- J. M. Scharf, L. L. Miller, C. A. Gauvin, J. Alabiso, C. A. Mathews, Y. Ben-Shlomo: Population prevalence of Tourette syndrome: a systematic review and meta-analysis. In: Movement disorders: official journal of the Movement Disorder Society.
- J. M. Scharf, L. L. Miller, C. A. Mathews, Y. Ben-Shlomo: Prevalence of Tourette syndrome and chronic tics in the population-based Avon longitudinal study of parents and children cohort. In: Journal of the American Academy of Child and Adolescent Psychiatry.
- M. H. Bloch, B. S. Peterson, L. Scahill, J. Otka, L. Katsovich, H. Zhang, J. F. Leckman: Adulthood outcome of tic and obsessive-compulsive symptom severity in children with Tourette syndrome. In: Archives of pediatrics & adolescent medicine.
- M. M. Robertson, V. Eapen, A. E. Cavanna: The international prevalence, epidemiology, and clinical phenomenology of Tourette syndrome: a cross-cultural perspective. In: Journal of psychosomatic research. Band 67,
- Centers for Disease Control and Prevention: Prevalence of diagnosed Tourette syndrome in persons aged 6–17 years – United States, 2007. In: MMWR. Morbidity and mortality weekly report.
- S. Mills, T. Hedderly: A guide to childhood motor stereotypies, tic disorders and the tourette spectrum for the primary care practitioner. In: The Ulster medical journal.
- S. C. Cohen, J. F. Leckman, M. H. Bloch: Clinical assessment of Tourette syndrome and tic disorders. In: Neuroscience and biobehavioral reviews. Band 37, Nummer 6, Juli 2013, S. 997–1007
- M. H. Bloch, J. F. Leckman: Clinical course of Tourette syndrome. In: Journal of psychosomatic research. Band 67, Nummer 6, Dezember 2009, S. 497–501, doi:10.1016/j.jpsychores.2009.09.002, PMID 19913654, PMC 3974606
- M. M. Robertson: Tourette syndrome, associated conditions and the complexities of treatment. In: Brain: a journal of neurology.
- C. A. Mathews, J. Waller, D. Glidden, T. L. Lowe, L. D. Herrera, C. L. Budman, G. Erenberg, A. Naarden, R. D. Bruun, N. B. Freimer, V. I. Reus: Self injurious behaviour in Tourette syndrome: correlates with impulsivity and impulse control. In: Journal of neurology, neurosurgery, and psychiatry. Band 75, Nummer 8, August 2004, S. 1149–1155, doi:10.1136/jnnp.2003.020693, PMID 15258218, PMC 1739182
- G. M. Jackson, A. Draper, K. Dyke, S. E. Pépés, S. R. Jackson: Inhibition, Disinhibition, and the Control of Action in Tourette Syndrome. In: Trends in cognitive sciences. Band 19, Nummer 11, November 2015, S. 655–665, doi:10.1016/j.tics.2015.08.006,
- N. El Malhany, M. Gulisano, R. Rizzo, P. Curatolo: Tourette syndrome and comorbid ADHD: causes and consequences. In: European Journal of Pediatrics. Band 174, Nummer 3, März 2015, S. 279–288, doi:10.1007/s00431-014-2417-0, PMID 25224657 (Review).
- V. Neri, F. Cardona: Clinical pharmacology of comorbid obsessive-compulsive disorder in Tourette syndrome. In: International review of neurobiology. Band 112, 2013, S. 391–414
What is Tourette syndrome? How to live with this rare disease?
Tourette syndrome is a "rare" genetic disorder affecting about 1% of the population. It affects mostly men. It is characterised by neurological and psychiatric symptomatology dominated by tics, grimaces and obsessive swearing. Mild manifestations often go unnoticed, but the media sensation is the significant disability.
Most common symptoms
Characteristics
The term rare can be used for patients with pronounced symptomatology, but if we consider even the mildest manifestations, it occurs quite often.
It is a lifelong disability that begins to manifest itself at an early age and persists until death.
TS is classified as a mild motor disorder, causing abnormal and involuntary movements.
For a diagnosis to be made, multiple motor tics and at least one vocal tic must have been present for at least one year.
The first signs of the disease can be observed already between the ages of 4 and 6, when they are not very pronounced and mostly go unnoticed. They are not given much importance, rather they are attributed to the personality of the child.
In more than 90% of cases, the symptoms surface between the 10th and 12th, and are most intense in this period of puberty, which is associated with hormone fluctuations (testosterone and androgenic steroids).
After puberty, most sufferers begin to have milder symptoms, and they diminish with age.
In general, the later the onset of symptoms, the sooner they are alleviated.However, there is a small percentage of patients whose symptoms worsen.
History of Tourette syndrome
The first case of Tourette's syndrome was reported in 1825 by the French physician Jean Marc Gasard Itard. The first patient observed was the aristocratic Marquise de Dampierre, a woman of noble birth.
TS was named by French neurologist and pathologist Jean-Martin Charcot after his scholar and French physician Georges Gilles de la Tourette.
It was he who, in 1884, studied at Charcot's behest in the practice of patients with motor disorders at the Pitié-Salpêtrière University Hospital in Paris. The primary aim was to define the differences from hysteria and chorea.
A year later, in 1885, Gilles de la Tourette published a study on patients with convulsive tic disorder, which would be defined as a new and separate clinical category.
The turning point was 1965, when Arthur K. Shapiro began treating TS patients with haloperidol. He is still referred to as the "father of modern tic disorder research".
The possibility that all movement disorders, and hence Tourette's syndrome, have an organic origin increased between 1918 and 1926, at the time of the encephalitis epidemic, due to the fact that encephalitis was associated with an increase in tic disorders.
It was not until 1994 that genetic predisposition and environmental factors were cited as one of the causes.
More advanced knowledge has been recorded since 1999. These have been achieved on the basis of advances in genetics, neurology and pathology.
Causes
- Genetic predisposition refers to the transmission of inherited traits, and therefore genetic defects, from parents to offspring.
- If the disease is not caused by genes, it means that environmental factors have an influence on its development. These are the various exogenous influences acting on the developing nervous system of the fetus.
Although the exact cause of TS is unknown, we do know that the above factors are involved, except that we do not know the exact mechanism of occurrence.
Genetic predisposition of Tourette syndrome
To date, no gene has been conclusively identified as a definite cause of TS. It is thought to involve the simultaneous involvement of hundreds of genes at the same time.
However, several genetic mutations (SLITRK1, HDC, CNTNAP2) have been found that are rare and explain the small number of TS cases.
Thus, tic disorders, also occurring in TS, are probably due to impaired function of cortical and subcortical brain regions. These are the thalamus, basal ganglia and cerebral cortex.
Anatomical models, imaging techniques and post-mortem studies of animal brains reveal disturbances in the parts that connect the cerebral cortex and subcortex, the frontal cortex and the basal ganglia.
It is the neural pathways connecting the basal ganglia to other areas of the brain that transmit information and regulate the control of movements, behaviour, decision-making and learning.
It is believed that involuntary movements, which include tics, grimaces or gestures, are the result of disturbances in these areas.
Noteworthy:
TS patients have anatomically larger prefrontal cortex.
This is probably an adaptive consequence of trying to regulate tics.
With age, its capacity increases even more, which inhibits tics.
Environmental impacts of TS
Certain exogenous factors affecting the developing fetus increase the risk that children with genetic vulnerability will develop TS or comorbid obsessive-compulsive disorder, which in some cases co-occurs in patients with TS.
The most common exogenous factors in the development of TS:
- higher maternal age
- stress
- smoking
- excessive caffeine intake
- alcohol and other drugs
- some medicines
- premature birth
- low birth weight
- low Apgar score after delivery
- autoimmune diseases
- streptococcal infections
Symptoms
It is most often seen in the context of various attention deficit disorders, often with ADHD or obsessive compulsive disorder. Comorbidity with other disorders means that the symptomatology of TS is enriched by the manifestations of these disorders, or their symptoms are in the foreground.
Learn more:
Specific and developmental learning disabilities. Do they affect a child's intellect?
Do you have a hyperactive child? How can you distinguish hyperactivity from ADHD?
Aggression in children. How to handle an unmanageable child?
Some features are common to multiple diagnoses at the same time. For example, TS has manifestations of obsessional psychosis, but may or may not co-occur with this disorder.
Obsessive-compulsive manifestations of TS
Patients with TS suffer from obsessions that occur both alone and with co-occurring obsessive-compulsive disorder.
Obsessions are intrusive, compulsive thoughts and ideas which the patient cannot resist and which force themselves morbidly into his head. They have an irrational basis, provoke unjustified feelings of anxiety and apprehension, and are therefore not easily ignored. They are persistent and lead to compulsions.
Compulsions are meaningless movements, or actions, and rituals that serve to suppress obsessions. When the patient performs the movement, he or she feels relief.
Example:
The patient has a compulsive thought to twitch his shoulder.
If they don't, they feel uncomfortable.
They twitch their shoulder to get rid of the uncomfortable feeling.
Then comes short-term relief, but only until the intrusive thought reappears.
Motor manifestations of TS - tics, sounds, grimaces
Tics are generally sudden, involuntary, repetitive and rhythmic movements of individual muscle groups.
These are movements occurring intermittently in the background of normal motor activity. They are most often observed on the face, but also on other parts of the body.
There are also acoustic (vocal tics), which are manifested by a certain sound. They affect the laryngeal, pharyngeal, oral, nasal and respiratory muscles. Most often these are different sounds, squeaks, whistles.
Tics in TS are involuntary movements of individual muscle groups that are not otherwise explained (disease, deficiency of a substance, substance use).
In some patients, even complex tics appear, such as extending and adducting hands, jumping, kicking, twisting with the whole body.
Noteworthy:
Substances that can induce tics mimicking Tourette's syndrome and at the same time exacerbate the tics of existing Tourette's syndrome are, for example, amphetamines or cocaine.
The intensity and depth of tics are also increased by certain medications or their discontinuation. These include opiates, lithium, antidepressants, antiepileptics, antihistamines...
Compared to tics in other diseases, tics in TS differ at certain points:
- do not come unexpectedly, their predictability is related to the obsession described above - the compulsive thought
- if the patient does not perform a particular movement, he feels tension, a bad feeling that he needs to get rid of
- performed tic brings relief
- tics can be suppressed in some patients, but only for a certain period of time (this applies more to adults, suppression of tics is difficult in children)
- suppression of tics leads to fatigue
- suppression of tics in specific situations leads to their increased increase after a period of suppression
- are not identical in different TS patients
- a particular TS patient has a unique pattern of tics
- tics do not occur in the combination of motion + sound
- tics worsen in stressful situations
- their number and intensity also increases with fatigue, anxiety, depression or illness
- improve when the patient is concentrating on an activity ( watching TV, listening to favourite music)
Example:
A patient with TS is in a work meeting.
He is aware of the inappropriateness of tics in a particular situation.
To some extent it can suppress them for a limited time (duration of the meeting).
After an encounter that has caused an accumulation of obsessive thoughts, he is forced to go to a distant place and let the tics run free.
Table: the most commonly observed tics and consequences
| Tics and dyskinesias | Possible consequences |
| winking | eye pain, headache, dizziness |
| head twitching | neck pain, disc herniation of the cervical spine (tic neck) |
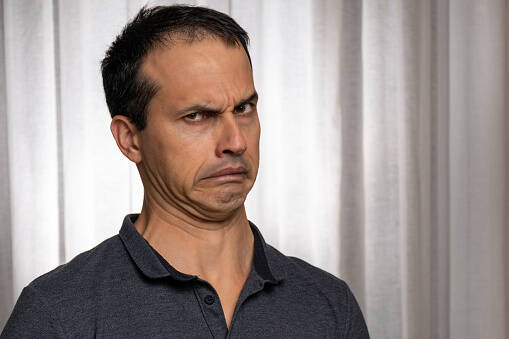
| grimaces | taunts, social isolation |
| burping | gatroesophageal reflux disease (GERD) |
| shoulder twitching | pain with shoulder overload |
| hopping | injuries associated with poor rebounding (abrasions, dislocations) |
| complex motor complexes | various injuries associated with dizziness, falls |
| whistling | social impact |
| screaming | social impact |
Psychological manifestations of TS
The psychological manifestations of Tourette's syndrome include the above-mentioned obsessive tics, which form complexes.
Table with psychological manifestations of TS
| Complex sound tics | Complex motor tics |
|
|
- Coprolalia are feelings of compulsion to use certain verbal expressions, mostly swear words, obscenities and derogatory terms, which we also refer to as "fecal utterances".
The term corpolalia comes from Greek and literally means excrement.
Although this is a typical feature of TS, only 10% of all patients actually suffer from it. - Echolalia means constant repetition of other people's words.
They are most commonly seen in pediatric patients.
This is inappropriate behaviour which, especially in society, can be the cause of interpersonal conflicts and disputes. - Palilalia occurs only sporadically in a minimal number of patients with this syndrome.
It is a repetition of one's own words. - Copropraxia represents a frequent urge to use obscene gesticulations, mostly indecent.
For example, patients stick out their tongue, show their middle finger, imitate masturbatory movements.
These tics are provocative, and can often result in an unwanted physical assault on the ill person at whom they were directed. - Echopraxia is the repetition or imitation of another person's gesticulation, movements, or actions.
In today's society, exhopraxia can be seen as ridiculing others. - Palipraxia, like palilalia, occurs rarely.
It is the repetition of one's own movements.
Neuropsychological manifestations of TS
Although many people think so, people with TS do not experience any major disorders on a neuropsychological level. These can only be observed more significantly in the case of TS in combination with another illness - comorbidities (e.g. ADHD).
Most often, attention disorders, learning disabilities, worse memory are noticeable. Patients do not suffer from more severe intellectual disabilities, although the manifestations of TS can cause learning difficulties.
Some patients with TS even show high intellectual ability, they do not show cognitive deficits.
Other manifestations in TS
- affective irritability - is a condition affecting mood, emotions and overall affect. At the forefront is a pathological mood manifested by a disproportionate emotional reaction of the body with great dynamism.
- raptus - a violent fit of rage directed against the surroundings, but also against oneself. It usually follows a state of anxiety, or it is a rampage stemming from a pathological anxious mood.
- heteroaggression - is aggressive behaviour directed towards an external object or subject. It includes aggressive behaviour towards objects (kicking, smashing, throwing), but also aggressive verbal expressions, gesticulations, even physical assaults on another person.
- self-aggression - is aggressive behaviour directed against one's own person. It is a self-destructive behaviour, even self-harm, where the individual attacks himself/herself. Most often this involves, for example, slapping oneself, biting oneself on the wrist, cutting oneself.
Diagnostics
Given the many manifestations of TS, and some of the typical manifestations for this disease (coprolalia - swearing), it would seem that the diagnosis is easy.
However, it should be noted that the vast majority of TS patients have only mild manifestations, which even close relatives may not perceive as a problem or are not aware that it could be a genetic disease. 20% of them are not aware of the tics themselves.
Unfortunately, even most doctors to this day mistakenly believe that TS is rare, and furthermore, they believe that it typically manifests itself in obsessions, coprolalia, and tics.
At the same time, the shortness of the doctor's visit, the impossibility of longer observation and the patient's ability to suppress obsessions tend to keep the diagnosis hidden forever.
Moreover, the diagnosis is made only on the basis of symptoms or anamnestic data. There are no laboratory tests, screening or imaging methods to confirm or exclude the disease.
Imaging methods and other examinations are relevant only in differential diagnosis, which means that their aim is to exclude or confirm other organic or psychiatric diseases that could cause tics and other symptoms (epilepsy, brain tumour, obsessive-compulsive disorder, thyroid disease, liver disease, Wilson's disease).
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5), still in use today, reveals only TS with more pronounced manifestations.
According to him, one can speak of TS only if the patient has multiple motor tics and at least one auditory tic for a period of one year, and other causes of these symptoms (disease, intoxication, drugs) must be ruled out.
The onset of symptomatology must be before the age of 18.
Course
Although suffering from the same symptoms, but in different intensity, on a different muscle group and with typical deviations.
Initial phase of Tourette syndrome
In most cases of TS, their common feature is the approximate age of onset of the disease, namely 4 to 6 years of age. Children suffer from behavioural inhibition and anxiety states. Tics may or may not be present, at least not initially.
In the initial phase, the tics are brief and not intense enough to make a clear diagnosis. The first tics usually affect the muscles of the face, up to the shoulders, mostly winking, sniffing, grimacing. In many they are mild and do not even draw attention to themselves.
Sound tics are rarely the first to appear; they come after motor tics.
A clue in the diagnosis is the increase in their intensity and frequency during psychological stress, especially at school (papers, oral exams), which is why the teacher often points out the unusual behaviour of the child. The condition is also aggravated by fatigue or an associated illness, which should be noted by the parent.
Conversely, the alleviation of dyskinesias is induced by an activity that requires concentration (sports, painting, playing a musical instrument, singing).
The peak phase of Tourette's syndrome
Between 9 and 12 years, symptomatology reaches its peak. This is usually when the disease becomes fully manifested, and only time will tell how much the patient will remain affected.
Obsessive (repetitive) patterns of behaviour predominate; we also observe anxiety states, sullenness, restlessness, mood changes, marked affective irritability with rants, anger, coprolalia, copropraxia, tics worsening in stressful situations.
Escalating aggression is manifested by frequent bouts of autoaggression and heteroaggression. Self-destructive behaviour, even deliberate self-harm, often occurs.
Since the symptoms are psychological and, so to speak, inappropriate, problems also arise on a social level.
Patients try to hide their disability, avoid society, withdraw into themselves and suffer from feelings of inferiority.
Phase of remission of Tourette's syndrome symptoms
With advancing years - during adolescence, there is a decrease in tics, in some cases to a minimum.
In a few patients, tics and other symptoms become permanent, and only sporadically do childhood tics surface in adulthood.
- patients with a mild form of Tourette's syndrome do not require medical attention and pharmacological treatment
- some patients with a mild form of Tourette's syndrome do not want medical help and pharmacological treatment
- patients with moderate Tourette's syndrome require minimal pharmacological support and psychological help
- patients with severe Tourette's syndrome require a combination of multiple psychopharmaceuticals
- in some patients with a critical stage of Tourette's syndrome, even a combination of drugs is not enough
Can Tourette syndrome be an advantage?
A certain group of scientists, but also patients believe that it is!
There are patients with TS who deliberately refuse pharmacological treatment.
They consider that there are certain benefits of the disease associated with genetic vulnerability, and drugs suppress these benefits.
These benefits have a high adaptive value.
These include, for example, increased attention to detail in the environment, initiative, motivation, increased awareness, etc.
Did you know?
There are many prominent and gifted people in the world who have been diagnosed with TS.
As with Asperger's syndrome, we can include many accomplished athletes, musicians, eminent scientists, and, paradoxically, public speakers.
It is thought that Wolfgang Amadeus Mozart also suffered from this syndrome, but the evidence is not conclusive.
Among the most famous personalities is football player Tim Howard, who owes his illness to better perception and focus on details during the game.
Only recently, the well-known rapper Eminem also confessed to this diagnosis, bringing elements of TS into his work.
The social impact of Tourette's syndrome on the individual
TS, due to its socially unacceptable symptoms, increases the risk of anxiety, depression, and consequent aggressive behaviour, which may not only be a manifestation of TS, but is also often evoked by social rejection, exclusion from the group, even ridicule and bullying.
In the school period, it is difficult for the child to understand why this is happening to him, just as peers do not understand it, and are not aware of the psychological pressure they often exert on the sick person.
In some cases, the child is also misunderstood by the parents and unjustifiably punished.
If dyskinetic disorders are significant, especially vocal tics, which are less socially acceptable than motor tics, the child is usually proposed to study in a special school, in a home environment, or psychiatric monitoring.
However, this is not necessary on the part of the sick person; rather, these consequences flow from society, for which such behaviour is extremely disturbing.
Similar difficulties that children with TS have at school are experienced by employed adults.
Although many TS patients are highly intelligent and also work in high-level positions, the vast majority hold less skilled positions, which is due to the manifestations of the disease, not the intellect.
A slightly decreasing trend of the intelligence curve was observed in patients with TS and concomitant comorbid disease!
It could be said that the biggest impact of this syndrome is the social one.
This is because the vast majority of society still does not understand, is not knowledgeable enough and does not accept the lesser known diseases and symptoms, which undoubtedly include Tourette's syndrome.
How it is treated: Tourette syndrome
What is the treatment for Tourette syndrome? Medications to suppress symptoms
Show moreTourette syndrome is treated by
Other names
Interesting resources










