptospirosis
See also:
What is salmonellosis?3x HOW: Does it occur, does it manifest, can you get rid of it?
Leptospirosis
Some history....
In 1908, Nicolle and Manceaux of the Pasteur Institute in Tunisia discovered a parasitic protozoan in an African rodent. They named it Toxoplasma gondii.
The disease in humans was first described by a Czech ophthalmologist, Professor Janků. In honour of Professor Janků, toxoplasmosis is also referred to as morbus Janků in older literature.
In 1969, Hutchison and his team first described the complex life cycle of the parasite. They also pointed out the epidemiological importance of the cat as the definitive host.
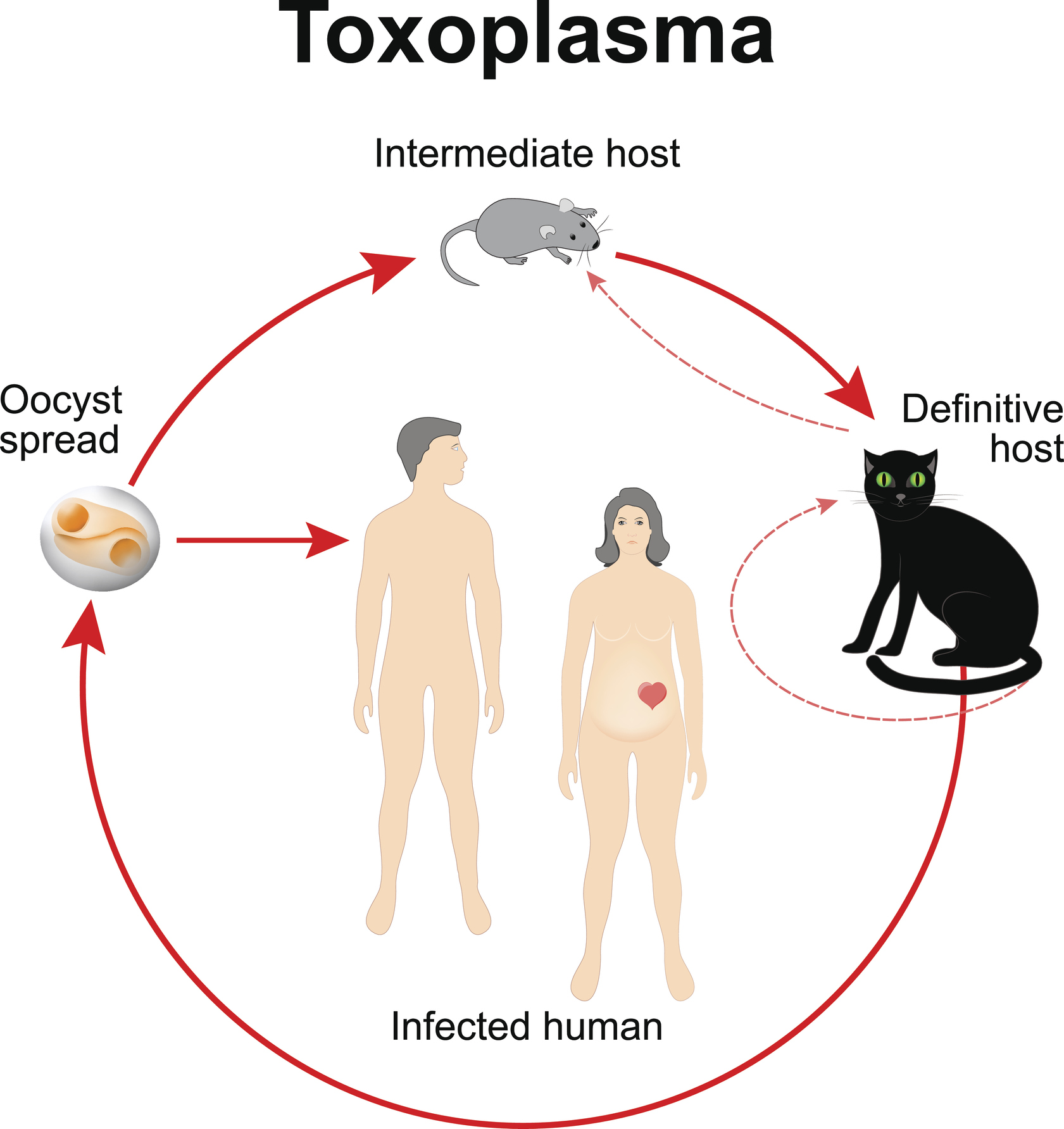
The causative agent of the disease is the intracellular unicellular parasite Toxoplasma gondii. In the definitive host it occurs in three forms. In the intermediate host it forms two forms (tachyzoite, bradyzoite). The developmental forms include:
- Trophozoite (tachyzoite) - Vegetative form. It is characteristic of the acute stage of the disease. It attacks all cells except erythrocytes.
- Bradyzoite - The quiescent form. It is characteristic of the chronic stage of toxoplasmosis. Cysts are found in various tissues (muscles, brain).
- Oocyst - The result of sexual reproduction that takes place only in the intestine of cats and felines. They are very resistant.
The life cycle of this parasite takes place in the definitive host and intermediate host. The definitive host is cats and felines.
Infection of a cat occurs only once in a lifetime. The shedding of oocysts is short-lived. It spreads to the environment via cat faeces.
Oocyst shedding usually takes about 3 to 10 days.
The oocysts mature in the external environment. They become infectious. They then contaminate soil, plants and water. Infection of other animals occurs through ingestion of contaminated food or water.
Intermediate hosts include all warm-blooded vertebrates (cattle, pigs, poultry, rodents). Humans can also be intermediate hosts.
In intermediate hosts, developmental stages may be present in tissues (e.g. muscle, brain) in the form of cysts. Tissue cysts are viable and infectious for a very long time. Even for the lifetime of the individual.
People at risk include:
- pregnant women and their children
- newborns
- immunocompromised patients
- cancer patients
- transplant patients
There is a higher incidence of the disease in people who live in rural areas. The highest incidence of toxoplasmosis is between the ages of 16 and 25.
Causes
- cleaning cat litter boxes, working with soil, eating contaminated raw vegetables.
- through tissue cysts found in food of animal origin - by eating raw or undercooked meat
- blood transfusion
- organ transplantation
- transplacental transmission from mother to child during pregnancy
In general, toxoplasmosis is not transmissible from person to person. The following routes are exceptions:
- blood transfusion and organ transplantation - when an uninfected recipient receives blood or an organ from a donor infected with toxoplasma
- transplacentally from mother to child
According to the World Health Organisation, there are more than 1 million cases of toxoplasmosis caused by contaminated food in Europe.
Symptoms
The manifestations of toxoplasmosis include:
- fever
- joint, muscle, head and neck pain
- enlargement of lymph nodes
- fatigue
- skin changes
- pneumonia

Diagnostics
Laboratory diagnosis is based on:
- serological testing
- histological examination of tissues, lymph nodes and placenta
- direct detection of DNA using molecular biology methods (PCR)
- isolation of gondii by experiments on laboratory mice
Currently, the following methods are used to diagnose the disease:
- enzyme-linked immunosorbent assay and its modifications (ELISA, ELISA capture)
- protein analysis (Western blot)
- molecular biology (PCR, real-time PCR)
The detection of antibodies to Toxoplasma gondii is the basis for a correct diagnosis. The most common antibodies detected by ELISA are IgG, IgM, IgA, IgE, IgG avidity and total antibody titre.
The acute phase of toxoplasmosis is characterised by positivity of IgM, IgA, IgG or IgE antibodies and low IgG avidity. The total antibody titre is high. This phase lasts for one year. Gradually, there is a decline to negativity of the individual classes.
However, IgG positivity persists throughout life. IgG are considered memory antibodies.
The latent phase is characterised by IgG positivity, moderate to low total antibody titres and high avidity.
The following table shows the characteristics of each antibody
| Antibodies | Characteristics |
| IgM |
|
| IgA |
|
| IgG |
|
| IgE |
|
What is avidity of IgG antibodies?
It is used to determine the exact stage of the disease. It distinguishes ongoing infection from chronic or latent infection.
The avidity determines the strength of the binding between the antigen and the antibody. For example, antibodies that form in the early stages of infection do not bind too tightly to the antigen. Their avidity is therefore low.
Course
1. congenital
In pregnancy, acute acquired infection of the mother during pregnancy or in the short period before pregnancy (less than three months) is dangerous.
The risk of transmission increases in proportion to the length of pregnancy. In the first trimester, the risk of transmission is relatively low (6%). In the third trimester, on the other hand, it is already around 60 to 80%.
The following factors influence transmission and the course of infection:
- individual factors - short-term fluctuations in immunity, immunogenetic predisposition
- parasite virulence parameters - infectious dose
The severity of infant involvement decreases with the progress of pregnancy. The earlier the infection occurs, the higher the risk of damage to the infant. A miscarriage may even occur.
Toxoplasmosis most threatens pregnancy in the first and early second trimester.
The information is summarised by trimester in the following table
| Trimester | Characteristics |
| 1st trimester |
|
| 2nd trimester |
|
| 3rd trimester |
|
The manifestations of the disease are non-specific in pregnant women. Most infections are asymptomatic. Some patients may have flu-like symptoms.
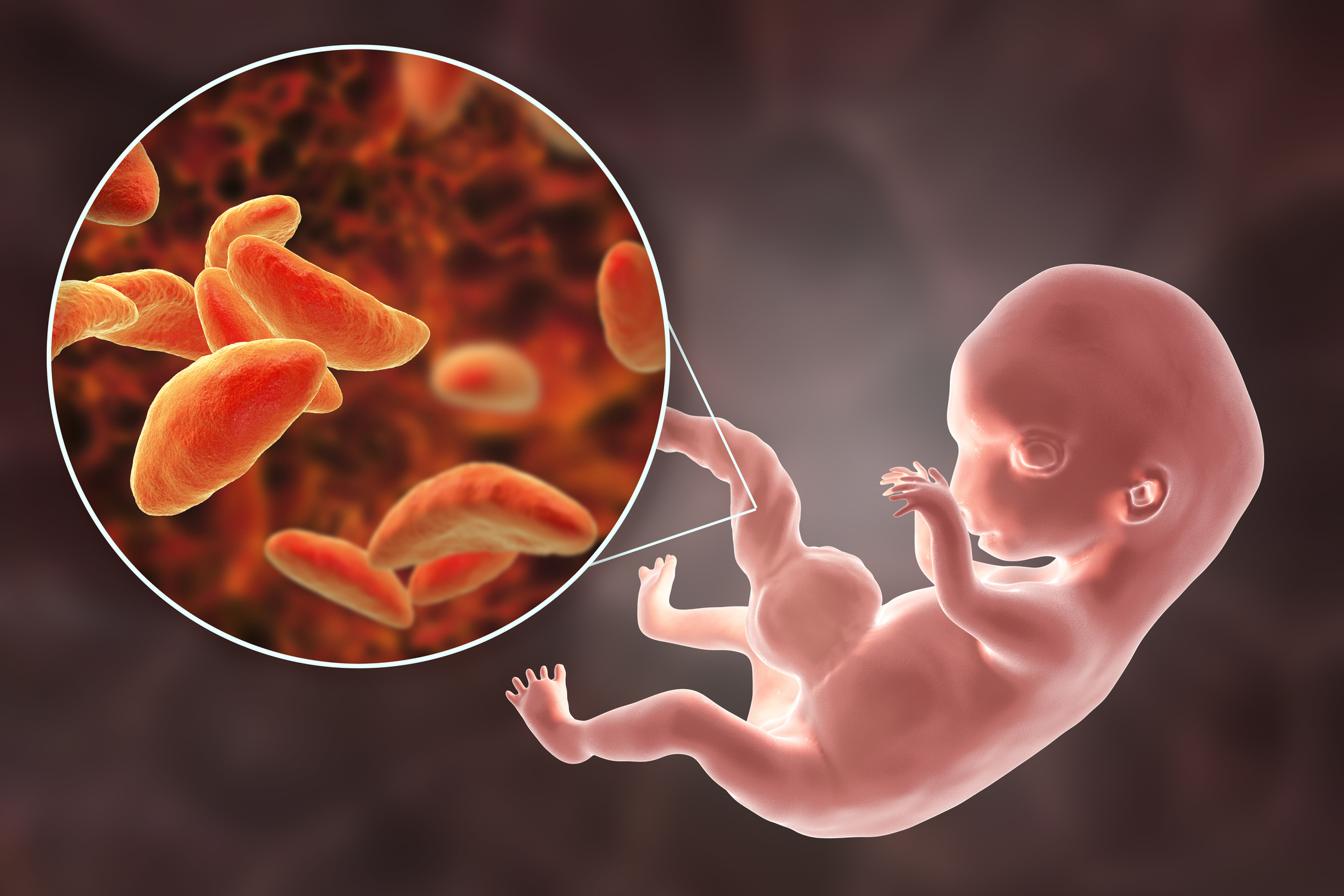
Manifestations of congenital toxoplasmosis in the newborn may occur in two forms:
- Asymptomatic form.
Most often occurs with primoinfection (first infection) of the mother after the 30th week of pregnancy. The newborn is born without clinical signs of congenital toxoplasmosis.
If the disease is not diagnosed early or causal treatment is not initiated, late development of symptoms (psychomotor retardation, chorioretinitis) may occur.
- Symptomatic form
Congenital toxoplasmosis most often occurs before the 30th week of pregnancy. The most risky period is considered to be the 10th to 24th week of pregnancy.
After birth, clinical symptoms appear in approximately 6-10 % of infants. The so-called classic Sabin triad (hydrocephalus, chorioretinitis, cerebral calcifications) occurs in 2 % of infants.
In the neonatal period, fevers, convulsions and persistent jaundice may occur. The latent form is the most common. In the latent form, symptoms of the disease do not appear until later in life.
The following symptoms are typical of the congenital form of toxoplasmosis:
- microcephaly (neurodevelopmental disorder).
- hydrocephalus (caused by the accumulation of large amounts of cerebrospinal fluid in the ventricles or cavities of the brain)
- chorioretinitis (inflammation of the iris and retina of the eye)
- blindness
- epilepsy
- mental retardation
- anaemia
- thrombocytopenia
Can toxoplasma cause neuropsychiatric complications?
The answer is yes. Toxoplasma gondii can infect the central and peripheral nervous system. It can cause severe neurological and psychiatric disorders. Severe psychiatric disorders are associated with asymptomatic chronic toxoplasmosis:
- Schizophrenia
- obsessive disorders
- Parkinson's disease
2. Acquired (acquisition) form
The incubation period of the disease ranges from 1 to 3 weeks. In more than 95% of cases, the course of primoinfection is hidden (inapparent). There is lifelong latent infection.
In some cases, symptoms such as lymphadenopathy, fever, fatigue, malaise, headache and muscle aches occur. Exceptionally, patients develop symptoms such as maculopapular rash, splenomegaly, hepatitis, encephalitis and myocarditis.
When symptoms of the disease appear, toxoplasmosis is divided into the following based on the predominant symptoms:
- The nodular form of toxoplasmosis
Nodular toxoplasmosis is a relatively common form of acquired toxoplasmosis. It appears within 4 to 6 weeks of infection.
Typical localisations include the cervical area, sometimes the axillary (axillary fossa) and inguinal areas. The size of the nodules may vary. They are freely movable, sensitive and tend not to coalesce.
Typical symptoms include:
- subfebrile temperatures
- malaise
- headache and muscle pain
- generalised lymphadenopathy (rare)
- hepatosplenomegaly
The nodular form of toxoplasmosis has a good prognosis. In most cases, symptoms resolve within a few weeks. However, nodular swelling may persist for several months.
- The ocular form of toxoplasmosis
The ocular form of toxoplasmosis is considered to be a serious form of the disease. It can severely damage vision. It can be a form of acquired or congenital (more common) toxoplasmosis. In most cases, it affects only one eye.
The typical characteristic feature is inflammatory involvement of the retina (chorioretinitis). Other typical symptoms of the disease include blurred vision, photophobia, eye pain and scotomas.
Read also:
Visual field loss: what causes scotomas and what is visual field loss?
The untreated ocular form of toxoplasmosis can lead to glaucoma. In some cases, even loss of vision.
What is the prevention of toxoplasmosis?
- As a preventive measure, it is recommended to eat only properly washed vegetables, sufficiently cooked meat.
- After handling raw meat, we must always wash our hands and the kitchen utensils we have used properly. It is best to handle raw meat with gloves.
- Cats should not be fed raw meat.
- The cat's litter box should be cleaned every day, but be careful! Pregnant women should leave this kind of pet care to other family members.
- The area where children play (sandpit, garden) should be protected from cat droppings.
- Hygiene habits should be observed when in contact with animals, potentially contaminated soil and substrate. Gloves should be worn when working.
- The most effective preventive measures are sufficient public awareness, health education and screening of pregnant women.

How it is treated: Toxoplasmosis
Treatment of toxoplasmosis: drugs, antibiotics
Show moreToxoplasmosis is treated by
Interesting resources










