- gco.iarc.fr - Lungs
- acsjournals.onlinelibrary.wiley.com - Global Cancer Statistics 2020: GLOBOCAN incidence and mortality estimates for 36 cancer types in 185 countries.
- pubmed.ncbi.nlm.nih.gov - Lung cancer in non-smokers
- pubmed.ncbi.nlm.nih.gov - Lung cancer in non-smokers: disease characteristics and risk factors
- pubmed.ncbi.nlm.nih.gov - Lung cancer in non-smokers: a review article
- mdpi.com - E-cigarettes and head and neck cancer risk - current state of knowledge
- pubmed.ncbi.nlm.nih.gov - E-Cigarettes-a review of the evidence-harm versus harm reduction
- pubmed.ncbi.nlm.nih.gov - An updated review of the human health effects of e-cigarettes
- pubmed.ncbi.nlm.nih.gov - Benefits of smoking cessation for longevity
- solen.sk - Rapid diagnosis of lung cancer- what is the role of the GP?
- linkos.cz - Lung cancer: from histological classification to diagnosis of genetic changes in DNA in tumor tissue and freely circulating in plasma
- pathologyoutlines.com - Lung
- solen.sk - Immunotherapy of lung cancer
- Pneumology and phthisiology for general practitioners, Krištúfek,P., 2021.
- Oncology, Vorlicek J., 2012.
- General oncology, Kaušitz J., Ondruš D. et al, 2017.
- Selected chapters in clinical oncology, Rečková M. et al. 2014.
Lung cancer: what are the causes and risks, symptoms and course?

What is lung cancer? How do the lungs work? Do you know the symptoms of lung cancer?
Most common symptoms
- Malaise
- Chest pain
- Painful Breathing
- Hoarseness
- Spirituality
- Increased body temperature
- Bone Pain
- Indigestion
- The Island
- Stubby fingers
- Swallowing disorders
- Back Pain
- Bone thinning
- Dry cough
- Muscle weakness
- Fatigue
- Damp cough
- Coughing up mucus
- Coughing up blood
Characteristics
What is lung cancer? What are the causes and risk factors of lung cancer? Do you know the symptoms of lung cancer?
How do the lungs work?
Not every cough is just a cough...
Cigarette smoking and e-cigarette smoking?
How can I avoid getting lung cancer?
Also read about the many myths in our society.
Breathing is one of the basic functions of life.
Diseases of the respiratory system include lung cancer.
Lung cancer is characterized by the uncontrollable growth of abnormal cells in the lungs.
Myth:
We often hear in our population: "Many people smoke and don't get lung cancer, so smoking is not that harmful."
Many people imagine ninety-year-old men with a pipe or cigarette who have smoked all their lives and have not gotten cancer. This actually happens in some cases.
But smoking is harmful... And we don't know what our real genetics are...
Let's appreciate a clean deep breath through healthy lungs...
Lungs
Breathing involves the exchange of oxygen from the air and carbon dioxide from the blood.
Air enters the lungs through the larynx, trachea, bronchi and bronchioles into the lung chambers, which are surrounded by blood vessels - capillaries.
The lungs are located in the chest and are protected by the rib cage.
The lungs are divided into right and left parts.
They contain approximately 300 million lung chambers called alveoli.
The total volume of the lungs is 4-6 litres depending on the sex, constitution of the person and condition.
There is a distinction between upper and lower airways.
The upper airways include the nasal cavity, nasopharynx and larynx. The lower airways include the trachea, bronchi, bronchioles up to the lung lobes.
Ventilation is the process by which inhalation (inspiration) and exhalation (expiration) are cycled.
During inspiration, the airway widens and lengthens. During expiration, it narrows and shortens.
In lung disease, basic functions are impaired. Patients experience a reduced quality of life.
Characteristics
Lung cancer is one of the most common cancers in the world.
Globally, lung cancer accounts for approximately 11% of the total incidence of newly diagnosed cancers in both sexes.
In 2020, there were 2 206 771 new cases of lung cancer and 1 796 144 deaths from this cancer.
Lung cancer ranks first in overall mortality from all cancers. It is the most common cancer in men.
The incidence and mortality rates for men are three times higher than for women. The total number of male smokers is decreasing, resulting in lower mortality than in the past.
In contrast, the number of female smokers has been increasing over the last 15 years. This is linked to the upward trend in lung cancer incidence in women (WHO statistics, GLOBOCAN 2020).
The WHO estimates that there are approximately 1.1 billion smokers and 7 million smoking-related deaths annually.
However, lung cancer is now also on the rise in never smokers - LCINS (Lung Cancer In Never Smokers).
This represents a group of people who were never smokers and were not under the influence of passive smoking.
In this group, researchers point to indoor air pollution, occupational exposure, the influence of certain genetic mutations, even infection with HPV and Mycobacterium tuberculosis, hormonal influences, dietary factors and diabetes mellitus.
Classification of lung tumours
The term bronchogenic carcinoma refers to malignant tumours of the bronchi, also malignant tumours arising from the lung parenchyma.
Lung cancer is simplistically divided into groups:
- non-small cell lung cancer (NSCLC)
- Small cell lung cancer (SCLC)
- There are a number of histological types and subtypes, but the above division is for a quick orientation.
Causes
What are the causes and risk factors for lung cancer?
Risk factors
The most common causes are...
Smoking
- Approximately 80-90% of lung cancers in men and 50% in women are caused by long-term exposure of the lungs to cigarette smoke.
- Smoking is the cause of 85-90% of lung cancers.
- 70% of tar from cigarette smoke is deposited in the lungs.
- Smokers have a 30 times higher risk of lung cancer compared to non-smokers.
- Smoking cigars, pipes and marijuana also increases the risk.
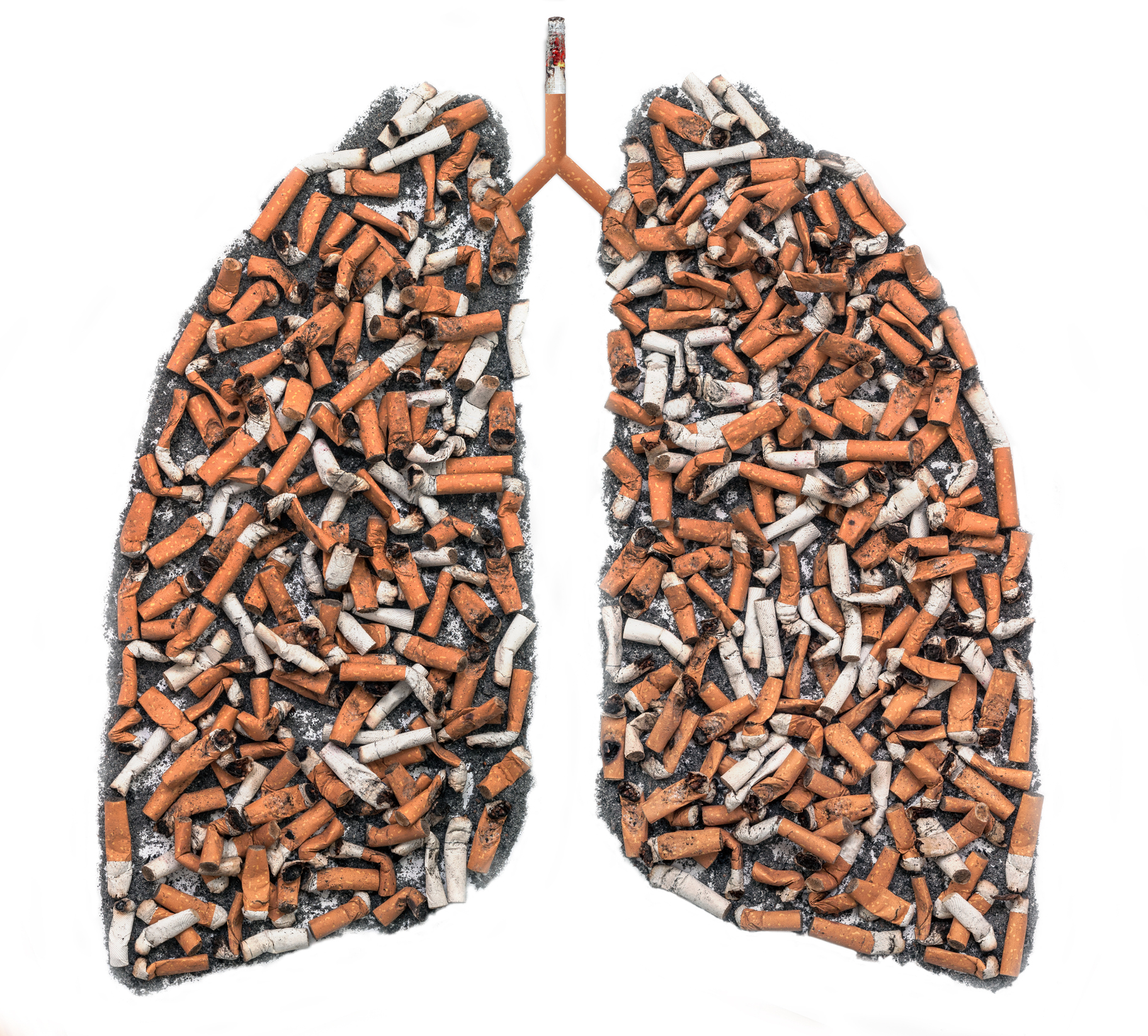
Many epidemiological studies have clearly demonstrated the role of tobacco smoking in the development of lung cancer.
The main carcinogens include polycyclic aromatic hydrocarbons, aromatic nitro compounds, nitrosamines, aldehydes, butadienes, metals - chromium, nickel, cadmium, polonium and others.
The risk ratio of lung cancer in smokers compared to non-smokers is 9.2-14 : 1. When smoking more than 20 cigarettes a day, it is 14.7-25.1 : 1.
A major influence on the increased risk of lung cancer - even more than the number of cigarettes - is the length of exposure of the lungs to tobacco. So it depends on how long a person smokes.
Myth: Smoking is my business and I am only harming my health...
There are now many clinical studies with laboratory findings, epidemiological evidence that involuntary (passive) smoking can cause lung cancer.
The International Agency for Research on Cancer (IARC) was the first international organization to describe that "involuntary smoking", i.e. inhaling cigarette smoke produced by another smoker, is a proven human carcinogen.
Second-hand smoke is a serious risk factor!
Especially if one lives in the same household as an active smoker and smokes directly in the home.
Unfortunately, we are increasingly seeing the alarming image of a smoking parent right next to a helpless child!
Other risk factors:
- Carcinogenic chemicals - asbestos, arsenic, chromium, nickel, silicon, exhaust fumes from internal combustion engines.
- Radiation - radiotherapy, radon
E-cigarettes
Smoking electronic cigarettes is a "hot topic" for lung cancer.
In recent years, we have seen an increase in the smoking of electronic cigarettes, so-called e-cigarettes.
There is a general belief in the population that they are not harmful at all or that they are "healthier".
Compared to conventional tobacco smoking, lower levels of toxic and carcinogenic substances were initially described. However, this controversial topic is the subject of scientific research. There is still a lack of long-term conclusive data.
What is certain is that there are no health benefits from smoking electronic cigarettes and that we do not inhale any vitamins.
At present, studies point to worrying levels of toxic substances, nicotine and carcinogens for the lungs comparable to conventional smoking.
Data have been published on a lower risk of respiratory infections, some lower levels of toxic substances, but only in the short term.
A recent multicentre study in 2020 points to the same risk of head and neck cancers as conventional smoking.
E-cigarettes also contain unstudied additives with questionable toxicity risks and their questionable breakdown in the metabolism of the human body in the long term.
Most clinical studies agree that a definitive assessment of the lower toxicity of e-cigarettes is not yet possible.
Health organisations and experts in this field are concerned worldwide about the significant impact of e-cigarettes and the enormous increase in nicotine dependence among adolescents.
I'm going to stop smoking...
Smoking is not a habit. It's an addiction. That's why the real struggle to quit smoking for good is difficult.
Even a small amount of cigarettes a day (1-2 cigarettes) is smoking. Cutting down on smoking is not the same as quitting. Medications containing nicotine will help ease withdrawal symptoms.
Myth: I haven't smoked for several months, I've cleaned up my body...
Research has found that it takes about 12 years after the last cigarette for a smoker's lungs to adapt to those of a non-smoker.
The benefits to the body are dependent on the length of time without smoking until complete cessation.
It is obviously most advantageous to stop smoking at a young age. Before the age of 35 years, life expectancy has been described to increase by 6.9 to 8.5 years in men and 6.1 to 7.7 years in women compared with continuing smokers.
It always makes sense to quit smoking.
Symptoms
Symptoms of lung cancer
- chronic cough
- aggravation of chronic cough
- in smokers, a change in the nature of the cough!
- coughing up mucus with a mixture of blood to massive coughing up of blood
- shortness of breath, feeling of lack of air (dyspnoea)
- pain in the chest area
- recurrent pneumonia
- bone pain to pathological bone fractures
- general weakness, fatigue, weakness
- weight loss to severe weight loss (cachexia)
- neurological symptoms (for secondary lesions - metastases to the central nervous system)
- symptoms depending on the location in the presence of other distant metastases
- severe complication - superior vena cava syndrome (when tumour oppression and blood flow restriction through the superior vena cava)
- manifested by hoarseness, swelling of the face, eyes, neck, upper limbs up to discolouration, significant conjunctival congestion, tinnitus, chest pain up to breathing and swallowing disorders, the condition may culminate in life-threatening oedema of the larynx.

Diagnostics
The basis is a thorough physical examination of the patient and medical history.
Auscultation of the lungs is one of the first examinations that can reveal diseases of the respiratory system.
A negative finding on chest auscultation does not rule out lung cancer.
The patient should be examined by a pulmonologist when the above difficulties occur.
Smoking and a positive family history are aggravating factors.
The first choice for imaging examinations is a chest X-ray. CT (computed tomography) of the lungs provides an accurate view. In some cases, PET-CT (positron emission tomography) can be used in the diagnosis.
Especially in the case of lung cancer, the patient waits at each step of the diagnosis. But the tumour does not wait.
Do not ignore the symptoms, see a doctor in time.
It is important to know at the outset during the basic diagnosis and staging (classification of the clinical stage) that the patient does not have small cell lung cancer.
Untreated small cell lung cancer leads to death within approximately 6 weeks. If inadequate treatment is given in the limited stage of the disease, waiting for treatment will substantially worsen the patient's outlook.
The change from localised 'limited' disease to advanced 'extensive' disease means a change in median survival.
For non-small cell lung cancer, the impact of a potentially longer diagnosis on survival is more modest than for small cell lung cancer.
Laboratory testing
Standard blood counts, biochemistry and oncomarkers (SCCA, CYFRA, NSE, CEA) may be helpful.
Bronchoscopic examination
In this examination, a sample is obtained for cytological and/or histological examination.
It is an endoscopic examination. It may not be comfortable for the patient but has a very high diagnostic value.
It is also used in treatment as a so-called therapeutic bronchoscopy, e.g. to stop bleeding (massive coughing up of blood), insertion of stents (special tubes to widen the airways in case of tumour oppression), laser treatment of tumour obstructions, bronchoscopic suctioning of mucus in case of stagnation in the airways, e.g. after surgical procedures, etc.
How is bronchoscopy performed?
In bronchoscopy, the doctor uses a thin flexible or rigid tube (bronchoscope) with a light and camera to view the airways from the inside.
He can thus directly see and assess the condition of the airways, detect diseases, inflammation, tumours and take a sample for further analysis (histological, cytological, microbiological examination, etc.). This direct visualisation of the airways is irreplaceable.
Prior to the actual start, the patient is given a treatment to relax and calm him/her, called analgosedation. The doctor also injects a numbing spray (anaesthetic) into the nasal cavity and throat.
General anaesthesia is used less often. It is used more in cases where a so-called hard (rigid) bronchoscope is needed.
The examination is relatively quick and painless. It takes about 20-30 minutes. It depends on whether tissue samples need to be taken. The doctor takes out the bronchoscope, finishes the examination and the patient goes home.
You should not eat or drink before the bronchoscopy (about 6 hours). Also, after the examination, the patient should not consume anything.
The airways are irritated and food or drink could be aspirated, for example.
Throat irritation, sore throat or hoarseness may be transient in some patients.
If you follow the doctor's instructions, there is no need to worry.
The basic sampling techniques for bronchoscopic examination are:
- abrasion with a brush (brushing) for cytological analysis
- forceps biopsy (excision) for histological examination
- bronchial lavage
Other options are transbronchial needle aspiration biopsy (TBNA). It is used in specific indications, e.g. tumour tissue is located in the so-called submucosa, in the absence of endobronchial changes.
In autofluorescence bronchoscopy, the tumour is illuminated by ultraviolet light and fluoresces differently from the healthy surrounding mucosa.
Endobronchial ultrasonography (EBUS) is an investigative method that allows ultrasonographic imaging of the tumor surroundings as well as material collection.
Cytological diagnosis precedes definitive histology in the diagnostic process. It is a useful landmark examination method. It allows rapid orientation to distinguish reactive changes from tumor changes.
We often encounter the finding of water in the lungs (pleural effusion). Water in the lungs can have various causes and occurs in a number of diseases. One of them is lung cancer. Cytological examination is very useful in decision making.
Histological examination of the tissue is indispensable for the diagnosis of malignancy. In the field of practical medicine, the progress of science brings new findings in the field of molecular diagnostics (immunohistochemistry, genetic testing, etc.).
The treatment of patients using genetic and molecular biological analyses opens up therapeutic possibilities.
Knowledge of individual mutations of EGFR, ALK, MET, ROS and other genes, isolation of circulating tumour cells from blood, so-called liquid biopsy, is of great diagnostic and therapeutic importance.
Videothoracoscopy (VATS) is a surgical procedure in which the surgeon enters the chest through a small incision. A camera is inserted into the chest and the image is transmitted to a monitor.
Using special endoscopic instrumentation, diagnosis of suspicious (suspected) malignant lesions, resection and definitive biopsy are possible.
In case of significant tumour effusions, a diagnostic and therapeutic procedure called talcum powder is possible. A special talcum powder is injected into the pleural cavity.
The layers of the pleurodesis are then joined together. The effusion should not form any further.
In oncology, you will come across the following terms
Grading - evaluation of the degree of differentiation.
Tumours that are well differentiated closely resemble the tissue from which they originated.
Conversely, tumours that are poorly differentiated are characterised by marked cytological and architectural changes in the cells. They have a poorer prognosis.
In oncology, we also encounter so-called anaplastic tumours, meaning that they are undifferentiated and their histogenetic classification is problematic.
Staging is an assessment of the stage of the disease based on the size of the tumour, the extent of local involvement, the condition of the regional lymph nodes and the presence or absence of distant metastases (secondary foci).
TNM classification - basic general classification:
- T - category
- T0 - absence of tumour
- Tis - in situ (non-invasive tumour)
- T1 - small or minimally invasive tumour in the primary organ
- T2 - larger or more infiltrating tumour in the primary organ
- T3 - larger and/or infiltrating the margins of the primary organ
- T4 - very large and/or very infiltrating tumour or tumour spreading beyond the primary organ
- N - category
- N0 - no lymph node metastases
- N1 - regional lymph node involvement
- N2 - extensive regional lymph node involvement
- N3 - distant lymph node involvement
- M - category
- M0 - no distant metastases
- M1 - presence of distant metastases
Clinical stages of the disease
Early stage I to clinical terminal stage IV.
Complete remission - complete disappearance of oncological manifestations (duration min. 4 weeks).
Partial remission - partial disappearance of oncological symptoms (duration min. 4 weeks).
Disease progression - formation of new lesions, enlargement of original lesions according to specific criteria.
Disease stabilization - response to treatment, between partial remission and disease progression.
Course
Lung cancer often becomes clinically apparent only at an advanced stage.
For smokers, lung cancer should be considered during outpatient screening, especially for those who work in a high-risk environment, with weakness, weight loss or worsening cough.
A distinction is made between primary lung cancer arising from this organ and secondary cancer localised in the lungs (metastases).
If the lung tumour spreads, metastases may be present in the brain, bones, liver, etc.
Before describing the symptoms of lung cancer itself, it is useful to understand cough and its types in more detail.
Cough
- Acute cough - lasts less than a week
- Subacute cough - lasts up to 8 weeks (for infections)
- Chronic cough - lasts more than 8 weeks (usually does not subside spontaneously, significantly impairs quality of life)
What kind of cough bothers you? Dry, irritating cough? Damp cough with mucus production?
- Morning cough
- morning cough until coughing up sputum
- dry cough
- dry cough associated with pain behind the sternum (very often in patients as a side effect of very effective heart drugs called ACE inhibitors)
- cough associated with exertion
- cough associated with shortness of breath
- cough associated with chest wheezing and shortness of breath (often in asthmatics, especially in the morning and after waking up)
- dry cough associated with mucous membrane inflammation, rhinitis (often seasonal, allergic manifestations).
- Damp cough with mucus production (various admixtures of pus, blood may also be present)
- chronic cough associated with frequent heartburn (pyrosis)
- chronic cough with a sensation of mucus leaking from the sinuses (most often when falling asleep, at night)
- cough induced by a change of position, associated with coughing
Cough in smokers
- smokers develop coughs gradually, even over several years
- the patient may no longer even be aware of it
- often denies its presence when it is pointed out
- generally considers coughing to be a normal phenomenon
Myth: I'm sure I don't have a lung tumour because I don't cough up blood...
Read also
Prognosis of the disease
The prognosis of the disease depends on the histological type of the disease, the stage of the disease and the clinical condition of the patient and associated complications.
Unfortunately, lung cancer remains one of the most difficult to treat cancers with an unfavourable prognosis.
Smoking cessation remains useful in terms of regimen and limiting co-infections of the respiratory system.
Many smokers would quit immediately if they only once saw themselves choking and dying of lung cancer.
One effective anti-smoking campaign has been to place various images of cancers on cigarette packs.

How it is treated: Lung cancer
How is lung cancer treated: what are the treatment options and can it be cured?
Show moreLung cancer is treated by
Other names
Interesting resources










