- ZAVORAL, Miroslav, ed. Mařatka's gastroenterology: pathophysiology, diagnostics, treatment. Prague: Charles University, Karolinum Publishing House, 2021. ISBN 978-80-246-5002-9.
- MARTÍNEK, Jan and Pavel TRUNEČKA. Gastroenterology and hepatology in algorithms. Prague: Institute of Hepatology and Biochemistry of the CAS, v. v. i.: Maxdorf, [2021]. Jessenius. ISBN 978-80-7345-684-9
- solen.sk - Treatment of non-specific intestinal inflammation today. Solen. doc. MUDr. Ladislav Kužela, CSc.
- medicinapropraxi.cz - Idiopathic intestinal inflammation from the point of view of a general practitioner. Medicine for practice. Petr Huvar, M.D.
- healthline.com - Everything you want to know about IBS. Healthline. Jaime Herndon, MS, MPH, MFA
Non-specific inflammatory bowel disease, IBD: What are the types and symptoms?
Nonspecific intestinal inflammation affects mostly young people between the ages of 20 and 35. The incidence of this disease is steadily increasing. The main representatives of IBD are Crohn's disease and ulcerative colitis. Why does inflammation arise and how does it manifest itself?
Most common symptoms
- Malaise
- Abdominal Pain
- Joint Pain
- Increased body temperature
- Cramps in the abdomen
- Diarrhoea
- Rash
- Bloating - flatulence
- Fatigue
- Redness of the conjunctivae
Characteristics
IBD is an abbreviation of Inflammatory Bowel Disease (non-specific intestinal inflammation). This disease can affect any part of the intestinal tract.
The etiology of IBD is relatively unknown, but it has a variety of risk factors for its development.
Types of inflammation, symptoms, diagnosis, treatment options, prevention and much more interesting information can be found in the article.
IBD: Nonspecific inflammation of the intestinal tract
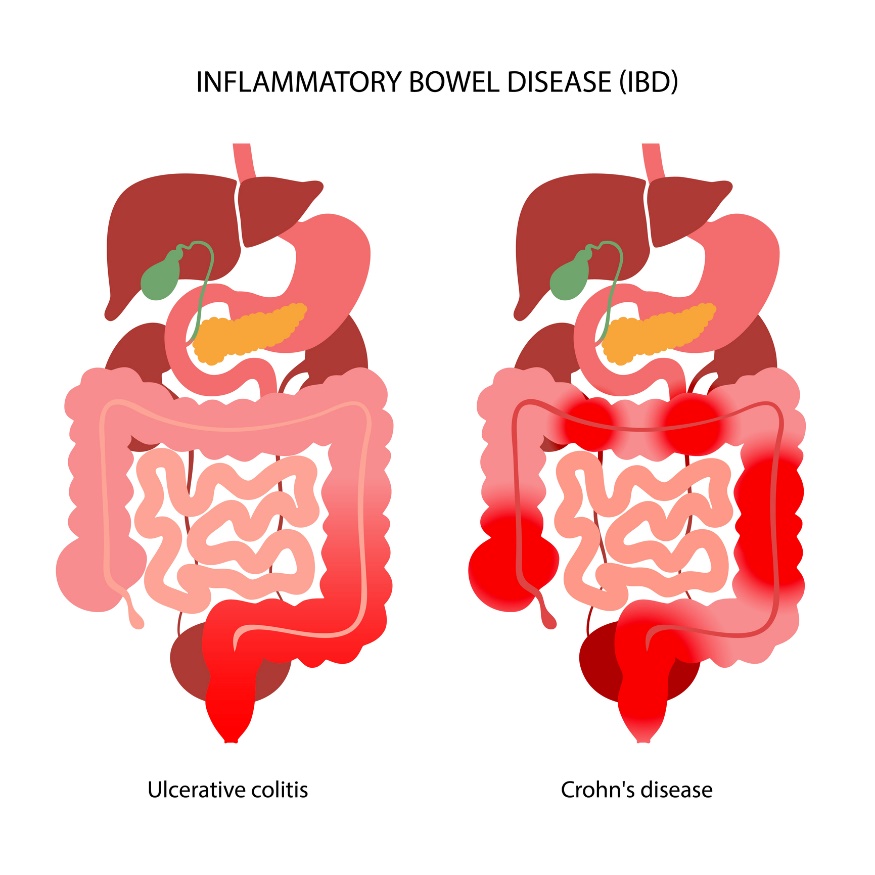
IBD involves idiopathic chronic inflammation of the intestines. The basic phenotypes are referred to as Crohn's disease (CD) and ulcerative colitis (UC). In clinical practice, there is a third, transient but unspecified type of intestinal inflammation.
The prevalence of this disease is increasing. It mainly affects individuals aged 20 to 35 years. However, in recent years, IBD has also appeared in children and the elderly.
Approximately 10% of cases occur before the age of 18.
The incidence of the disease is slightly more common in the female sex. Geographically, the incidence is most common in northern Europe, the UK and North America.
The basic division of IBD:
- Ulcerative colitis
- Crohn's disease
Ulcerative colitis is a non-specific inflammation of the mucosa of the colon. The disease affects the colon in its mucosal and submucosal layers. The inflammatory changes are localized in the rectum and colon.
Crohn's disease is an inflammation affecting all layers of the intestinal wall. It can occur in any part of the digestive tube, from the oral cavity to the rectum. The ileocecal region (small and large intestine) is most commonly affected.
The biggest difference between Crohn's disease and ulcerative colitis is the location of the inflammation. Unlike UC, CD can affect any part of the digestive tract. It is an autoimmune disease.
The inflammatory reaction of IBD becomes chronic because it is "maintained" and recurrent in the digestive tract. Depending on lifestyle and treatment, the disease has individual asymptomatic, resting and exacerbated acute phases.
Thus, non-specific intestinal inflammation includes 2 different lifelong diseases (UC and CD) characterized by remissions (alleviation) and relapses (deterioration) of the condition.
Both UC and CD interfere with physiological digestion and proper absorption (assimilation) of nutrients into the body.
Causes
The cause of this inflammatory reaction is currently unknown.
It is a combination of intrinsic and extrinsic factors that leads to a spontaneously recurring inflammatory process.
As the name of the disease suggests, the cause is not fully understood. The results of studies and research point to the presence of risk or triggering factors.
- Internal risk factor
- External risk factor
Internal risk factor
Genetic factors and family history play a role. Genetic influences are important due to family history of the disease (approximately 15 times higher incidence of CD in first-degree relatives). Co-occurrence of IBD with other genetic diseases also plays a role.
IBD occurs mainly in economically developed countries. The high standard of hygiene in developed countries, combined with an immature intestinal immune system, does not recognise antigens of the physiological intestinal flora and perceives them as pathogenic.
Pathophysiologically, there is a mistranslation of antigen by T-lymphocytes. The antigen translated by enterocytes (cells of the intestinal mucosa) triggers an inflammatory response. In layman's terms, this is a dysregulation of the immune response to common intestinal bacteria.
External risk factor
Experiencing frequent or severe intestinal infections, various gastrointestinal diseases can lead to an inflammatory reaction of the intestinal mucosa in a person with a genetic predisposition.
A poor state of the bacterial gut microbiome is currently being discussed as a trigger for IBD.
Hand in hand with gastrointestinal disease, the frequent use of antibiotics and strong anti-inflammatory drugs is a risk factor.
SIBO: What is Bacterial Intestinal Overgrowth Syndrome? Symptoms...
An inappropriate lifestyle in the form of chronic stress, unhealthy unbalanced diet and smoking are among the main external risk factors.
A diet with an excess of simple refined sugars and a lack of protein and fibre impairs the composition of the intestinal microflora, thereby increasing the risk of inflammation.
Summary of possible causes and triggers:
- Genetic predispositions
- Defective immune system response
- Excessive intestinal infections and diseases
- Imbalance of the gut bacterial microbiome
- Unhealthy diet high in refined sugar
- Frequent use of antibiotics
- Chronic stress
- Smoking and alcohol
Symptoms
Symptoms of inflammatory bowel disease in the exacerbated phase include mainly abdominal pain, abdominal cramps, marked bowel motility, indigestion and diarrhoea (loose watery stools). In the acute phase, fever or fever is possible.
General symptoms include excessive fatigue, general weakness and weight loss. Weight loss occurs due to diarrhoea and poor intestinal absorption.
Rectal bleeding, blood in the stool and diarrhoea are more common in ulcerative colitis. Abdominal pain is more typical for Crohn's disease. However, the symptoms are similar.
Extra-intestinal manifestations are also possible, which appear years later. Examples are joint pain, arthritis, liver damage, eye inflammation and skin manifestations and diseases. Therefore, regular monitoring of the health condition by a doctor is necessary.
Long-term complications of inflammatory bowel disease include an increased risk of colorectal cancer (cancer of the colon).
Summary of symptoms of inflammatory bowel disease:
- Abdominal pain
- Feeling of a bloated abdomen
- Cramps in the abdomen
- Indigestion
- Diarrhea
- Urge to pass stool
- Weight loss
- Presence of mucus and blood in the stool
- Increased fatigue
- Increased body temperature
Diagnostics
The disease is diagnosed and treated by a specialist gastroenterologist. The diagnostic process begins with a basic examination, assessment of clinical symptoms and taking a medical history.
The doctor focuses primarily on diet, lifestyle, associated diseases and family history.
Blood and stool samples are taken routinely. In mild IBD, basic laboratory blood tests may be normal. Their importance lies in excluding other diseases. In more extensive forms of IBD, changes in the blood count may also be detected.
Diagnosis is made by endoscopic examination, including mucosal sampling. The exact type of IBD and its extent (localisation) are determined.
During endoscopic examination (gastroscopy, colonoscopy), when IBD is present, a typical endoscopic picture of the intestinal mucosa is found, which bleeds to the touch. Often ulcerations (ulcers) are present.
Other imaging methods such as CT (computed tomography) and MRI (magnetic resonance imaging) may be indicated.
As part of the extended diagnosis, it is important to differentiate between ulcerative colitis and Crohn's disease. Of the laboratory tests, blood tests for p-ANCA and ASCA antibodies are particularly useful for differentiation.
Course
The course of the disease is described in the section on symptoms.
Prevention of IBD
In the case of genetic predisposition and autoimmune disease, prevention is not possible in most cases. However, external risk factors can be eliminated. These are precisely lifestyle and lifestyle factors.
It is primarily about diet, which should be regular wholesome and balanced. A diet with an excess of simple refined sugar, lack of protein and soluble fibre worsens the composition of the intestinal microflora and increases the risk of inflammatory disease.
Alcohol and smoking tobacco products are risk factors for this disease, as well as other diseases.
Although it sounds like a cliché, daily chronic stress is a potential trigger for many physical and psychological diseases and disorders in the body. Therefore, it is advisable to regenerate the body, get quality sleep and eliminate stress.
Prevention of gastrointestinal (and other) infections and their thorough treatment under the supervision of a physician is necessary. Prebiotics and probiotics are useful to support the bacterial balance of the gut.
Frequent treatment with irritant drugs such as antibiotics, corticosteroids, non-steroidal antirheumatic drugs or hormonal contraceptives is also a risk.
Prevention of IBD:
- A balanced and nutritious diet
- sufficient protein and fibre in the diet
- elimination of refined sugar from the diet
- adherence to food intolerances and allergies
- elimination of daily stress
- elimination of physical and psychological stress
- sufficient regeneration of the body
- prevention of gastrointestinal infections
- treatment of infections under medical supervision
- use of probiotics and prebiotics after illness
- not postponing a visit to the doctor in case of health problems
How it is treated: Non-specific intestinal inflammation - IBD
IBD treatment options - Medications for inflammatory bowel disease?
Show moreNon-specific intestinal inflammation is treated by
Other names
Interesting resources










