- detskaonkologia.info
- linkos.cz - Leukemia in childhood
- solen.sk - Acute leukaemia - what a GP should know
- solen.cz - Bone marrow biopsy in myeloproliferative neoplasia - necessity or survival?
- solen.sk - Treatment of relapsed and refractory chronic lymphocytic leukemia
- solen.sk - New perspectives in cytogenetics and classification of childhood acute lymphoblastic leukemia
- solen.sk - Life after oncological treatment of paediatric patients
- Clinical Hematology. Sakalova et al., 2010
- Fundamentals of immunology, Hořejší and Bartůňková, 2009
- Medical physiology, Javorka et al., 2001
Leukemia: Why does it occur and what are its symptoms? + Diagnostics
What is leukaemia, why does it occur and how does it manifest itself? What is used in diagnosis and what is the treatment?
Most common symptoms
- Malaise
- Abdominal Pain
- Joint Pain
- Limb pain
- Fever
- Spirituality
- Depression - depressed mood
- Tinnitus
- Black stool
- Bone Pain
- Rash
- Blood in the power
- Bleeding gums
- Bleeding
- Sweating
- Indigestion
- Nausea
- Petechie
- Slow wound healing
- Stool with blood - blood in the stool
- Muscle weakness
- Head spinning
- Fatigue
- Vomiting blood
- Deterioration of vision
- Enlarged lymph nodes
- Liver enlargement
- Increased body temperature
Characteristics
Leukaemia is a blood cancer. What else is there to know, what causes it and what are the symptoms of leukaemia? What is the acute and chronic form? Can it be cured?
Theanswers to these and other questions can be found in the article.
Blood has been considered a symbol of life since ancient times.
Blood circulates throughout the body through the bloodstream and connects all the tissues of the body.
In literature, it is also called the "liquid organ".
It has an important and irreplaceable role. It carries oxygen, transports vital substances to the cells and excretes metabolic "wastes" to the various organs.
Diseases of the hematopoietic system therefore seriously damage the human body. How? Read on.
What is leukaemia?
In short: leukaemia is a cancer of the blood.
A malignant cancer of the hematopoietic system in the human body.
In 2020, 474,519 new cases of leukaemia were diagnosed worldwide in both sexes (WHO statistics).
The incidence of leukaemia in humans increases with age.
Characteristics of leukaemia
Leukaemia is caused by clonal proliferation of haematopoietic stem cells in the bone marrow.
There is an uncontrolled malignant (malignant) transformation of the so-called myeloid or lymphoid lineage of blood cells.
It can take both acute and chronic forms.
Accordingly, acute myeloblastic or lymphoblastic leukaemia or chronic myeloid or lymphocytic leukaemia can be distinguished.
Acute myeloblastic leukaemia occurs predominantly in adults. Acute lymphoblastic leukaemia predominates in children.
Leukaemic cells lose their ability to mature, called differentiation.
Immature malignant clones of blood cells do not have the same capabilities as healthy cells. Physiological haematopoiesis is suppressed.
The basis of malignant clones may be normal stem cells or malignantly transformed stem cells.
Immature cells are called blasts. They wash into the blood. They may form diffuse (scattered) or nodular (nodular) infiltrates in various organs, e.g. liver, spleen, lymph nodes, etc. This creates secondary foci.
This is a very heterogeneous disease. It is very important to identify the correct subtype of leukaemia so that patients can receive the most effective treatment in time.
Blood formation (haemopoiesis)
To further understand the nature of leukaemia, it is essential to know how blood formation works.
Blood formation is subject to complex mechanisms.
Proper blood cell development is important for the balance so that the bone marrow produces enough blood cells for the body.
When inflammation, injury or other disease occurs, the bone marrow responds flexibly and replenishes the blood cells. If the cause of increased production ceases, the increased blood production must be reduced to normal.
The beginning of blood cell development is based on a so-called pluripotent stem cell. A pluripotent stem cell conditions more than one cell type.
During a person's lifetime, a pluripotent stem cell is capable of unlimited self-renewal. After it divides, one of them remains a pluripotent cell and the other cell is destined to develop into a mature form of blood cell.
The whole process of maturation (differentiation) is complex. Different developmental forms of blood cells arise.
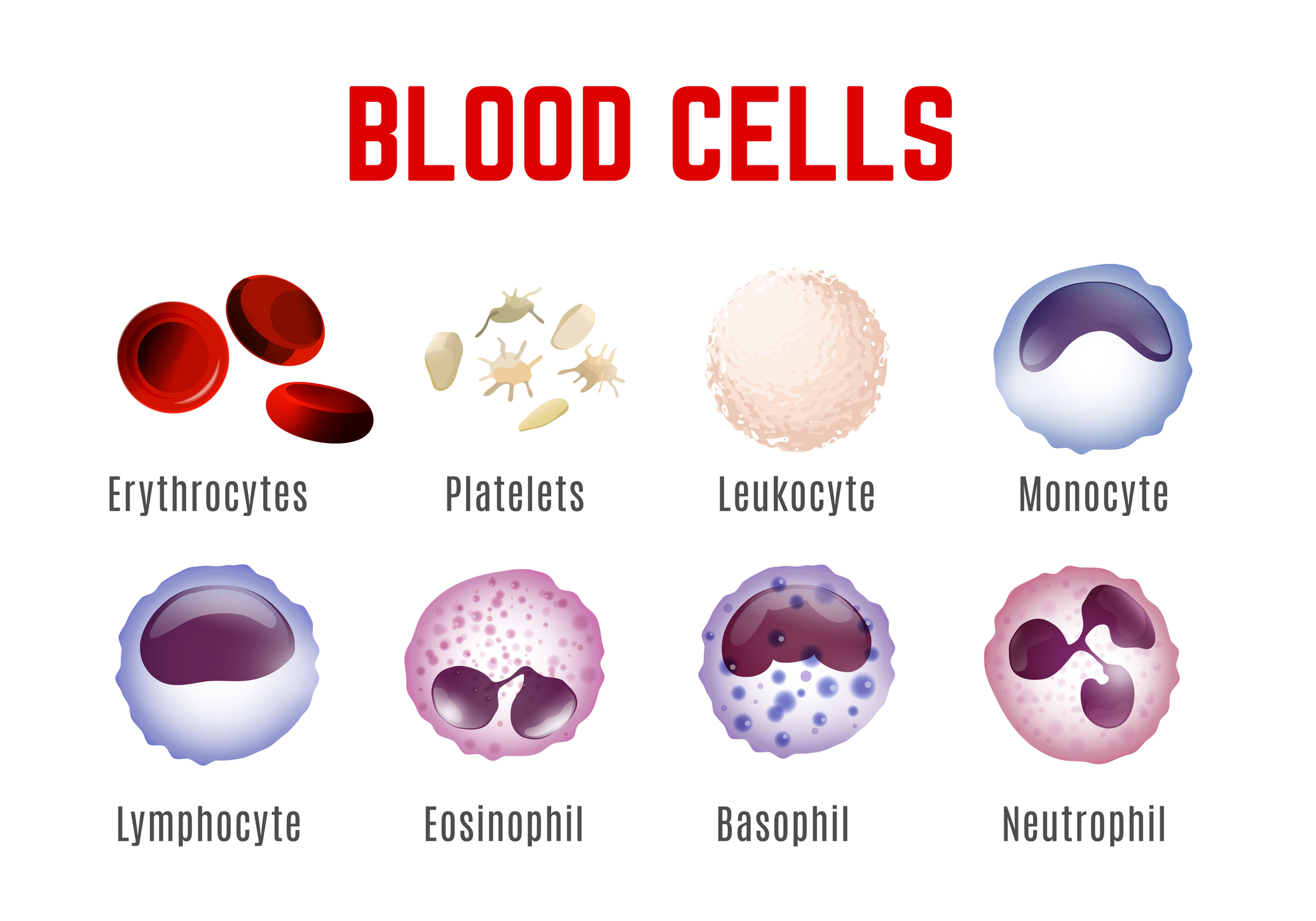
The myeloid lineage gives rise to monocytes, neutrophils, eosinophils, basophils, also dendritic cells, platelets and erythrocytes.
The lymphoid lineage produces T-lymphocytes, B-lymphocytes and NK cells.
A more detailed description and explanation of the different forms and immunological mechanisms is extensive. In this article, we will briefly explain the basic types of blood cells.
What basic blood cells do we know?
We distinguish between white blood cells (leukocytes), red blood cells (erythrocytes) and platelets (thrombocytes).
Erythrocytes are primarily responsible for the transport of blood gases (oxygen and carbon dioxide). The red blood pigment haemoglobin is a component of erythrocytes.
Leukocytes have an irreplaceable function in human immunity.
Platelets play a key role in the blood clotting process, promoting wound healing or inflammatory processes.
Where does blood formation take place? What is bone marrow?
Bone marrow is tissue that is found inside the bones. It has a jelly-like structure.
Blood formation takes place in the bone marrow.
Bone marrow is the "factory" for the production of blood cells.
Active red bone marrow is gradually replaced in the peripheral parts of the skeleton as we age. Fat cells infiltrate this marrow. This marrow is called inactive yellow marrow.
It is directly influenced by cells of the immune system and other tissues and organs. It is indirectly influenced by nervous and hormonal regulation.
Cytokines, which act as messengers in the body, have an important influence.
They transmit unique information between cells of the immune system and cells of other organs to target cells.
They have various biological functions:
- they can influence the maturation of blood cells
- play a role in the body's defences
- may influence cell proliferation
- influence the course of inflammation
Causes
The causes of leukemia are:
- genetic factors
- environmental influences (epigenetic factors)
- radiation, chemicals (dyes, organic solvents, fertilizers)
- drugs
- viruses
Symptoms
What symptoms can we expect?
- rapid fatigue, weakness
- Pallor
- shortness of breath even with slight exertion, exhaustion
- bleeding symptoms, increased tendency to bleed from the gums, nose, bruises (haematomas) all over the body of varying size, can be on the feet, nails, bleeding from organs etc.

Bleeding often occurs even with small injuries such as a simple scratch:
- Elevated temperature, fever (fever for several days may not be leukemia!)
- Increased tendency to infections
- Symptoms of infection are a common complication of leukemia. Infections often affect the urinary tract, lungs, skin, mucous membranes, etc.
- Symptoms of reduced blood flow (called hypoperfusion syndrome). Masses of leukaemic cells disrupt the microcirculation and blockage (occlusion) of blood vessels occurs. Damage to vital organs occurs. When the blood supply to the brain is impaired, speech, vision, mobility to varying degrees of consciousness and other disorders may occur.
- Venous thrombosis due to increased blood clotting
- Feeling of bloated abdomen, pressure, premature satiety, constipation. Often there is significant enlargement of the liver and/or spleen, called hepatosplenomegaly.
- Pain, often bony, in the chest wall area
- Manifestations associated with metabolic disturbances, mineral disorders, renal dysfunction. There is tumour breakdown of leukaemic cells.
- Weight loss
Weight loss in cancer is gradual, regular or rapid. Patients report that they often lose weight despite adequate dietary intake. Conversely, weight loss may be accompanied by lack of appetite and reduced food intake.

Diagnostics
The disease can be diagnosed incidentally during a routine examination. Sometimes the patient is brought to the doctor by clinical symptoms.
The basis is a general examination of the patient by a general practitioner.
During the examination, a complete blood count must be taken.
In the laboratory, the blood cells are also checked for abnormal changes, atypia and the presence of blasts.
In the laboratory, we look for changes in the number of white blood cells (leukocytes) - an increase in the number (called leukocytosis) or a decrease in the number (leukocytopenia). There may be anaemia (anaemia) or changes in the number of platelets (a lack of platelets is thrombocytopenia).
In chronic leukemias, we usually find extreme leukocytosis.
A marked increase in white blood cell count does not immediately indicate leukaemia.
There is a so-called leukemoid reaction - very high leukocyte counts e.g. in severe infections, pneumonia, blood poisoning, meningitis, burns, tumours, application of special drugs.
The patient should undergo a basic imaging examination - chest X-ray, abdominal ultrasound, possibly enlarged lymph nodes. He is then referred to a haematologist who manages the treatment.
A bone marrow biopsy is indicated, and often further imaging tests such as CT (computed tomography), MRI (magnetic resonance imaging) or PET-CT (positron emission tomography) and others.
Molecular genetic testing to categorise a more specific type of leukaemia is standard.
The examination may also include a diagnosis of lymphoma (in ALL). is performed for possible leukemic infiltration of the meninges.
Bone marrow biopsy (trepanobiopsy)
Don't be afraid of a bone marrow biopsy!
Preconceptions and lack of information make bone marrow biopsy an unnecessary "scarecrow".
It can be a step towards a very early diagnosis and life-saving surgery.
It provides unique information about the hematopoietic system!
There is no equivalent diagnostic mirror to this diagnostic method.
There's too much fear in our society. Fear often delays the procedure.
It makes a difference to the prognosis whether the disease is diagnosed early or only when leukaemic clones infest the body.
Bone marrow biopsy is an invasive procedure. In today's medicine, the risks are minimal.
It is only carried out by a specialist doctor who is qualified, experienced and specially trained.
During a biopsy, a sample of bone marrow tissue is obtained, which makes it possible to confirm a cancerous (malignant) process.
It determines the exact type of leukaemia, excludes reactive changes in the haematopoietic system that may mimic a malignant condition, shows morphological changes in the bone marrow, provides material for possible genetic analysis and allows specific treatment of the patient.
It is performed with a special long hollow needle from a specific site, usually the scapula of the hip or the sternum. It is taken under local anaesthesia.
A bone marrow puncture takes about 3 minutes, a bone marrow biopsy takes about 5 minutes.
Course
The course of the disease can be individual. It varies depending on whether it is acute leukaemia, chronic leukaemia or acute exacerbation (progression in chronic leukaemia).
The patient may have a set of multiple symptoms. The disease may progress from one symptom to another. The symptoms gradually increase.
In acute leukaemias, symptoms usually appear violently.
Untreated acute myeloblastic leukaemia has a rapid clinical course. It can cause death within days to months.
In many patients, initial symptoms last less than 3 months.
Acute myeloblastic leukaemia may be laboratory associated with cytopenia in the pre-leukaemia syndrome years before overt leukaemia becomes apparent.
Cytopenia in the blood count indicates fewer blood cells, e.g. anaemia.
Manifestations in chronic leukaemias may be very subtle at the outset or there may be no symptoms.
In chronic leukaemias, the so-called chronic phase may last for several years without symptoms. It may be detected incidentally or occur during the transformation phase into a more aggressive form.
In leukaemia you will encounter the following terms.
Disease remission is a condition where the tumour is suppressed by treatment.
There may be partial suppression and this is called partial remission. There may be complete suppression and complete remission.
Relapse means that after the initial removal or reduction of tumour growth, the disease has reactivated.
Disease progression refers to the growth, enlargement and progression of the tumour.
Graft versus host disease is a graft versus host reaction during transplantation.
Leukaemia in children
Leukemia is the most common malignancy in childhood.
Treatment and prognosis have radically improved thanks to intensive research.
The most common type of leukaemia in children is acute lymphoblastic leukaemia (ALL).
It accounts for approximately 80% of cases. The highest incidence is between the ages of 2 and 5.
ALL in children differs in biological behaviour compared to adults.
Acute myeloblastic leukaemia (AML) has a poorer prognosis compared to ALL. It accounts for a minority of cases.
Chronic leukemias in childhood are less common.
An increased risk of childhood leukemias has been described in association with X-rays during maternal pregnancy and also approximately 5-10 years after cytostatic treatment for other malignancies.
A higher incidence of leukaemia has also been reported in congenital genetic disorders, e.g. Down syndrome has a 56-fold increased risk of leukaemia by 4 years of age.
In most cases, the exact causative factor is unknown.
Cytogenetic testing often reveals mutations that have accumulated in cells and caused leukaemia.
Symptoms of leukaemia in children
- Elevated temperature to fever, signs of infection, unresponsive to commonly available drugs that control the elevated temperature
- Children are lethargic, sleepy
- Hemorrhagic manifestations (mentioned above)
- Pain on walking, limping (infiltrated bone marrow)
Child may even refuse to walk.
- Pressure, pain in the abdomen when the liver, spleen and/or lymph nodes are enlarged
- Laboratory findings may be initially without significant changes, may not contain leukemic cells
- Mild anemia, slight decrease in white blood cells and platelets, but gradual development of changes over time
- Decreased white blood cell loss is seen more often than an increase in leukocytes
- Other symptoms described above
Treatment in children
Treatment in children is a challenging process and requires a top-notch team of many specialists.
The mainstay of treatment is chemotherapy. Radiation (radiotherapy) and surgery are used in the treatment of only some patients. Initially, intensive treatment is given, later maintenance treatment. The duration of this treatment is approximately two years.
Targeted therapy is the subject of clinical trials. Its use is possible in certain indications, e.g. in ALL with detection of a Philadelphia chromosome mutation.
In children where remission lasts more than five years, leukaemia rarely returns. But it is not completely excluded. In these children, there is essentially a cure.
After cancer treatment, it remains important to keep patients well informed about their health status, follow-up options and intervals, and the prevention or treatment of late sequelae.
Follow-up of the young patient after reaching adulthood passes from the hands of the paediatric oncologist to the adult oncologist. Good cooperation is essential.
A specialised team offers a wide range of assistance. If necessary, they even come to the patient's home and administer treatment.
Prognosis of leukaemia
The prognosis of patients with leukaemia varies mainly depending on the type of leukaemia, early or late diagnosis, response to first-line treatment, quality and duration of treatment response, age, patient comorbidities and associated complications, as well as prognostic factors, the most important of which are cytogenetic abnormalities.
Different types of leukaemias may have different prognoses in adults and children (e.g. ALL).
Blood donation
Donating is the most beautiful thing a person can do....
Why donate blood?
Your blood can save someone's life.
In particular, patients with leukemia or other cancers have severe bleeding symptoms associated with this insidious disease and are referred for help.
After a blood transfusion, they are able to breathe properly and fight again.
Maybe one day you too will need help...
Help and donate a drop of blood...

How it is treated: Leukemia
Treatment of leukaemia
Show moreLeukemia is treated by
Other names
Interesting resources
Related










